Abstract
Tirzepatide is a first-in-class GIP/GLP-1 receptor agonist (‘twincretin’)—a single molecule that acts as an agonist at both glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors. In the SURPASS clinical trial program in type 2 diabetes mellitus (T2D), tirzepatide was associated with unprecedented reductions in HbA1c, clinically significant weight loss and other metabolic benefits, combined with low rates of hypoglycaemia across a wide range of patient characteristics. The safety and adverse event rate for tirzepatide appears comparable to that of GLP-1 receptor agonists. Although results from dedicated cardiovascular (CV) and kidney trials are currently not available, information to date suggests that tirzepatide may have CV and kidney benefits in people with T2D. Tirzepatide has been approved for the treatment of T2D in the USA, United Arab Emirates, European Union, Japan and Australia. Here, we review how tirzepatide will fit into the T2D treatment continuum. We also consider future directions with tirzepatide in T2D, including its potential for targeting cardio-renal-metabolic disease in T2D, and discuss how tirzepatide—and other co-agonists in development—may challenge current approaches for management of T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tirzepatide—a first-in-class GIP/GLP-1 receptor agonist (‘twincretin’)—is a single molecule that acts as an agonist at both GLP-1 and GIP receptors. |
Tirzepatide demonstrated substantial clinical benefits across a range of metabolic outcomes in a broad patient population and when compared with a range of therapies currently considered best practice in T2D management. |
A total of 43–62% of participants receiving tirzepatide 15 mg in the SURPASS clinical trials—even those with long-standing T2D—achieved normoglycaemia (HbA1c < 5.7%), and 39–51% achieved normoglycaemia together with clinically significant weight loss (≥ 5%) without hypoglycaemia. This challenges existing treatment paradigms and targets, which may need to be revised. |
Determining the future potential for tirzepatide in cardio-renal-metabolic disease will depend on the outcomes of dedicated cardiovascular outcomes and kidney trials, but tirzepatide may offer additional benefits beyond glycaemic control for individuals at high risk for or with established cardio-renal-metabolic disease. |
Introduction
Management of type 2 diabetes mellitus (T2D) remains a major challenge worldwide [1, 2], requiring a multifactorial approach to reduce cardiovascular risk and prevent and address metabolic comorbidities [3, 4].
The incretin hormones glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) are released by the gut in response to food intake [5]. In addition to their insulinotropic effects, they have a number of roles in tissues that express GLP-1 and/or GIP receptors, including the pancreas, brain and adipose tissue (Table S1, Supplementary Appendix) [6]. However, the incretin response is diminished in people with T2D [5, 6].
Tirzepatide is a first-in-class GIP/GLP-1 receptor agonist (‘twincretin’)—a single molecule that acts as a co-agonist at both GLP-1 and GIP receptors. The 39-amino acid peptide was developed to add the metabolic actions of GIP to the established clinical benefits of GLP-1 receptor agonism in T2D [7]. In the SURPASS clinical trial program, tirzepatide alone or in combination with other diabetes therapies was associated with clinically significant reduction in HbA1c, weight loss, improvements in lipid parameters and low rates of hypoglycaemia in people with T2D of varying duration [8,9,10,11,12]. Tirzepatide has been approved for use in the management of T2D by the US Food and Drug Administration [13], the European Medicines Agency [14] and the Australian Therapeutic Goods Administration [15]. It is also currently marketed in Japan and the United Arab Emirates.
This review explores the potential future role of tirzepatide in challenging current approaches for management of T2D. The article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Tirzepatide in T2D: SURPASS Clinical Trial Program
Results from SURPASS-1–5 have been published [8,9,10,11,12] and reviewed extensively elsewhere [16,17,18,19], so are only briefly summarised here. Further details of the SURPASS clinical trial program, study designs and outcomes are provided in the Supplementary Appendix.
Study Designs
The wide range of background therapies and study population characteristics at baseline in SURPASS-1–5 reflect the continuum of T2D disease (with mean disease duration ranging from 4.7 to 13.3 years) and treatment (including monotherapy, combination oral therapy and insulin). Tirzepatide was compared with active comparators (semaglutide 1 mg, basal insulins) as well as with placebo (Table 1, Table S2 Supplementary Appendix) [8,9,10,11,12]. In all phase 3 studies, tirzepatide was initiated at 2.5 mg sc once weekly and escalated by 2.5-mg increments every 4 weeks until the target dose of 5, 10 or 15 mg sc per week was reached [8,9,10,11,12].
HbA1c
Marked reductions in HbA1c were achieved with tirzepatide across the broad patient populations enrolled in SURPASS-1–5. HbA1c reductions with tirzepatide were dose dependent, ranging from − 1.9% to − 2.6% (− 20 to − 28 mmol/mol) and significantly greater than those achieved by any of the comparators in the studies (Fig. 1a) [8,9,10,11,12]. These reductions were sustained in those participants continuing therapy to week 104 in SURPASS-4 [11]. A substantial majority (81–97%) of participants receiving tirzepatide 5, 10 or 15 mg achieved HbA1c < 7% (< 53 mmol/mol). Moreover, HbA1c < 5.7% (< 39 mmol/mol), a value within the normal range for people without diabetes, was achieved by 43–62% of participants receiving tirzepatide 15 mg (Fig. S1, Supplementary Appendix) [8,9,10,11,12].
