Abstract
Faecal incontinence is a common complication of ileal pouch anal anastomosis (IPAA) and seems to worsen with time. The aim of this paper is to review the evidence of the use of sacral nerve stimulation (SNS) for patients with faecal incontinence after IPAA. A literature search was performed on PubMed and Cochrane databases for all relevant articles. All studies, which reported the outcome of SNS in patients with faecal incontinence after IPAA, were reviewed. Three papers were identified, including a case report, cohort study and retrospective study. The total number of patients was 12. The follow-up duration included 3 months, 6 months and 24 months. After peripheral nerve evaluation, definitive implantation was performed in 10 (83.3%) patients. All three studies reported positive outcomes, with CCF scores and incontinence episodes improving significantly. Preliminary results suggest good outcome after permanent SNS implant. Studies with larger sample sizes, well-defined patient characteristics and standardized outcome measures are required to fully investigate the effect of SNS in IPAA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ileal pouch anal anastomosis (IPAA), first described by Parks and Nicholls in 1978 [1], is the procedure of choice for patients with inflammatory bowel disease (IBD) and familial adenomatous polyposis (FAP) requiring surgery [2].
The overall functional outcome of IPAA is generally excellent [3,4,5,6]. However, faecal incontinence is a common complication of IPAA and seems to worsen with time [4]. Faecal incontinence is defined as the involuntary passage of rectal contents (faeces, flatus) through the anus and the inability to delay bowel movement until it is convenient. The issue should last at least 1 month and occurs in a child older than 4 years old and who has previously attained continence.
At 12 months post-IPAA, it has been reported that 19% of patients suffered occasional daytime incontinence and 49% suffered nocturnal incontinence [7]. Consequently, this can have a significantly negative impact on the quality of life of patients [8, 9].
Neuromodulation has gained support over the past 18 years as a treatment for faecal incontinence without any significant damage to the anal internal and external sphincters. By delivering chronic low-voltage electrical stimulation to the sacral spinal nerves, the muscles of the anal sphincter are recruited. The most established of neuromodulation treatments is sacral nerve stimulation (SNS) [10].
In practical terms, SNS involves the implantation of a programmable nerve stimulator in the subcutaneous tissue under general anaesthesia without the use of muscle relaxants. This delivers a continuous low amplitude electrical stimulation through the sacral nerve which can be accessed via the S3 or S4 foramen [11].
It has been shown that 80% of patients undergoing SNS with faecal incontinence not responsive to medical therapy had a > 50% improvement in symptoms [10]. Long-term results have shown a successful maintenance rate of 71% in patients 10 years after permanent SNS implant, with 50% maintaining full continence [12].
This systematic review will look at the use of SNS on faecal incontinence in IPAA patients.
Method
A literature search was performed on PubMed and Cochrane databases for all relevant articles. The following keywords were used in various combinations to conduct the search: ‘sacral nerve stimulation’, ‘SNS’, ‘restorative proctocolectomy (OR coloproctectomy)’, ‘pouch’, ‘IAA’ and ‘IPAA’. All studies which were identified in this search were analysed for relevance and content.
Results
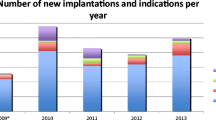
Nine studies were identified in the initial search and reviewed. Two studies were excluded based on the abstract alone. Four studies assessed the electrophysiology of the puborectalis muscle using SNS and not the long-term effect of SNS on faecal continence and therefore were deemed irrelevant to this review by both authors. The remaining three studies included 12 patients [11, 13, 14]. The characteristics of these studies are shown in Table 1 (Fig. 1).
In 2010, Meurette et al. [13] was the first to report the outcome of SNS for faecal incontinence following an IPAA in a case report. Meurette et al. reported the stimulation of the right S3 nerve root in a 46-year-old male patient who was referred for a severe attack of acute colitis. A subtotal colectomy with end ileostomy was performed and then 3 months later, a completion proctectomy with an IPAA reconstruction and a defunctioning loop ileostomy was performed, which was later reversed. He suffered faecal incontinence after the initial surgery for 3 years which had not improved despite optimised medical therapy and biofeedback. Endonanal ultrasonography showed no sphincter disruption. He experienced up to eight bowel movements per day with nocturnal soiling, with a Wexner/Cleveland Clinic (CCF) Incontinence Score of 16. An improvement, greater than 75% in incontinence episodes was experienced after percutaneous nerve evaluation (PNE) was performed on the right S3 nerve root. A permanent SNS device was then implanted. His CCF score had improved to less than 4 and frequency of stools per day had decreased to 5 with no nocturnal soiling at 1 year post-implantation.
