Abstract
Trauma is the leading cause of death in young people with a considerable socio-economic impact worldwide. A trimodal distribution of trauma mortality was described in the past, but recently different studies underlined a progressive change in trauma mortality distribution linked to improvement in trauma care. This study aimed to analyze the mortality trends in a Level-One Trauma Center in Italy. Data on 6065 patients consecutively admitted to the Trauma Center between 2011 and 2020 were selected and retrospectively analyzed. Causes of Death (CODs) and time of death were stratified in four main groups and the patient sample was further divided into five age groups. Multivariate regression models were then performed to identify independent predictors of mortality. The most common COD in all age groups was Central Nervous System injuries. Immediate deaths (in ED) affected mostly patients over 75 years of age (34.3%). Deaths caused by massive hemorrhage occurred soon upon arrival in the ED, whereas deaths due to other causes (e.g. sepsis, MOF) after the first week. Patients’ characteristics, the need for emergency procedures and high trauma severity scores were independent predictors of deaths. This study represented the first analysis on trauma mortality distribution in Italy over a nine-year period. The trimodal distribution described in the past seems to be no longer present in Italy, due to improvements in trauma systems and critical care. However, the high number of immediate and acute deaths underlies a persisting need for efforts in injury prevention and control .
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma is the first cause of death in younger people worldwide [1]. In 1983, Trunkey D [2] described a trimodal distribution of death in trauma patients. The first peak represented the immediate deaths, occurring within the first hour after trauma, accounting for 45% of all deaths, mostly due to non-survivable hemorrhagic or central nervous system injuries [2]. Early deaths, occurring within 1–4 h after trauma, represented the second peak and accounted for about 34% of deaths [3], mostly caused by uncontrolled hemorrhagic injuries or expanding intracerebral hematomas. If these injuries are promptly recognized and treated, early deaths can be prevented: therefore these deaths have also been defined as preventable trauma deaths [4]. The third peak occurred more than a week after trauma and accounted for about 20% of all deaths, defined as late deaths [3]. Most of these deaths were attributed to sepsis and multiple organ failure (MOF) [4].
The concept of a trimodal distribution of death in trauma played an important role in the development of trauma systems. The development of damage control techniques, specific guidelines in massive transfusion protocols, and the implementation of modern technologies in intensive care has decreased the mortality of trauma patients [5, 6], leading to a bimodal distribution of trauma mortality [7, 8]. The increase in the age of the trauma population, as well as the presence of comorbidities and the predominance of some mechanisms of injury (MOIs), contributed to the change in the epidemiology of trauma related deaths over the past decade [9,10,11].
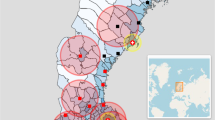
Different authors investigated the role of MOI, cause of death (COD), and time of death [7, 8] on the distribution of mortality as the relationship between these factors could be relevant in the assessment of the effectiveness of a trauma system. The aim of this study was to investigate the mortality distribution in a high-flow Level One Trauma Center in Italy over a nine-year period. To our knowledge, this is the first study that describes the distribution of trauma deaths and the effect of the introduction of a mature trauma system in Italy.
Methods
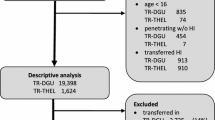
All major trauma managed in Niguarda Trauma Center were prospectively collected in Niguarda trauma registry from 2011 to 2020. The institution of the trauma registry for all major trauma admitted to the hospital was approved by Niguarda Ethical Committee Milano Area 3 (record number 534–102,018). Accordingly, no personal data of patients are disclosed in the present study. The registry is held by a Trauma Team consultant who is meant to keep it constantly updated, and it is annually revised by the head of the department. Demographic data, time of trauma, vital parameters (heart rate, respiratory rate, systolic blood pressure, Glasgow Coma Scale (GCS), MOI, emergency procedures performed in the emergency department (ED), need of emergency surgery, need of orotracheal intubation (IOT), and injuries sustained by the patients were extracted from the registry. The abbreviated injury scale (AIS, 1998 version) of each anatomical region, Injury Severity Score (ISS), Revised Trauma Score (RTS), probability of survival (PS) obtained by the Revised Trauma and Injury Severity Score (TRISS) system, and observed survival were retrospectively analyzed to estimate the severity of the trauma. The American Society of Anesthesiologists (ASA) physical status classification was chosen to summarize comorbidities. Patients were divided into five age groups: pediatric age (0–13 years), young adults (14–39 years old), adults (40–64 years old), elder adults (65–75 years old) and elderly (> 75 years old). Patients with ISS ≥ 16 were considered severely injured.