HbA1c, body weight and combined endpoint data from SURPASS-1–5 [8,9,10,11,12]. Data are estimated mean (SE) or percentage from the efficacy analysis set of the modified intent-to-treat population. A HbA1c change from baseline (primary efficacy endpoint) [8,9,10,11,12]. B Body weight change from baseline [8,9,10,11,12]. Figures A and B reproduced from Diabetes Obes Metab. De Block et al. 2022 [16]. ©2022 Eli Lilly and Company and The Authors. Diabetes, Obesity and Metabolism published by John Wiley & Sons Ltd. Reprinted with permission from John Wiley & Sons Ltd. This is an open-access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License. C Proportion of participants achieving a composite of HbA1c < 5.7% (39 mmol/mol) and ≥ 5% weight loss, without clinically significant or severe hypoglycaemia in SURPASS-1–5; Fig. C reproduced from Lingvay I et al. 2023 [20]. ©2022 Eli Lilly and Company. Diabetes, Obesity and Metabolism published by John Wiley & Sons Ltd. This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License. Figure c has also been adapted from 718-P: Patients Achieving an HbA1c < 5.7% with = 5% Weight Loss and without Hypoglycemia: A Post Hoc Analysis of SURPASS 1 to 5, American Diabetes Association, 2022 [21]. Copyright and all rights reserved. Material from this publication has been used with the permission of American Diabetes Association. *p < 0.001 superiority vs comparator [8–12]; **p < 0.001 vs comparator [21]; †p < 0.05 vs comparator. Met metformin, SGLT2i sodium-glucose cotransporter 2 inhibitor, SU sulfonylurea
Body Weight
Significantly greater reductions in body weight were observed with tirzepatide 5, 10 and 15 mg than with all comparators in SURPASS-1–5 (Fig. 1b) [8,9,10,11,12]; weight loss occurred even when tirzepatide was combined with therapies usually associated with weight gain, such as insulin or sulfonylureas [11, 12, 16]. Weight loss of > 5% was achieved by 77–88% of participants and weight loss of > 15% was achieved by 27–43% of participants receiving tirzepatide 15 mg (Fig. S2, Supplementary Appendix) [8,9,10,11,12]. Weight loss was accompanied by associated reductions in waist circumference [8,9,10,11,12].
Composite Outcome
A post hoc analysis evaluated the proportion of participants who achieved the triple endpoints of glycaemic control, weight loss, and no clinically significant or severe hypoglycaemia (defined as blood glucose < 3 mmol/L with symptoms or severe hypoglycaemia requiring assistance for treatment) [20]. Significantly more participants achieved the triple endpoint of normoglycaemia (HbA1c < 5.7% [39 mmol/mol]), ≥ 5% weight loss and no hypoglycaemia with tirzepatide 15 mg (39–51%) compared with placebo or active comparators (1–15%) (Fig. 1c) [20, 21].
Kidney Outcomes
An exploratory analysis of the SURPASS-4 study suggested tirzepatide may have kidney-protective effects [22]. Tirzepatide slowed the rate of decline in estimated glomerular filtration rate (eGFR) and reduced urinary albumin-to-creatinine ratio (UACR) compared with insulin glargine (UACR remained stable with tirzepatide but increased with insulin glargine), including in participants already receiving an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker or sodium-glucose cotransporter 2 inhibitor (SGLT2i); these effects were within clinically meaningful ranges (Fig. 2) [22].
Rate of eGFR decline and change in UACR in SURPASS-4. Changes in kidney function between baseline and end of treatment for the tirzepatide (pooled doses) versus insulin glargine groups in SURPASS-4 [22]. A Rate of decline in eGFR (mL/min/1.73 m2) per year. Mean baseline eGFR 81.3 mL/min/1.73 m2. B Percentage change in UACR from baseline median baseline UACR 15.0 mg/g, median treatment duration 85 weeks. ACEi angiotensin-converting enzyme inhibitors, ARB angiotensin receptor blocker, eGFR estimated glomerular filtration rate, SGLT-2i sodium-glucose co-transporter 2 inhibitor, UACR urinary albumin-to-creatinine ratio. Created using data from Heerspink et al. [22]
The difference in kidney outcomes between tirzepatide- and insulin glargine-treated participants was generally consistent across all participant groups but were more pronounced in participants with reduced kidney function at baseline [22]. In addition, achievement of a renal composite end point of decline in eGFR to ≥ 40% from baseline, death due to kidney disease or progression to end-stage kidney disease, and new-onset macroalbuminuria was 42% lower in study participants receiving tirzepatide compared with insulin glargine (p = 0.0008). Although the favourable effect of tirzepatide on this endpoint appeared to be predominantly driven by a reduction in new onset macroalbuminuria [22], it is worth noting that the differences in changes in albuminuria during the time course of the study were mainly attributable to a progressive increase in the insulin glargine group whereas levels remained relatively stable in the tirzepatide-treated group.
Lipid Profile
Tirzepatide was associated with dose-dependent favourable effects on lipid profile, including reductions in triglycerides and very-low-density lipoprotein cholesterol (VLDL-C), and increases in high-density lipoprotein cholesterol (HDL-C) in SURPASS-1–5 [8,9,10,11,12]. In SURPASS-4, tirzepatide 5, 10 and 15 mg reduced triglycerides, low-density lipoprotein cholesterol (LDL-C) and total cholesterol, and increased HDL-C, compared with baseline and the active comparator in the high CV risk population (82% on lipid-lowering therapy at baseline, which was continued throughout the study) [11]. In SURPASS-2, reductions in triglycerides and VLDL-C with tirzepatide (all doses) exceeded those seen with semaglutide 1 mg [9].
