Abstract
In the era of multimodal management of liver metastases, surgical resection remains the only curative option, with open approach still being referred to as the standard of care. Currently, the feasibility and benefits of the laparoscopic approach for liver resection have been largely demonstrated. However, its oncologic adequacy remains to be confirmed. The aim of this study is to report the oncological results of laparoscopic liver resection for metastatic disease in a single-centre experience. A single-centre database of 413 laparoscopic liver resections was reviewed and procedures for liver metastases were selected. The assessment of oncologic outcomes included analysis of minimal tumour-free margin, R1 resection rate and 3-year survival. The feasibility and safety of the procedures were also evaluated through analysis of perioperative outcomes. The study comprised 209 patients (294 procedures). Colorectal liver metastases were the commonest indication (67.9 %). Fourteen patients had conversion (6.7 %) and oncological concern was the commonest reason for conversion (42.8 %). Median tumour-free margin was 10 mm and complete radical resections were achieved in 211 of 218 curative-intent procedures (96.7 %). For patients affected by colorectal liver metastases, 1- and 3-year OS resulted 85.9 and 66.7 %. For patients affected by neuroendocrine liver metastases, 1- and 3-year OS resulted 93 and 77.8 %. Among the patients with metastases from other primaries, 1- and 3-year OS were 83.3 and 70.5 %. The laparoscopic approach is a safe and valid option in the treatment of patients with metastatic liver disease undergoing curative resection. It does offer significant perioperative benefits without compromise of oncologic outcomes.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics. CA Cancer J Clin 65(1):5–29
Stuart-Harris R, Shadbolt B, Palmqvist C, Chaudri Ross HA (2009) The prognostic significance of single hormone receptor positive metastatic breast cancer: an analysis of three randomised phase III trials of aromatase inhibitors. Breast 18(6):351–355
Moltzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J (1999) Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 17(8):2530–2540
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey JN, Nargoney DM, McWilliams RR (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27(22):3677–3683
Reddy SK, Zorzi D, Lum YW, Barbas AS, Pawlik TM, Ribero D, Abdalla EK, Choti MA, Kemp C, Vauthey JN, Morse MA, White RR, Clary BM (2009) Timing of multimodality therapy for resectable synchronous colorectal liver metastases: a retrospective multi-institutional analysis. Ann Surg Oncol 16(7):1809–1819
Gordon AC, Gradishar WJ, Kaklamani VG, Thuluvath AJ, Ryu RK, Sato KT, Gates VL, Salme R, Lewandowski RJ (2014) Yttrium-90 radioembolization stops progression of targeted breast cancer liver metastases after failed chemotherapy. J Vasc Interv Radiol 25(10):1523–1532
Tomlinson JS, Janargin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, Kemeny N, Brennan MF, Blumgart LH, D’Angelica M (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25(29):4575–4580
Khatri VP, Petrelli NJ, Belghiti J (2005) Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol 23(33):8490–8499
Tuttle TM, Curley SA, Roh MS (1997) Repeat hepatic resection as effective treatment of recurrent colorectal liver metastases. Ann Surg Oncol 4(2):125–130
Tranchart H, Di Giuro G, Lainas P, Pourcher G, Devaquet N, Perlemuter G, Franco D, Dagher I (2013) Laparoscopic liver resection with selective prior vascular control. Am J Surg 205(1):8–14
Kazaryan AM, Rosok BI, Marangos IP, Rosseland AR, Edwin B (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25(12):3881–3889
Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G (2010) Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 102(1):82–86
Di Fabio F, Samim M, Di Gioia P, Godeseth R, Pearce NW, Abu Hilal M (2014) Laparoscopic major hepatectomies: clinical outcomes and classification. World J Surg 38(12):3169–3174
Gagner M, Rogula T, Seizer D (2004) Laparoscopic liver resection: benefits and controversies. Surg Clin North Am 84(2):451–462
Lassen K, Hoye A, Myrmel T (2012) Randomised trials in surgery: the burden of evidence. Rev Recent Clin Trials 7(3):244–248
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157(2):211–222
Abu Hilal M, Underwood T, Zuccaro M, Primrose J, Pearce N (2010) Short- and medium-term results of totally laparoscopic resection for colorectal liver metastases. Br J Surg 97(6):927–933