Lebas et al. [14] described four female patients who had undergone SNS for severe faecal incontinence following restorative proctocolectomy and IPAA despite optimised medical therapy. The median age was 57 years (range 22–60 years). Patients had suffered faecal incontinence for a median duration of 54 months (range 20–160 months) prior to this study. Three of the four patients had a successful response to the PNE stimulation trial and continued to receive a permanent SNS implant. At 6 months after SNS, the median number of faecal incontinence episodes per week decreased from 4 (pre-SNS) to 0.5 (post-SNS). The median frequency of stools decreased from 8 (pre-SNS) to 5 (post SNS). Their ability to defer defecation had also improved from 6 min (pre-SNS) to 90 min (post-SNS). CCF scores also improved from 15 (pre-SNS) to 7 (post-SNS). Quality of life assessment for the three patients had improved in all categories at 3 and 6 months post-SNS. The patient who underwent IPAA for FAP reported perfect faecal continence 1 month post-SNS (Tables 2, 3).
Mege et al. [11] assessed the effectiveness of SNS on patients with faecal incontinence following colorectal resections, which included proctocolectomy with IPAA, rectal resection and left hemicolectomy. 7 out of 16 patients had undergone restorative proctocolectomy. Data for these seven patients were extracted from this study for analysis. A stimulation test was performed on the patients. Six of the seven patients had a satisfactory response to the SNS stimulation test and underwent pulse generator implantation for SNS. At a median follow-up of 18 (3.5–91) months, the median number of faecal incontinence episodes per week decreased from 4 (pre-SNS) to 1.8 (post-SNS). The CCF score decreased from 15 to 1.5. Daily stool frequency had also improved from 11 to 5 stools per day.
Discussion
This systematic review demonstrates the outcome of 10 patients who had undergone SNS.
All three studies reported positive outcomes, with CCF scores and incontinence episodes improving significantly. These results are promising, as they demonstrate the effect of SNS when other optimised medical therapies had been exhausted, and therefore improving the quality of life of patients. However, these results should be interpreted with caution. There are many confounding factors which can affect the results which include patient demographics such as age, gender, pre-existing bowel function and indication for IPAA. In addition to this, the pathophysiology of anorectal incontinence is not fully understood. As a result, it is still difficult to correlate subjective and objective parameters to predict outcome for each patient and hence determine which patients would benefit most from current treatment modalities. Current scoring systems including the most commonly used Wexner incontinence score, is based on subjective assessment of severity and frequency and does not include any physiologic test parameters which may have an effect on the result of SNS use [15].
It is also important to consider the shape of the pouch and its effect on faecal incontinence. In this review, not all articles commented on the type of pouch they had or whether they had tried any other treatment before SNS or in combination with it except a brief mention of failed optimised medical management. A Cochrane review in 2012 suggested that using SNS with pelvic floor muscles may confer some benefit although due to weakness of the data this is also not certain [16].
Risk factors implicated in faecal incontinence in patients who had an IPAA include advancing age at the time of surgery, longer disease duration preoperatively, being female and having lower preoperative maximum anal squeeze pressure which can affect the results of the SNS treatment [17].
Overall, there is a lack of good evidence in the literature to support the use of SNS in patients with faecal incontinence complications following IPAA. Studies with a larger sample size and longer follow-up duration are required to reciprocate these results. There is inconsistency in the literature regarding long-term SNS outcome on faecal incontinence. Some studies demonstrated a significant sustained long-term improvement in symptoms [18] whilst others reported a loss in long term efficacy for unknown reasons [19]. Future studies with longer follow-up durations investigating the outcome of SNS in IPAA patients should take this into consideration. This review may help plan larger randomised prospective studies in the effect of SNS on faecal incontinence following IPAA.
The mechanisms of action of SNS are unknown. However, studies have illustrated using electrophysiological assessments that sacral nerve terminal motor latency [20, 21] and anal resting and squeezing pressures are markedly improved after SNS [22, 23]. Continence is the result of both the anal sphincter functional contraction and the integrity and coordinated function for the surrounding pelvic muscles. SNS is hypothesized to affect both, and therefore its effect is multifactorial.
Conclusion
The evidence to support the use of SNS for faecal incontinence after IPAA remains very limited. Studies with larger sample sizes, well-defined patient characteristics and standardized outcome measures are required to investigate the effect of SNS in IPAA patients fully.