Insulin Use
In SURPASS-5, participants on tirzepatide required significantly less background basal insulin than those on placebo (p < 0.001, all doses). By the end of the study, mean daily insulin dose decreased from baseline by 3.8 U (− 11.4%) in participants receiving insulin glargine plus tirzepatide 15 mg but increased by 25.1 U (75%) in those receiving insulin glargine plus placebo [12]. (Participants self-adjusted background daily insulin glargine dose on the basis of self-monitored blood glucose using a treat-to-target algorithm.)
Tolerability
The most common adverse events with tirzepatide were similar to those seen with GLP-1 receptor agonists (GLP-1RA), namely gastrointestinal (GI) events such as nausea, diarrhoea and vomiting [8,9,10,11,12, 16]. These were mostly mild-to-moderate in severity and transient, occurring more frequently during the dose escalation phase of each study (Fig. S3, Supplementary Appendix). Severe diarrhoea and severe vomiting were uncommon with tirzepatide, affecting 0.31% and 0.25% of participants, respectively [8,9,10, 12]. In SURPASS-2, the rates of all reported GI side effects—including nausea, diarrhoea, vomiting, dyspepsia, decreased appetite, constipation and abdominal pain—occurring with tirzepatide (40–44.9%) were generally comparable to those seen with semaglutide (41.2%) [9].
Hypoglycaemia
The incidence of hypoglycaemia (blood glucose < 3 mmol/L) or severe hypoglycaemia (requiring assistance for treatment) with tirzepatide was generally low across SURPASS-1–5 [8,9,10,11,12]. Risk increased with concomitant sulfonylurea or insulin use; for example among tirzepatide-treated participants in SURPASS-4, hypoglycaemia was reported by 10–14% of those using SU at baseline compared with 1–3% of those not using an SU [11].
Cardiovascular Safety
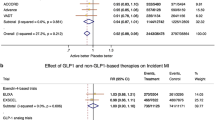
There was no increased CV risk with tirzepatide compared with insulin glargine in the SURPASS-4 study, which enrolled participants with high CV risk [11]. Additionally, tirzepatide did not increase the risk of CV events versus controls (active comparator or placebo) in a prespecified CV safety meta-analysis of 7215 clinical trial participants: hazard ratio for major adverse cardiovascular events (MACE-4; cardiovascular death, myocardial infarction, stroke or hospitalisation for unstable angina) 0.80 (95% CI 0.57–1.11) (Fig. S4, Supplementary Appendix) [23]. The median duration of follow-up for this analysis was 55 weeks; longer follow-up may have been needed to demonstrate benefit.
Systolic and diastolic blood pressures were reduced with tirzepatide in all SURPASS trials in a dose-dependent manner [8,9,10,11,12]. As seen with GLP-1RA clinical trials, small increases in pulse rate occurred in the SURPASS studies [8,9,10,11,12, 24]; mean pulse rates did not differ significantly between the tirzepatide- and semaglutide-treated groups in SURPASS-2 [9].
The ongoing CV outcomes trial, SURPASS-CVOT, will compare tirzepatide with dulaglutide (a GLP-1RA with established cardiovascular protection [25, 26]) in approximately 12,500 participants with T2D and atherosclerotic CV disease. The study started recruiting in May 2020 and completion is anticipated in October 2024 (maximum treatment duration approximately 54 months) [27].
Adverse Events of Special Interest
Adverse events of special interest with incretin-based therapies include medullary thyroid carcinoma, pancreatitis, cholelithiasis and diabetic retinopathy [28].
No cases of medullary thyroid carcinoma were reported during SURPASS-1–5, and pancreatitis, cholelithiasis and diabetic retinopathy were reported in fewer than 1% of participants receiving any dose of tirzepatide or control (Table S3, Supplementary Appendix) [8,9,10,11,12].
Implications for Management of T2D in Clinical Practice
The SURPASS program demonstrated substantial clinical benefits with tirzepatide 5 mg, 10 mg and 15 mg across a broad patient population and when compared with a range of therapies currently considered best practice in T2D management [3, 8,9,10,11,12]. It is reasonable to expect that results from SURPASS clinical trials may drive important updates to T2D management guidelines and clinical practice. Indeed, the American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) updated their 2022 consensus statement for T2D to include tirzepatide [4].
Fitting Tirzepatide into the T2D Treatment Continuum
Tirzepatide is effective across the T2D treatment continuum, from initial drug therapy through to those not at target on basal insulin (mean T2D duration 4.7–13.3 years in the SURPASS studies) [8,9,10,11,12].
Metformin is universally recognised as the first-line therapy for people with T2D not reaching glycaemic targets with diet and exercise. The optimum add-on therapy to metformin is less clear. Findings from the recent Glycemia Reduction Approaches in Type 2 Diabetes: A Comparative Effectiveness (GRADE) study support the early introduction of incretin-based therapies in the T2D treatment pathway, although it should be noted that GRADE did not include a SGLT2i treatment arm [29, 30].
In view of the microvascular and macrovascular benefits and long-term legacy effects of early, intensive HbA1c control, it would seem logical to introduce a highly effective agent such as tirzepatide early in the T2D treatment pathway. Given the benefits of tirzepatide on weight, waist circumference, and lipid parameters in addition to impressive improvements in glycaemic control, this medication appears to be ideally placed as first add-on therapy for individuals not at HbA1c target on metformin, particularly for those with T2D and excess adiposity (Table 2, clinical scenario A). However, this will need to be considered in the context of data from cardiovascular and kidney outcome trials involving tirzepatide. Addition of tirzepatide should also be considered for any person with T2D who would benefit from weight loss and those not reaching glycaemic targets on current therapies. In practice, it is likely that use of tirzepatide will be driven by cost and funding considerations, in addition to clinical benefits.