CODs were classified as follows:
-
Central Nervous System (CNS): predominantly lethal injury of brain, brain stem, and high cervical spine.
-
Massive hemorrhage (HEM): hemorrhage, predominantly from uncontrolled bleeding “clinically visualised or otherwise documented (disruption of large vessels or parenchymatous organ leading to complete loss of blood volume, or hypovolemic cardiac arrest)” [12].
-
CNS + HEM: combination of the previous two.
-
Other: MOF, ARDS, other injuries or secondary complications (pulmonary embolism, sepsis, myocardial infarction).
Deceased patients were also stratified over four groups based on the time of death:
-
Immediate: patients deceased early after admission in the ED to whom no patient ID number was assigned;
-
Acute: death within 24 h from access in the ED;
-
Early: death after 24 h but within 7 days;
-
Late: demise of the patient after 7 days from arrival in the ED
The data were recorded in a computerized spreadsheet (Microsoft Excel 2016, Microsoft Corporation, Redmond, WA) and analyzed with statistical software (IBM Corp. Released 2012, IBM SPSS Statistics for Windows, version21.0, Armonk, NY, IBM Corp.). Graphics were also obtained with R coding. The sample distribution was evaluated with Kolmogorov–Smirnov and Shapiro–Wilk tests, resulting in a non-Gaussian distribution for any of the examined variables. Continuous data were compared by independent sample Kruskar–Wallis test, and categorical data using Pearson’s chi-square test. P values below 0.05 were considered statistically significant, and included in the multivariate logistic regression model. Survival curves were obtained with Kaplan–Meier analysis, and log-rank test was assessed to evaluate differences in cumulative survival among age groups. Bivariate logistic regression was used to provide odds ratio for individual variables, identifying possible predictors of mortality. After computing the variance inflation factor (VIF), showing no collinearity, three different multivariate regression models were built: one for general variables (age, in-hospital vital parameters), another one for the pre-hospital and in-hospital maneuvers and surgeries performed and the last one for the injury’s severity indicators (AIS’98, ISS, TRISS) to detect independent risk factors for death and to estimate the adjusted odds ratio (OR) and 95% confidence interval (CI).
Results
During the study period, of the 6065 patients who fulfilled the inclusion criteria, 316 (5.21%) died. Table 1 resumes the univariate and multivariate analysis among the general population. Significant variables which correlated with mortality using bivariate logistic regression analysis were Age, ASA score, SBP, DBP, GCS, RTS, BE levels, extra-peritoneal packing (EPP), damage control laparotomy (DCL) and thoracotomy (DCT), thoracic drain placement, need of emergency surgery and IOT, ISS and TRISS.
Table 2 resumes the COD according to the mechanism of trauma and intent among the 316 deceased patients. Deaths in motorcycle and motor vehicle collisions were mostly caused by CNS (45.5% and 44.7% respectively) and HEM (34.1% and 23.7%). Deaths in accidental falls were related to CNS in 73.3% of cases, and CNS + HEM in 15.6% of cases. The highest ratio of death due to ‘other’ causes was found in bicycle related injuries (18%, two third of which were elderly). Most deceased cyclists (n = 14.42%) were over 75 years of age. The most common COD in all age groups was CNS. ‘Other’ causes of death were found in almost 14% of elderly (> 75) and in lower ratios in the other age groups. Among those who died of ‘other’ causes, only one patient had less than 41 years of age.
