Abstract
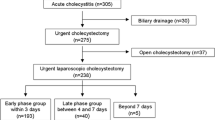
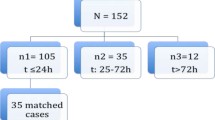
Laparoscopic cholecystectomy (LC) is a common surgical procedure in acute cholecystitis (AC). Patients often suffer from considerable postoperative pain and indigestion, which prolongs in-hospital stay. The enhanced recovery after surgery (ERAS) program has proven its efficacy in elective surgery and could hypothetically improve outcomes of emergency LC. Currently, there is no ERAS program for LC in patients with AC. A modified ERAS (mERAS) protocol was studied in a prospective, randomized non-blinded clinical trial (NCT03754751). The mERAS group consisted of 88 patients the control group of 101 patients. The modified protocol included a patient information brochure; minimizing drain use; local anesthesia; low-pressure pneumoperitoneum; PONV prophylaxis, early mobilization and oral diet. The primary outcome was postoperative length of stay (pLOS). The postoperative length of stay in the mERAS group was shorter (24 (21–45.5) h) than in the control (45 (41–68) h) (p < 0.0001). One re-admission in the mERAS group was reported (p = 0.466). There difference in complications was insignificant (mERAS 6.8% vs 5% p = 0.757). Post-operative pain intensity was significantly lower in the mERAS group immediately after awaking (3.7 ± 1.8 vs 5.4 ± 1.3 p < 0.0001), 2 h (3.3 ± 1.7 vs 4.9 ± 1.6 p = 0.0006), 6 h (2.9 ± 1.5 vs 4.2 ± 1.2 p < 0.0001), 12 h (2.7 ± 0.9 vs 4.1 ± 1.2 p = 0.0001) and 24 h after surgery (2.1 ± 1.2 vs 3 ± 1.2 p < 0.0001). The incidence of shoulder and neck pain was lower in mERAS group (13.6% vs 34.7% p = 0.0009). Peristalsis recovery was similar in both groups. The proposed protocol improved postoperative recovery and reduced hospital stay in patients with AC without increasing the rate of complications or re-admissions.

Similar content being viewed by others
Availability of data and materials
Data used to support the findings of this study are available from the corresponding author upon reasonable request.
References
Stinton LM, Shaffer EA (2012) Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 6:172–187
Ansaloni L, Pisano M, Coccolini F et al (2016) 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. https://doi.org/10.1186/s13017-016-0082-5
Shaffer EA (2005) Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep 7:132–140
Wang H, Naghavi M, Allen C et al (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1459–1544. https://doi.org/10.1016/S0140-6736(16)31012-1
Koti RS, Davidson CJ, Davidson BR (2015) Surgical management of acute cholecystitis. Langenbeck’s Arch Surg 400:403–419. https://doi.org/10.1007/s00423-015-1306-y
Borzellino G, Khuri S, Pisano M et al (2020) Timing of early laparoscopic cholecystectomy for acute calculous cholecystitis revised: protocol of a systematic review and meta-analysis of results. World J Emerg Surg 15:1. https://doi.org/10.1186/s13017-019-0285-7
Murphy MM, Ng SC, Simons JP et al (2010) Predictors of major complications after laparoscopic cholecystectomy: surgeon, hospital, or patient? J Am Coll Surg 211:73–80. https://doi.org/10.1016/j.jamcollsurg.2010.02.050
Kamalapurkar D, Pang TCY, Siriwardhane M et al (2015) Index cholecystectomy in grade II and III acute calculous cholecystitis is feasible and safe. ANZ J Surg 85:854–859. https://doi.org/10.1111/ans.12986
Vaccari S, Cervellera M, Lauro A et al (2020) Laparoscopic cholecystectomy: which predicting factors of conversion? Two Italian center’s study. Minerva Chir. https://doi.org/10.23736/S0026-4733.20.08228-0
Duca S, Bãlã O, Al-Hajjar N et al (2003) Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB 5:152–158. https://doi.org/10.1080/13651820310015293
Terho PM, Leppäniemi AK, Mentula PJ (2016) Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World J Emerg Surg 11:54. https://doi.org/10.1186/s13017-016-0111-4
Isazadehfar K, Entezariasl M, Shahbazzadegan B et al (2017) The comparative study of ondansetron and metoclopramide effects in reducing nausea and vomiting after laparoscopic cholecystectomy. Acta Med Iran 55:254–258
Salman N, Aykut A, Sabuncu Ü et al (2020) Dextrose administration may reduce the incidence of postoperative nausea and vomiting after laporoscopic cholecystectomy: a double blind randomized controlled trial. Minerva Anestesiol. https://doi.org/10.23736/S0375-9393.20.13484-9