The future role and position of insulins in the T2D treatment continuum will need to be reconsidered, given incretin-based therapies provide substantial reduction in HbA1c without the potential for weight gain and hypoglycaemia seen with insulins. Tirzepatide may be considered for individuals not at target on basal insulin with the aim of improving glycaemic control, decreasing weight and minimising risk of hypoglycaemia [12] (Table 2, clinical scenario B). Outcomes from SURPASS-6 (tirzepatide vs insulin lispro in people with T2D on insulin glargine ± metformin [31]) will further establish the role of tirzepatide in people currently not at target on basal insulin.
Results from SURPASS-CVOT should help establish the role of tirzepatide in managing people with T2D and CV disease. Furthermore, an ongoing study in people aged 10–18 years with T2D will help establish its safety and efficacy in children and adolescents [32].
Where to Next? Future Directions in T2D & Beyond
Should HbA1c Targets be Revised in T2D?
Normoglycaemia, previously considered unachievable, is becoming a potential reality in T2D. Up to 51% of participants in the SURPASS program, even those with long-standing diabetes, achieved normoglycaemia and clinically significant weight loss without hypoglycaemia [21]. This unparalleled potency challenges existing treatment paradigms and targets, which may need to be revised.
Early and intensive HbA1c control in people with newly diagnosed T2D is well established for the prevention and management of microvascular complications [33] and has demonstrated a long-term legacy effect on macrovascular outcomes [34]. However, macrovascular benefit was elusive in people with T2D of longer duration (7.9–11.5 years) in the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) and Veterans Affairs Diabetes Trial (VADT) studies [35, 36], and the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study reported increased CV mortality [37]. Further analyses suggested that increased rates of hypoglycaemia may have contributed to the lack of CV benefit with intensive HbA1c lowering in these studies [38, 39]. More recently, risk reduction for MACE was shown to be proportional to the magnitude of HbA1c decrease when agents with less hypoglycaemic potential were considered [39].
Tirzepatide did not increase CV risk in the SURPASS-1–5 studies [23], although subset analysis of participants achieving HbA1c < 5.7% (< 39 mmol/mol) was not reported. The ongoing CV outcomes trial, SURPASS-CVOT (anticipated completion 2024) [27], may help to establish the CV safety of achieving normoglycaemia with tirzepatide in people with T2D.
Current guidelines recommend that HbA1c targets in T2D are individualised, but a general target of ≤ 7% (≤ 53 mmol/mol) is commonly accepted [3, 4]. With the introduction of agents able to achieve normoglycaemia together with weight reduction without increased risk of hypoglycaemia, it is enticing to consider how outcomes for people with T2D might change if the HbA1c treatment goal was updated to be normoglycaemia. An HbA1c target closer to < 5.7% (39 mmol/mol), achieved early in the course of T2D, could potentially minimise the onset and progression of microvascular disease and have a legacy effect on macrovascular outcomes [34]. This potentially could reduce the burden of disease for people living with diabetes, and also reduce the burden on healthcare systems (tertiary and primary care).
Follow-up of the SURPASS clinical trials to assess long-term outcomes for the subgroup of participants who reached normoglycaemia with weight loss and no hypoglycaemia should add to the body of knowledge on prevention of complications associated with T2D, including emerging diabetes weight-related complications such as cancer, fatty liver disease and obstructive sleep apnoea.
Targeting Multi-morbidities in T2D
Weight Loss
Weight loss in T2D can improve glycaemic control, insulin sensitivity and comorbidities [40, 41]. A person-centred approach focussing on updated weight loss targets—now achievable with therapies such as tirzepatide—may improve not only glycaemic control but also other metabolic complications for people with adiposity-associated T2D, including blood pressure, lipids, obstructive sleep apnoea and fatty liver disease. Non-metabolic progressive comorbidities such as osteoarthritis would also be expected to benefit from substantial weight loss.
Although weight loss is recognised as beneficial in the majority of people with T2D, it is challenging to maintain long-term and treatment targets have not been a focus of management [42]. Bariatric surgery is currently the most effective means of achieving substantial weight loss; clinical studies with Roux-en-Y gastric bypass in people with obesity and T2D demonstrated mean weight losses of 26–33%, compared with 5–8% in those receiving medical management [43]. Furthermore, bariatric surgery plus intensive medical therapy was superior to intensive medical therapy alone for decreasing (and in some subjects, resolving) hyperglycaemia in T2D plus obesity [44]. However, bariatric surgery is not feasible as a population-wide intervention for people with T2D [42].
With respect to glucose-lowering medications, the 2022 ADA/EASD consensus statement emphasises the need to focus on both glycaemic and weight management goals, and lists tirzepatide or semaglutide as having very high efficacy for weight loss [4]. Across the SURPASS studies, tirzepatide reduced mean body weight by 6.2–12.9 kg, with 7–43% achieving weight loss greater than 15%—including in participants receiving agents promoting weight gain, such as insulin [8,9,10,11,12]. Significantly greater weight losses were seen with tirzepatide than with semaglutide 1.0 mg in SURPASS-2, and significantly more participants achieved greater than 15% weight loss [9]. Weight loss achievable with medical therapy is becoming closer to that seen with bariatric surgery in people with T2D and obesity, potentially making sustained, substantial weight loss achievable for a greater proportion of these individuals.