References
Parks AG, Nicholls RJ (1978) Proctocolectomy without ileostomy for ulcerative colitis. Br Med J 2(6130):85–88 (-0007-1447 (Print)):-85-88
Fazio VW, Ziv Y, Church JM, Oakley JR, Lavery IC, Milsom JW, Schroeder TK (1995) Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 222(2):120–127
Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR (2007) Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg 94(3):333–340. doi:10.1002/bjs.5464
Tekkis PP, Lovegrove RE, Tilney HS, Smith JJ, Sagar PM, Shorthouse AJ, Mortensen NJ, Nicholls RJ (2010) Long-term failure and function after restorative proctocolectomy—a multi-centre study of patients from the UK National Ileal Pouch Registry. Colorectal Dis 12(5):433–441. doi:10.1111/j.1463-1318.2009.01816.x
Delaney CP, Fazio VW, Remzi FH, Hammel J, Church JM, Hull TL, Senagore AJ, Strong SA, Lavery IC (2003) Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch-anal anastomosis. Ann Surg 238(2):221–228. doi:10.1097/01.sla.0000080825.95166.26
McGuire BB, Brannigan AE, O’Connell PR (2007) Ileal pouch-anal anastomosis. Br J Surg 94(7):812–823. doi:10.1002/bjs.5866
Meagher AP, Farouk R, Dozois RR, Kelly KA, Pemberton JH (1998) J ileal pouch-anal anastomosis for chronic ulcerative colitis: complications and long-term outcome in 1310 patients. Br J Surg 85(6):800–803. doi:10.1046/j.1365-2168.1998.00689.x
Ganschow P, Pfeiffer U, Hinz U, Leowardi C, Herfarth C, Kadmon M (2010) Quality of life ten and more years after restorative proctocolectomy for patients with familial adenomatous polyposis coli. Dis Colon Rectum 53(10):1381–1387. doi:10.1007/DCR.0b013e3181e56feb
O’Bichere A, Wilkinson K, Rumbles S, Norton C, Green C, Phillips RK (2000) Functional outcome after restorative panproctocolectomy for ulcerative colitis decreases an otherwise enhanced quality of life. Br J Surg 87(6):802–807. doi:10.1046/j.1365-2168.2000.01404.x
Thin NN, Horrocks EJ, Hotouras A, Palit S, Thaha MA, Chan CL, Matzel KE, Knowles CH (2013) Systematic review of the clinical effectiveness of neuromodulation in the treatment of faecal incontinence. Br J Surg 100(11):1430–1447. doi:10.1002/bjs.9226
Mege D, Meurette G, Vitton V, Leroi AM, Bridoux V, Zerbib P, Sielezneff I, Club N (2017) Sacral nerve stimulation can alleviate symptoms of bowel dysfunction after colorectal resections. Colorectal Dis 19(8):756–763. doi:10.1111/codi.13624
Altomare DF, Giuratrabocchetta S, Knowles CH, Munoz Duyos A, Robert-Yap J, Matzel KE, European SNSOSG (2015) Long-term outcomes of sacral nerve stimulation for faecal incontinence. Br J Surg 102(4):407–415. doi:10.1002/bjs.9740
Meurette G, Wong M, Paye F, Parc Y, Tiret E, Lehur PA (2011) Sacral nerve stimulation for the treatment of faecal incontinence after ileal pouch anal anastomosis. Colorectal Dis 13(7):e182–e183. doi:10.1111/j.1463-1318.2010.02352.x
Lebas A, Rogosnitzky M, Chater C, Colombel JF, Nachury M, Cortot A, Zerbib P (2014) Efficacy of sacral nerve stimulation for poor functional results of J-pouch ileoanal anastomosis. Tech Coloproctol 18(4):355–360. doi:10.1007/s10151-013-1058-z
Ruiz NS, Kaiser AM (2017) Fecal incontinence—challenges and solutions. World J Gastroenterol 23(1):11–24. doi:103748/wjgv23i111 (Epub 2017 Jan 7) (1007–9327 (Print)):11–24
Norton C, Cody JD (2012) Biofeedback and/or sphincter exercises for the treatment of faecal incontinence. D-100909747 (-1469-493X (Electronic))-CD002111
Kim H, Sun L, Gurland B, Hull T, Zutshi M, Church J (2015) Does stool leakage increase in aging pouches? Dis Colon Rectum 58(12):1158–1163. doi:101097/DCR0000000000000493 (-1530-0358 (Electronic)):1158–1163
Hull T, Giese C, Wexner SD, Mellgren A, Devroede G, Madoff RD, Stromberg K, Coller JA (2013) Long-term durability of sacral nerve stimulation therapy for chronic fecal. Dis Colon Rectum 56(2):234–245. doi:101097/DCR0b013e318276b24c (-1530-0358 (Electronic)):234–245
George AT, Kalmar K, Panarese A, Dudding TC, Nicholls RJ, Vaizey CJ (2012) Long-term outcomes of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum 55(3):302–306. doi:10.1097/DCR.0b013e3182401ecd
Tomita R, Kurosu Y, Isozumi M, Munakata K, Tanjoh K (1995) Sacral nerve terminal motor latency after ileal J pouch-anal anastomosis for ulcerative colitis. Surg Today 25(11):946–949
Tomita R, Kurosu Y, Munakata K (1996) Electrophysiologic assessments in pudendal and sacral motor nerves after ileal J-pouch-anal anastomosis for patients with ulcerative colitis and adenomatosis coli. Dis Colon Rectum 39(4):410–415
Matzel KE, Stadelmaier U, Hohenfellner M, Gall FP (1995) Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Lancet 346(8983):1124–1127
Matzel KE, Stadelmaier U, Hohenfellner M, Hohenberger W (2001) Chronic sacral spinal nerve stimulation for fecal incontinence: long-term results with foramen and cuff electrodes. Dis Colon Rectum 44(1):59–66
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving Human Participants and/or Animals
This review, does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kong, E., Nikolaou, S., Qiu, S. et al. A systematic review of sacral nerve stimulation for faecal incontinence following ileal pouch anal anastomosis. Updates Surg 70, 1–5 (2018). https://doi.org/10.1007/s13304-017-0496-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0496-y