However, head AIS was not found to be predictor of death at the multivariate analysis. Deaths due to a combination of CNS HEM occurred in patients with higher ISS and at a younger age.
Table 3 resumes the time of death in the different age groups. Immediate deaths (in ED) affected mostly patients over 75 years of age (34.3%). Table 4 describes the time of death in the different COD groups. Deaths caused by massive hemorrhage occurred soon upon arrival in the ED, whereas deaths due to ‘Other’ causes occurred later in time, after the first week (Fig. 2).
The survival rate computed with Kaplan–Meier method was 98.1% in patients younger than 13 years of age. In patients between 14 and 39 years it was 97.6%, 95.1% in patients between 40 and 64 years, 89.9% in patients between 65 and 75 years and 75% in patients over 75 years of age (log-rank test, p < 0.001). Survival curves among the different age groups are reported in Fig. 1.
Discussion
Our study represented the first analysis on trauma mortality distribution in Italy over a nine-year period. The classic trimodal distribution of trauma mortality, previously described in literature, was no longer present. Improvements in trauma systems and critical care changed the distribution of mortality, with most deaths occurring within the first hour and an important decrease in the number of late deaths: patients who survived the first hours were more likely to survive. The persisting elevated number of immediate and acute deaths underlined the need for further efforts in injury prevention and control. In a mature trauma system immediate and acute deaths affected principally patients unlikely to survive due to the severity of the injuries who arrived alive in the ED because of the efficiency of the pre-hospital care.
Multivariate logistic regression (Table 1) showed that patient characteristics (such as age, ASA score and vital parameters), the need for Damage Control procedures (EPP, DCT, thoracic drain placement, emergency surgery etc.) and trauma severity scores (ISS, death probability TRISS, RTS), were independent predictors of mortality. Therefore, mortality seemed to be related to different factors, with a different impact according to the timing of treatment. Kaplan Mayer analysis (Fig. 1) showed that mortality was higher in patients older than 75 years old with a greater incidence of immediate and acute deaths, thus confirming the impact of age on mortality. These results were in line with recent international literature [7, 13]. However, Table 1 shows how variables often associated with an increased mortality (such as emergency surgery needing or ISS > 16) were not independent predictors of mortality. In our study, “emergency surgery” included any emergency procedure performed in the operating room immediately after the patient arrival. Therefore, also non-life-saving procedure (as orthopedics or plastic procedures) are included in this definition. This can explain how this variable was not a predictor of mortality. Concerning the ISS > 16, this study was conducted in a high-flow trauma center with a specialized trauma team consisting of surgeons, anesthesiologist, and radiologist immediately available at the trauma arrivals. It is therefore possible that these data represent the protective effect of an experienced trauma team in reducing mortality in seriously injuries patients.
Figure 1, 2, shows a decreasing in mortality over the time with a clear decrease of trauma mortality in late deaths. Decrease in late deaths could be ascribed to two main reasons: (a) the efficacy of damage control surgery and resuscitation in the acute phase [14], with early use of blood products, application of massive transfusion protocols [5] and on the minimization of crystalloid resuscitation [15]; (b) improvement in intensive care treatment and artificial support which allowed for an increased survival of sick patients. Late deaths, occurring days to weeks after trauma, were mainly related to hypovolemic shock and massive crystalloid resuscitation, resulting in ischemia–reperfusion mechanism with cellular damage and multiple organ disfunction (such as cardiac failure, acute renal failure, acute respiratory distress syndrome, infection and sepsis) [16, 17]
Table 2 shows the mortality distribution according to the MOI and intent. Falls represented the first cause of death, followed by pedestrian struck and motorcycle accidents, with CNS injuries as the first cause of mortality in these groups. Lansink et al. [18] analyzed the trauma distribution in a Level One Trauma Center in Germany, showing a great incidence of blunt trauma, with CNS injuries as a main COD, but HEM playing a major during the first hour after trauma. These results diverged from North American reports where HEM is the first COD in all stages, as the main MOI are gunshot wounds (GSW) and stab wounds (SW) [19].