Cardio-Renal-Metabolic Disease
Cardio-renal-metabolic (CRM) disease involves multidirectional interactions between CV disease, hypertension, kidney disease and metabolic disorders such as T2D, dyslipidaemia and obesity [45,46,47]. A holistic approach to CRM care that recognises the interconnected nature of these disorders may improve patient outcomes compared with isolated treatment of the individual conditions [47,48,49,50]. Although SGLT2i have offered a therapeutic option for CRM syndrome [48], there remains an unmet need for effective agents in this area.
Tirzepatide has demonstrated improved metabolic outcomes, including reductions in HbA1c, body weight and blood pressure, and improvement in lipid profile [8,9,10,11,12]. Information available to date suggests that tirzepatide may also have CV and kidney benefits in people with T2D [22, 23]. Determining the future potential for tirzepatide in CRM disease will depend on the outcomes of dedicated CV and kidney trials, but it is tempting to consider whether it might provide a treatment option for individuals at risk (Fig. 3).
Knowledge Gaps with Tirzepatide
The SURPASS clinical trial program was comprehensive, but some knowledge gaps remain regarding its use.
Most of the SURPASS studies were of 40–52 weeks duration. Long-term efficacy and safety data are needed to assess the durability of improved glycaemic control and weight loss, and to further elucidate the potential for adverse events of special interest such as diabetic retinopathy, cholelithiasis, thyroid medullary cancer and adverse pancreatic outcomes. The current studies did not identify red flags for retinopathy, but people with diabetic maculopathy, proliferative diabetic retinopathy, or non-proliferative diabetic retinopathy that required urgent treatment were excluded from the studies. Regardless of treatment modality, rapid improvements in glycaemic control can result in a temporary worsening of diabetic retinopathy [51], and prescribers of tirzepatide should be mindful of this.
SGLT2i is now recognised by many international guidelines as a first add-on therapy option for people with T2D not at HbA1c target on metformin, especially in those with or at high-risk of CV disease and kidney disease [4]. It would be useful to further explore the efficacy of adding tirzepatide to SGLT2i; subgroup analysis of SURPASS-3 and -4 may provide information on this combination. SURPASS-CVOT may also offer insights into the safety of the combination, as participants could receive other diabetes therapies, including SGLT2i, during the study.
Whilst kidney outcomes identified in SURPASS-4 were promising [22], the true renal protective effects of tirzepatide, and indeed other GLP-1RAs, await the results of dedicated kidney outcome studies in people with established diabetic kidney disease and renal impairment that assess the risk of progressing to kidney failure as their primary endpoint. Further subgroup analyses or future clinical trials would be useful to determine efficacy of tirzepatide in other targeted populations such as the elderly or different ethnic groups.
Other Indications
Tirzepatide is currently being investigated for use in other conditions, including obesity, heart failure with preserved ejection fraction (HFpEF) and non-alcoholic steatohepatitis (NASH).
Greater weight loss was seen with tirzepatide in the 72-week, phase 3 SURMOUNT study in people with obesity without T2D than in the SURPASS studies. This was expected, as weight loss achieved with any intervention in people without T2D generally exceeds that seen in people with T2D [42]. Tirzepatide 5, 10 and 15 mg demonstrated substantial and sustained reductions in body weight of 15.0%, 19.5% and 20.9%, respectively, versus 3.1% with placebo. Notably, 57% of participants receiving tirzepatide 10 or 15 mg achieved weight loss of 20% or more [52]. This approaches the weight loss typically expected for bariatric surgery, which is in the range of 25–35% [53], and suggests tirzepatide could play an important role in managing obesity.
The phase 3 SUMMIT study in people with HFpEF and obesity [54] and the phase 2 SYNERGY-NASH study [55] are ongoing.
Other Incretin Co-agonists and Combinations in Development
Tirzepatide is a first-in-class GIP/GLP-1 receptor agonist, but there are numerous other incretin-based co-agonists and combination therapies at various stages of preclinical and clinical development for different metabolic disorders. A wide range of potential partners to GLP-1 agonists have been investigated, including glucagon, amylin, cholecystokinin, fibroblast growth factors, and neuroreceptor Y2 (NPY2), as well as GIP receptor agonists and antagonists [56,57,58].
Several GLP-1/glucagon co-agonists have been investigated in phase 1 or 2 clinical trials [57]. A phase 2b study with once-daily cotadutide 100, 200 or 300 µg in T2D demonstrated reductions in HbA1c and body weight similar to those achieved with liraglutide 1.8 mg and significantly greater than those seen with placebo [59]. Gastrointestinal disorders were the most commonly reported adverse event; these occurred more frequently with cotadutide than with liraglutide or placebo, but incidence decreased over time [59]. Gastrointestinal adverse events and other safety issues have hindered the development of some GLP-1/glucagon co-agonist candidates, and several (e.g. SAR425899, efinopegdutide, NNC9204-1177) have been discontinued from development for management of T2D/obesity [57, 60].
Oxyntomodulin is an endogenous gut hormone that acts at both GLP-1 and glucagon receptors to reduce food intake and increase energy expenditure [61]. Mazdutide (LY3305677), an oxyntomodulin analogue, is currently in early clinical development and was reported to be well tolerated at doses up to 10 mg [62,63,64]
CagriSema, a combination of semaglutide 2.4 mg plus cagrilintide (an amylin analogue), is currently in development for obesity and T2D. A phase 1b trial in overweight/obese participants demonstrated an acceptable safety profile with reductions in body weight of up to 17% [65]. A 32-week phase 2 study in people with T2D (n = 92) demonstrated decreases in HbA1c of − 2.2% with CagriSema vs − 1.8% with semaglutide 2.4 mg (p = 0.075) and 0.9% with cagrilintide (p < 0.0001). Reductions in body weight were greater with CagriSema (− 15.6%) than with semaglutide 2.4 mg (− 5.1%) or cagrilintide (− 8.1%) (both p < 0.0001) [66].