Zhou C, Zhu Y, Liu Z, Ruan L (2016) 5HT3 antagonists versus dexamethasone in the prevention of PONV in patients undergoing laparoscopic cholecystectomy: a meta-analysis of RCTs. Biomed Res Int 2016:8603409. https://doi.org/10.1155/2016/8603409
Ko-Iam W, Sandhu T, Paiboonworachat S et al (2017) Predictive factors for a long hospital stay in patients undergoing laparoscopic cholecystectomy. Int J Hepatol. https://doi.org/10.1155/2017/5497936
Barazanchi AWH, MacFater WS, Rahiri JL et al (2018) Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth 121:787–803
Loizides S, Gurusamy KS, Nagendran M et al (2014) Wound infiltration with local anaesthetic agents for laparoscopic cholecystectomy. Cochrane Database Syst. Rev. 2014:CD007049
Brown JK, Singh K, Dumitru R et al (2018) The benefits of enhanced recovery after surgery programs and their application in cardiothoracic surgery. Methodist Debakey Cardiovasc J 14:77–88
Brustia P, Renghi A, Gramaglia L et al (2003) Mininvasive abdominal aortic surgery. Early recovery and reduced hospitalization after multidisciplinary approach. J Cardiovasc Surg 44:629–635
Garcés-Albir M, Martín-Gorgojo V, Perdomo R et al (2019) Acute cholecystitis in elderly and high-risk surgical patients: is percutaneous cholecystostomy preferable to emergency cholecystectomy? J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04424-5
Trevino CM, Katchko KM, Verhaalen AL et al (2016) Cost effectiveness of a fast-track protocol for urgent laparoscopic cholecystectomies and appendectomies. World J Surg 40:856–862. https://doi.org/10.1007/s00268-015-3266-3
Scott MJ, Baldini G, Fearon KCH et al (2015) Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 59:1212–1231
Paduraru M, Ponchietti L, Casas IM et al (2017) Enhanced recovery after emergency surgery: a systematic review. Bull Emerg Trauma 5:70–78
Hamill JK, Rahiri JL, Gunaratna G, Hill AG (2017) Interventions to optimize recovery after laparoscopic appendectomy: a scoping review. Surg Endosc 31:2357–2365. https://doi.org/10.1007/s00464-016-5274-2
Takada T, Strasberg SM, Solomkin JS et al (2013) TG13: updated Tokyo guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:1–7. https://doi.org/10.1007/s00534-012-0566-y
Nechay T, Sazhin A, Titkova S et al (2020) Evaluation of enhanced recovery after surgery program components implemented in laparoscopic appendectomy: prospective randomized clinical study. Sci Rep. https://doi.org/10.1038/s41598-020-67591-5
Hefermehl LJ, Largo RA, Hermanns T et al (2014) Lateral temperature spread of monopolar, bipolar and ultrasonic instruments for robot-assisted laparoscopic surgery. BJU Int 114:245–252. https://doi.org/10.1111/bju.12498
Clavien PA, Barkun J, De Oliveira ML et al (2009) The clavien-dindo classification of surgical complications: Five-year experience. Ann Surg 250:187–196
Зaтeвaxин ИИ, Caжин AB, Киpиeнкo AИ et al (2020) Диaгнocтичecкиe и лeчeбныe пoдxoды пpи ocтpoм aппeндицитe в пpaктикe xиpypгoв Poccийcкoй Фeдepaции. Peзyльтaты oбщepoccийcкoгo oпpoca. Xиpypгия им HИПиpoгoвa No 8:5–16
Hamill JK, Rahiri J-L, Gunaratna G, Hill AG (2017) Interventions to optimize recovery after laparoscopic appendectomy: a scoping review and other interventional techniques. Surg Endosc. https://doi.org/10.1007/s00464-016-5274-2
Wisely JC, Barclay KL (2016) Effects of an enhanced recovery after surgery programme on emergency surgical patients. ANZ J Surg 86:883–888. https://doi.org/10.1111/ans.13465
Gurusamy KS et al (2014) Methods of intraperitoneal local anaesthetic instillation for laparoscopic cholecystectomy (review). Summary of findings for the main comparison. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009060.pub2
Boddy A, Mehta S, Rhodes M (2006) The effect of intraperitoneal local anesthesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Anesth Analg 103:682–688. https://doi.org/10.1213/01.ane.0000226268.06279.5a
Gurusamy KS, Vaughan J, Davidson BR (2014) Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2014(3):CD006930. https://doi.org/10.1002/14651858.CD006930.pub3
Bajracharya JL, Subedi A, Pokharel K, Bhattarai B (2019) The effect of intraoperative lidocaine versus esmolol infusion on postoperative analgesia in laparoscopic cholecystectomy: a randomized clinical trial. BMC Anesthesiol 19:198. https://doi.org/10.1186/s12871-019-0874-8