In contrast with North American Literature [7, 20], GSW and SW represented a minor cause of death in our sample: penetrating injuries represented only approximately 8% of all injuries, and most GSWs were self-inflicted in male patients > 40 years of age. These results were in line with the overall trauma trends, as the incidence of this type of MOIs is higher in North America than in Europe [11, 20]. Our study was conducted in a high-flow Level One trauma center and showed, for the first time in Italy, the potential role of a specialized and trained Trauma Team in reducing mortality. The reduction in mortality is mainly linked to HEM through the damage control maneuvers performed in emergency room. Indeed, in the first hours upon arrivals, CSM represented the main cause of death.
Some limitations must be considered when interpreting the results present in this study. First of all, only intra-hospital data were analyzed, thus not providing information on pre-hospital mortality. The development of a mature trauma system, especially in the urban area, led to a “scoop and run” approach in the pre-hospital setting. Therefore, it is possible that many of the patients who would have previously been declared dead on the scene were transported to the hospital, increasing the number of immediate deaths in the ED due to non-survivable injuries, such as severe CNS injuries. Further studies are needed to confirm this finding.
In addition, the study was a retrospective analysis of a nine-year cohort of trauma patients transported and treated in a level one trauma center: a high-flow trauma center with a surgical leadership in trauma management and a staff specifically trained on trauma management and damage-control procedures [11, 21]. Although it represented the first Italian report on the topic, it cannot reflect the overall mortality distribution of trauma patients in all the country, as there are differences in trauma management according to the center. Further multi-center studies should be carried out to confirm these results.
Conclusions
This study confirms that the trimodal distribution of trauma mortality is no longer present in Italy. Advances in trauma management, development of evidence-based protocols for acute care of injuries, multidisciplinary care of the injured and primary social measure for trauma prevention probably contributed to the changes in the observed distribution of trauma mortality. Moreover, this study showed a significant difference in mortality distribution in Italy with a higher incidence of blunt road traffic trauma and CNS injuries as main COD comparing with North American literature. Further multi-center studies also including the pre-hospital data should be carried out to confirm and expand our results.
References
Park Y, Lee GJ, Lee MA, Choi KK, Gwak J, Hyun SY et al (2021) Major causes of preventable death in trauma patients. J Trauma Inj. https://doi.org/10.20408/jti.2020.0074
Trunkey DD (1983) Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am 249(2):28–35
Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C et al (2005) Trauma deaths in a mature Urban trauma system: is “Trimodal” distribution a valid concept? J Am Coll Surg 201(3):343–348. https://doi.org/10.1016/j.jamcollsurg.2005.05.003
Bansal V, Fortlage D, Lee JG, Costantini T, Potenza B, Coimbra R (2009) Hemorrhage is more prevalent than brain injury in early trauma deaths: the golden six hours. Eur J Trauma Emerg Surg 5(1):26–30. https://doi.org/10.1007/s00068-008-8080-2
Cornero SG, Maegele M, Lefering R, Abbati C, Gupta S, Sammartano F et al (2020) predictive factors for massive transfusion in trauma: a novel clinical score from an Italian trauma center and German trauma registry. J Clin Med 9(10):3235. https://doi.org/10.3390/jcm9103235
Meyer DE, Vincent LE, Fox EE, O’Keeffe T, Inaba K, Bulger E et al (2017) Every minute counts: time to delivery of initial massive transfusion cooler and its impact on mortality. J Trauma Acute Care Surg 83(1):19–24. https://doi.org/10.1097/TA.0000000000001531
Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S (2010) Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med) Cent 23(4):349–354