Triple agonists are also in development. LY3437943, a novel triple GIP/GLP-1/glucagon co-agonist has been studied in people with T2D. In a phase 1, 12-week study with multiple ascending doses, placebo-adjusted mean decreases in HbA1c of up to 1.56% and body weight decreases of up to 8.96 kg were observed [67].
Most combination/co-agonist incretin-based therapies in development focus on improving efficacy, but preclinical studies with the GLP-1/NPY2 co-agonist GEP44 examined the potential for mitigation of nausea and vomiting [58]. GEP44 reduced food intake and body weight compared to exendin-4 controls, with little to no nausea behaviour (in rats) or emesis (in musk shrews). Further investigation of incretin-based therapies with reduced gastrointestinal adverse event profile is warranted [58].
Conclusion
Tirzepatide is the first GIP/GLP-1 receptor agonist approved for the treatment for T2D. Clinical trial results suggest that tirzepatide will provide a major advancement in the treatment of T2D and its associated metabolic derangements such as cardio-renal-metabolic disease. Tirzepatide lowers glucose levels and reduces body weight more effectively than GLP-1 RA with a similar safety and adverse event profile. A recent CV meta-analysis has shown that tirzepatide does not increase major CV events compared with other glucose-lowering therapies. Supportive data for a kidney-protective effect of tirzepatide has also recently been published. Determining the optimal place for tirzepatide in T2D treatment algorithms may depend on the outcomes of dedicated CV and kidney trials and long-term safety studies. Phase 3 clinical studies with other co-agonists are awaited with interest.
Data Availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
References
Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract. 2018;137:137–48.
Blonde L, Aschner P, Bailey C, Ji L, Leiter LA, Matthaei S. Gaps and barriers in the control of blood glucose in people with type 2 diabetes. Diab Vasc Dis Res. 2017;14:172–83.
American Diabetes Association. Standards of Medical Care in Diabetes—2022 Abridged for Primary Care Providers. Clin Diabetes. 2022;40:10–38.
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45:2753–86.
Holst JJ, Gasbjerg LS, Rosenkilde MM. The role of incretins on insulin function and glucose homeostasis. Endocrinology. 2021;162:bqab065.
Nauck MA, Quast DR, Wefers J, Pfeiffer AFH. The evolving story of incretins (GIP and GLP-1) in metabolic and cardiovascular disease: a pathophysiological update. Diabetes Obes Metab. 2021;23(Suppl 3):5–29.
Coskun T, Sloop KW, Loghin C, et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14.
Rosenstock J, Wysham C, Frías JP, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398:143–55.
Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385:503–15.
Ludvik B, Giorgino F, Jódar E, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 2021;398:583–98.
Del Prato S, Kahn SE, Pavo I, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. 2021;398:1811–24.
Dahl D, Onishi Y, Norwood P, et al. Effect of subcutaneous tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA. 2022;327:534–45.
Food and Drug Administration. FDA approves novel, dual-targeted treatment for type 2 diabetes. https://www.fda.gov/news-events/press-announcements/fda-approves-novel-dual-targeted-treatment-type-2-diabetes. Accessed May 2023.
European Medicines Agency. Mounjaro. https://www.ema.europa.eu/en/medicines/human/EPAR/mounjaro. Accessed May 2023.
Therapeutic Goods Administration. Mounjaro. https://www.tga.gov.au/resources/auspmd/mounjaro. Accessed May 2023.
De Block C, Bailey C, Wysham C, Hemmingway A, Allen SE, Peleshok J. Tirzepatide for the treatment of adults with type 2 diabetes: an endocrine perspective. Diabetes Obes Metab. 2023;25:3–17.
Nauck MA, D’Alessio DA. Tirzepatide, a dual GIP/GLP-1 receptor co-agonist for the treatment of type 2 diabetes with unmatched effectiveness regrading glycaemic control and body weight reduction. Cardiovasc Diabetol. 2022;21:169.
Kaneko S. Tirzepatide: a novel, once-weekly dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes. TouchREV Endocrinol. 2022;18:10–9.
Nowak M, Nowak W, Grzeszczak W. Tirzepatide—a dual GIP/GLP-1 receptor agonist—a new antidiabetic drug with potential metabolic activity in the treatment of type 2 diabetes. Endokrynol Pol. 2022;73:745–55.
Lingvay I, Cheng AY, Levine JA, et al. Achievement of glycaemic targets with weight loss and without hypoglycaemia in type 2 diabetes with the once-weekly glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist tirzepatide: a post hoc analysis of the SURPASS-1 to -5 studies. Diabetes Obes Metab. 2023;25:965–74.
Cheng A, Lingvay I, Choudhary P, et al. 718-P: Patients achieving an HbA1c <5.7% with =5% weight loss and without hypoglycemia: a post hoc analysis of SURPASS 1 to 5. Diabetes. 2022;71:718-P.
Heerspink HJL, Sattar N, Pavo I, et al. Effects of tirzepatide versus insulin glargine on kidney outcomes in type 2 diabetes in the SURPASS-4 trial: post-hoc analysis of an open-label, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2022;10:774–85.
Sattar N, McGuire DK, Pavo I, et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591–8.