Khandelwal H, Parag K, Singh A et al (2019) Comparison of subcostal transversus abdominis block with intraperitoneal instillation of levobupivacaine for pain relief after laparoscopic cholecystectomy: a prospective study. Anesth Essays Res 13:144–148. https://doi.org/10.4103/aer.AER_3_19
Matsuzaki S, Vernis L, Bonnin M et al (2017) Effects of low intraperitoneal pressure and a warmed, humidified carbon dioxide gas in laparoscopic surgery: a randomized clinical trial. Sci Rep. https://doi.org/10.1038/s41598-017-10769-1
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery a review. JAMA Surg 152:292–298
Xu D, Zhu X, Xu Y, Zhang L (2017) Shortened preoperative fasting for prevention of complications associated with laparoscopic cholecystectomy: a meta-analysis. J Int Med Res 45:22–37. https://doi.org/10.1177/0300060516676411
Çetinkaya F (2019) The effects of listening to music on the postoperative nausea and vomiting. Complement Ther Clin Pract 35:278–283. https://doi.org/10.1016/j.ctcp.2019.03.003
Hossain MM, Begum M, Hossain M et al (2019) Efficacy of palonosetron as antiemetic prophylaxis for post operative patients. Mymensingh Med J 28:222–229
Gustafsson UO, Scott MJ, Schwenk W et al (2012) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr 31:783–800. https://doi.org/10.1016/j.clnu.2012.08.013
Shah JN, Maharjan SB, Manandhar K (2012) Early feeding and discontinuation of intravenous fluid after laparoscopic cholecystectomy. J Nepal Health Res Council 10:28–31
Cestonaro T, Madalozzo Schieferdecker ME, Daniela Thieme R et al (2014) The reality of the surgical fasting time in the era of the ERAS protocol. Nutr Hosp 29:437–443. https://doi.org/10.3305/nh.2014.29.2.7025
De Aguilar-Nascimento JE, Leal FS, Dantas DCS et al (2014) Preoperative education in cholecystectomy in the context of a multimodal protocol of perioperative care: a randomized, controlled trial. World J Surg 38:357–362. https://doi.org/10.1007/s00268-013-2255-7
Kleif J, Vilandt J, Gögenur I (2016) Recovery and convalescence after laparoscopic surgery for appendicitis: a longitudinal cohort study. J Surg Res 205:407–418. https://doi.org/10.1016/j.jss.2016.06.083
Yeh A, Butler G, Strotmeyer S et al (2020) ERAS protocol for pediatric laparoscopic cholecystectomy promotes safe and early discharge. J Pediatr Surg 55:96–100. https://doi.org/10.1016/j.jpedsurg.2019.09.053
Pucher PH, Brunt LM, Davies N et al (2018) Outcome trends and safety measures after 30 years of laparoscopic cholecystectomy: a systematic review and pooled data analysis. Surg Endosc 32:2175–2183. https://doi.org/10.1007/s00464-017-5974-2
Roulin D, Blanc C, Muradbegovic M et al (2014) Enhanced recovery pathway for urgent colectomy. World J Surg 38:2153–2159. https://doi.org/10.1007/s00268-014-2518-y
Author information
Authors and Affiliations
Contributions
TN, ST, MA and AS conceived and planned the study design. AS was involved in planning and supervised the work. ST and MA performed the analysis. TN, AE and ST drafted the manuscript and designed the tables. AS, AT and TN supervised the project. All authors provided critical feedback and helped shape the research, analysis and manuscript. All authors discussed the results and commented on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Taras Nechay, Svetlana Titkova, Alexander Tyagunov, Mikhail Anurov and Alexander Sazhin certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethics approval
The study had been approved by the local Ethics Committee of Pirogov Russian National Research Medical University (Protocol No. 161-30-01-17).
Informed consent
All subjects gave informed voluntary consent for participation in the study.
Research involving human participants and/or animals
Study has been approved by the institutional ethics committee and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nechay, T., Titkova, S., Tyagunov, A. et al. Modified enhanced recovery after surgery protocol in patients with acute cholecystitis: efficacy, safety and feasibility. Multicenter randomized control study. Updates Surg 73, 1407–1417 (2021). https://doi.org/10.1007/s13304-021-01031-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-021-01031-5