Abdelrahman H, El-Menyar A, Al-Thani H, Consunji R, Zarour A, Peralta R et al (2014) Time-based trauma-related mortality patterns in a newly created trauma system. World J Surg 38(11):2804–2812. https://doi.org/10.1007/s00268-014-2705-x
Atinga A, Shekkeris A, Fertleman M, Batrick N, Kashef E, Dick E (2018) Trauma in the elderly patient. Br J Radiol 91(1087):20170739. https://doi.org/10.1259/bjr.20170739
Jacobs DG, Plaisier BR, Barie PS, Hammond JS, Holevar MR, Sinclair KE et al (2003) Practice management guidelines for geriatric trauma: The EAST practice management guidelines work group. J Trauma 54(2):391–416. https://doi.org/10.1097/01.TA.0000042015.54022.BE
Difino M, Bini R, Reitano E, Faccincani R, Sammartano F, Briani L et al (2021) Epidemiology of trauma admissions in a level 1 trauma center in Northern Italy: a nine-year study. Updat Surg 73(5):1963–1973. https://doi.org/10.1007/s13304-021-00991-y
Irita K (2011) Risk and crisis management in intraoperative hemorrhage: human factors in hemorrhagic critical events. Korean J Anesthesiol 60(3):151. https://doi.org/10.4097/kjae.2011.60.3.151
Rauf R, von Matthey F, Croenlein M, Zyskowski M, van Griensven M, Biberthaler P et al (2019) Changes in the temporal distribution of in-hospital mortality in severely injured patients—an analysis of the traumaregister DGU. PLoS ONE 14(2):e0212095. https://doi.org/10.1371/journal.pone.0212095
Frassini S, Gupta S, Granieri S, Cimbanassi S, Sammartano F, Scalea TM et al (2020) Extraperitoneal packing in unstable blunt pelvic trauma: A single-center study. J Trauma Acute Care Surg 88(5):597–606. https://doi.org/10.1097/TA.0000000000002618
Watters JM, Tieu BH, Todd SR, Jackson T, Muller PJ, Malinoski D et al (2006) Fluid resuscitation increases inflammatory gene transcription after traumatic injury background: the debate continues. J Trauma 61(2):300–308. https://doi.org/10.1097/01.ta.0000224211.36154.44 (PMID: 16917442)
Cotton BA, Guy JS, Morris JA, Abumrad NN (2006) The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock 26(2):115–121. https://doi.org/10.1097/01.shk.0000209564.84822.f2
Mizobata Y (2017) Damage control resuscitation: a practical approach for severely hemorrhagic patients and its effects on trauma surgery. J intensive care 5(1):4. https://doi.org/10.1186/s40560-016-0197-5
Sakran JV, Mehta A, Fransman R, Nathens AB, Joseph B, Kent A et al (2018) Nationwide trends in mortality following penetrating trauma: are we up for the challenge? J Trauma Acute Care Surg 85(1):160–166. https://doi.org/10.1097/TA.0000000000001907
Lansink KWW, Gunning AC, Spijkers ATE, Leenen LPH (2013) Evaluation of trauma care in a mature level I trauma center in the Netherlands: outcomes in a Dutch mature level I trauma center. World J Surg 37(10):2353–2359. https://doi.org/10.1007/s00268-013-2103-9
Kauvar DS, Lefering R, Wade CE (2006) Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma 60(6 Suppl):S3-11. https://doi.org/10.1097/01.ta.0000199961.02677.19
Reitano E, Granieri S, Frassini S, Sammartano F, Cimbanassi S, Chiara O (2021) Infectious complications of extra-peritoneal pelvic packing in emergency room. Updates Surg 73(1):331–337. https://doi.org/10.1007/s13304-020-00856-w
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ER and MD, performed the statistical analysis, and drafted the manuscript. RB and OC designed the study, critically reviewed, and supervised the manuscript. MD provided English revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Research involving human participants and/or animals
This study was conducted in conformity to the principles declared to the National Commission for Data Protection and Liberties (CNIL: 2210699) and in accordance with the ethical principles described in the Declaration of Helsinki.
Informed consent
All patients or the next kind person signed an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reitano, E., Bini, R., Difino, M. et al. Nine year in-hospital mortality trends in a high-flow level one trauma center in Italy. Updates Surg 74, 1445–1451 (2022). https://doi.org/10.1007/s13304-022-01303-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01303-8