Lorenz M, Lawson F, Owens D, et al. Differential effects of glucagon-like peptide-1 receptor agonists on heart rate. Cardiovasc Diabetol. 2017;16:6.
Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394:121–30.
MacIsaac RJ. Glucagon-like peptide-1 receptor agonists and the cardiorenal axis in type 2 diabetes: a focus on dulaglutide. Future Cardiol. 2021;17:459–73.
Eli Lilly. A study of tirzepatide (LY3298176) compared with dulaglutide on major cardiovascular events in participants with type 2 diabetes (SURPASS-CVOT; NCT04255433). https://clinicaltrials.gov/ct2/show/record/NCT04255433. Accessed May 2023.
Smits MM, Van Raalte DH. Safety of semaglutide. Front Endocrinol. 2021;12:645563.
GRADE Study Research Group, Nathan DM, Lachin JM, et al. Glycemia reduction in type 2 diabetes—glycemic outcomes. N Engl J Med. 2022;387:1063–74.
GRADE Study Research Group, Nathan DM, Lachin JM, et al. Glycemia reduction in type 2 diabetes—microvascular and cardiovascular outcomes. N Engl J Med. 2022;387:1075–88.
Eli Lilly. A randomized, phase 3, open-label trial comparing the effect of the addition of tirzepatide once weekly versus insulin lispro (U100) three times daily in participants with type 2 diabetes inadequately controlled on insulin glargine (U100) with or without metformin (SURPASS-6; NCT04537923). https://clinicaltrials.gov/ct2/show/NCT04537923. Accessed May 2023.
Eli Lilly. A study to evaluate tirzepatide (LY3298176) in pediatric and adolescent participants with type 2 diabetes mellitus inadequately controlled with metformin or basal insulin or both (SURPASS-PEDS; NCT05260021). https://clinicaltrials.gov/ct2/show/record/NCT05260021. Accessed May 2023.
Sun S, Hisland L, Grenet G, et al. Reappraisal of the efficacy of intensive glycaemic control on microvascular complications in patients with type 2 diabetes: a meta-analysis of randomised control-trials. Therapie. 2022;77:413–23.
Lind M, Imberg H, Coleman RL, Nerman O, Holman RR. Historical HbA1c values may explain the type 2 diabetes legacy effect: UKPDS 88. Diabetes Care. 2021;44:2231–7.
ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Hsu P-F, Sung S-H, Cheng H-M, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care. 2013;36:894–900.
Huang C-J, Wang W-T, Sung S-H, et al. Revisiting ‘intensive’ blood glucose control: a causal directed acyclic graph-guided systematic review of randomized controlled trials. Diabetes Obes Metab. 2022;24:2341–52.
Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391:541–51.
Sjöholm K, Sjöström E, Carlsson LMS, Peltonen M. Weight change-adjusted effects of gastric bypass surgery on glucose metabolism: 2- and 10-year results from the Swedish Obese Subjects (SOS) study. Diabetes Care. 2016;39:625–31.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399:394–405.
Pareek M, Schauer PR, Kaplan LM, Leiter LA, Rubino F, Bhatt DL. Metabolic surgery: weight loss, diabetes, and beyond. J Am Coll Cardiol. 2018;71:670–87.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376:641–51.
Sowers JR, Whaley-Connell A, Hayden MR. The role of overweight and obesity in the cardiorenal syndrome. Cardiorenal Med. 2011;1:5–12.
Whaley-Connell A, Sowers JR. Basic science: pathophysiology: the cardiorenal metabolic syndrome. J Am Soc Hypertens. 2014;8:604–6.
Kadowaki T, Maegawa H, Watada H, et al. Interconnection between cardiovascular, renal and metabolic disorders: a narrative review with a focus on Japan. Diabetes Obes Metab. 2022;24:2283–96.
Akiyama H, Nishimura A, Morita N, Yajima T. Evolution of sodium-glucose co-transporter 2 inhibitors from a glucose-lowering drug to a pivotal therapeutic agent for cardio-renal-metabolic syndrome. Front Endocrinol. 2023;14:1111984.
Rangaswami J, Tuttle K, Vaduganathan M. Cardio-renal-metabolic care models: toward achieving effective interdisciplinary care. Circ Cardiovasc Qual Outcomes. 2020;13:e007264.
Sasso FC, Simeon V, Galiero R, et al. The number of risk factors not at target is associated with cardiovascular risk in a type 2 diabetic population with albuminuria in primary cardiovascular prevention. Post-hoc analysis of the NID-2 trial. Cardiovasc Diabetol. 2022;21:235.
Bain SC, Klufas MA, Ho A, Matthews DR. Worsening of diabetic retinopathy with rapid improvement in systemic glucose control: a review. Diabetes Obes Metab. 2019;21:454–66.
Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387:205–16.
Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118:1844–55.
Eli Lilly. A randomized, double-blind, placebo-controlled, phase 3 study comparing the efficacy and safety of tirzepatide versus placebo in patients with heart failure with preserved ejection fraction and obesity (SUMMIT; NCT04847557). https://clinicaltrials.gov/ct2/show/NCT04847557. Accessed May 2023.
Eli Lilly. A study of tirzepatide in patients with nonalcoholic steatohepatitis (NASH) (SYNERGY-NASH; NCT04166773). https://clinicaltrials.gov/ct2/show/NCT04166773. Accessed May 2023.
Baggio LL, Drucker DJ. Glucagon-like peptide-1 receptor co-agonists for treating metabolic disease. Mol Metab. 2020;46:101090.