Cheung TT, Poon RT, Yuen WK, Chok KS, Tsang SH, Yau T, Chan SC, Lo CM (2013) Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 83(11):847–852
Hasegawa Y, Nitta H, Sasaki A, Takahara T, Itabashi H, Katagiri H, Otsuka K, Nishizuka S, Wakabayashi G (2015) Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery doi:10.1016/j.surg.2015.01.017 [Epub ahead of print]
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg 250(2):177–186
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12:351–355
Pearce NW, Di Fabio F, Teng MJ, Syed S, Primrose JN, Abu Hilal M (2011) Laparoscopic right hepatectomy: a challenging, but feasible, safe and efficient procedure (How I do it). Am J Surg 202(5):52–58
Abu Hilal M, Pearce NW (2008) Laparoscopic left lateral sectionectomy: a safe, efficient, reproducible technique. Dig Surg 25(4):305–308
Pearce NW, Di Fabio F, Abu Hilal M (2011) Laparoscopic left hepatectomy with extraparenchymal inflow control. J Am Coll Surg 213(5):23–27
Abu Hilal M, Badran A, Di Fabio F, Pearce NW (2011) Pure laparoscopic en bloc left hemihepatectomy and caudate lobe resection in patients with intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 21(9):845–849
Abu Hilal M, Di Fabio F, Abu Salameh M, Pearce NW (2012) Oncological efficiency analysis of laparoscopic liver resection for primary and metastatic cancer. Arch Surg 147(1):42–48
Wakabayashi G et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in morioka. Ann Surg 261(4):619–629
Abu Hilal M, van der Poel MJ, Samim M, Besselink MG, Flowers D, Stedman B, Pearce NW (2015) Laparoscopic liver resection for lesions adjacent to major vasculature: feasibility, safety and oncological efficiency. J Gastrointest Surg 19(4):692–698
Shelat VG, Cipriani F, Basseres T, Armstrong TH, Takhar AS, Pearce NW, Abu Hilal M (2014) Pure laparoscopic liver resection for large malignant tumours: does size matter? Ann Surg Oncol Nov 8 PMID: 25380686
Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, Marvin M, Ravindra KV, Mejia A, Lainas P, Franco D, Cherqui D, Buell JF, Gamblin TC (2009) Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility and early outcomes. Ann Surg 250(5):842–848
Montalti R, Berardi G, Laurent S, Sebastiani S, Ferdinande L, Libbrecht LJ, Smeets P, Brescia A, Rogiers X, de Hemptinne B, Geboes K, Troisi R (2014) Laparoscopic liver resection compared to open approach in patients with colorectal liver metastases improves further resectability: oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol 40(5):536–544
Bodingbauer M, Tamandl D, Schmid K, Plank C, Schima W, Gruenberger T (2007) Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 94:1133–1138
Dhir M, Lyden ER, Wang A, Smith LM, Ullrich F, Are C (2011) Influence of margins on overall survival after hepatic resection for colorectal metastasis: a meta-analysis. Ann Surg 254:234–242
Ferrero A, Lo Tesoriere R, Russolillo N, Viganò L, Forchino F, Capussotti L (2015) Ultrasound-guided laparoscopic liver resections. Surg Endosc 29(4):1002–1005
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157(2):211–222
Samuels BL, Chawla S, Patel S, von Mehren M, Hamm J, Kaiser PE, Schuetze S, Li J, Aymes A, Demetri GD (2013) Clinical outcomes and safety with trabectedin therapy in patients wih advanced soft tissue sarcomas following failure of prior chemotherapy: results of a worldwide expanded access program study. Ann Oncol 24(6):1703–1709
Mauri D, Polyzos NP, Salanti G, Pavlidis N, Ioannidis JP (2008) Multiple-treatements meta-analysis of chemotherapy and targeted therapies in advanced breast cancer. J Natl Cancer Inst 100(24):1780–1791
Chua TC, Saxena A, Liauw W, Chu F, Morris DL (2011) Hepatic resection for metastatic breast cancer: a systematic review. Eur J Cancer 47(15):2282–2290
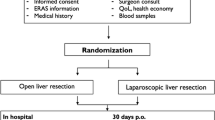
Fretland AA, Kazaryan AM, Bjornbeth BA, Flatmark K, Andersen MH, Tonnessen TI, Bjornlev GM, Fagerland MW, Kristiansen R, Oyri K, Edwin B (2015) Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet study): sudy ptotocol for a randomized controlled trial. Trials 16(1):73
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent form is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cipriani, F., Rawashdeh, M., Ahmed, M. et al. Oncological outcomes of laparoscopic surgery of liver metastases: a single-centre experience. Updates Surg 67, 185–191 (2015). https://doi.org/10.1007/s13304-015-0308-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-015-0308-1