Hope DCD, Vincent ML, Tan TMM. Striking the balance: GLP-1/glucagon co-agonism as a treatment strategy for obesity. Front Endocrinol (Lausanne). 2021;12:735019.
Milliken BT, Elfers C, Chepurny OG, et al. Design and evaluation of peptide dual-agonists of GLP-1 and NPY2 receptors for glucoregulation and weight loss with mitigated nausea and emesis. J Med Chem. 2021;64:1127–38.
Nahra R, Wang T, Gadde KM, et al. Effects of cotadutide on metabolic and hepatic parameters in adults with overweight or obesity and type 2 diabetes: a 54-week randomized phase 2b study. Diabetes Care. 2021;44:1433–42.
Simonsen L, Lau J, Kruse T, et al. Preclinical evaluation of a protracted GLP-1/glucagon receptor co-agonist: translational difficulties and pitfalls. PLoS One. 2022;17:e0264974.
Pocai A. Action and therapeutic potential of oxyntomodulin. Mol Metab. 2013;3:241–51.
Ji L, Jiang H, An P, et al. IBI362 (LY3305677), a weekly-dose GLP-1 and glucagon receptor dual agonist, in Chinese adults with overweight or obesity: a randomised, placebo-controlled, multiple ascending dose phase 1b study. EClinicalMedicine. 2021;39: 101088.
Jiang H, Pang S, Zhang Y, et al. A phase 1b randomised controlled trial of a glucagon-like peptide-1 and glucagon receptor dual agonist IBI362 (LY3305677) in Chinese patients with type 2 diabetes. Nat Commun. 2022;13:3613.
Ji L, Gao L, Jiang H, et al. Safety and efficacy of a GLP-1 and glucagon receptor dual agonist mazdutide (IBI362) 9 mg and 10 mg in Chinese adults with overweight or obesity: a randomised, placebo-controlled, multiple-ascending-dose phase 1b trial. eClinicalMedicine. 2022;54:101691.
Enebo LB, Berthelsen KK, Kankam M, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of concomitant administration of multiple doses of cagrilintide with semaglutide 2.4 mg for weight management: a randomised, controlled, phase 1b trial. Lancet. 2021;397:1736–48.
Frias JP, Deenadayalan S, Erichsen L, et al. Efficacy and safety of co-administered once-weekly cagrilintide 2.4 mg with once-weekly semaglutide 2.4 mg in type 2 diabetes: a multicentre, randomised, double-blind, active-controlled, phase 2 trial. Lancet. 2023. https://doi.org/10.1016/S0140-6736(23)01163-7.
Urva S, Coskun T, Loh MT, et al. LY3437943, a novel triple GIP, GLP-1, and glucagon receptor agonist in people with type 2 diabetes: a phase 1b, multicentre, double-blind, placebo-controlled, randomised, multiple-ascending dose trial. Lancet. 2022;400:1869–81.
Medical Writing and Editorial Assistance.
Medical writing and editorial support for this article were provided by Dr Susan Cripps of Ward7, and was funded by Eli Lilly Australia.
Funding
The Rapid Service Fee for Diabetes Therapy publication was funded by Eli Lilly.
Author information
Authors and Affiliations
Contributions
Richard J MacIsaac and Roy Rasalam reviewed literature and developed concept and content. Gary Deed, Michael D’Emden, Elif I Ekinci, Samantha Hocking and Priya Sumithran contributed equally to discussing content, reviewing and commenting on the manuscript. Authors did not receive honoraria for their contributions.
Corresponding authors
Ethics declarations
Conflict of Interest
Richard MacIsaac: Has received research grants from Novo Nordisk, Servier, Medtronic, The Rebecca Cooper Medical Research Foundation, St Vincent’s Research Foundation, The Juvenile Diabetes Research Foundation, Grey Innovations, The Diabetes Australia Research Trust/Program and The National Health and Medical Research Council of Australia. Also received honoraria for lectures from Eli Lilly, Novo Nordisk, Sanofi Aventis, AstraZeneca, Merck Sharp & Dohme, Norvartis and Boehringer Ingelheim and has been or is on the advisory boards for Novo Nordisk, Boehringer Ingelheim-Eli Lilly Diabetes Alliance, AstraZeneca and Merck Shape and Dohme. Travel support has been supplied by Novo Nordisk, Sanofi, Boehringer Ingelheim and AstraZeneca. Has been a principal investigator for industry-sponsored clinical trials run by Novo Nordisk, Sanofi, Bayer, Johnson-Cilag and AbbVie. Gary Deed: Has provided Advisory Board consultancy to Eli Lilly regarding tirzepatide, has provided medical education consultancy or been on advisory boards for AstraZeneca, Boehringer Ingelheim, Eli Lilly Australia, MSD Australia, Novo Nordisk and Sanofi-Aventis Australia, and provides educational support in diabetes management. Michael D’Emden: Has received honoraria for attendance at national advisory boards, presentations and/or support to attend international meetings from Boehringer Ingelheim, Eli Lilly, AstraZeneca, Novartis, Abbott, Novo Nordisk, Servier and Bayer. Elif I. Ekinci: Has been a member of advisory boards for Eli Lilly, Sanofi, Pfizer, and Bayer; income received is donated to EE’s institution for diabetes research. Speakers fees for presentations for Eli Lilly, Bayer and Sanofi have been donated to EE’s institution for diabetes research. EE’s institution has received research funding from Eli Lilly, Boehringer, Sanofi, Novo Nordisk, Gilead and Insulet. Samantha Hocking: Has received research grants from Novo Nordisk, The Diabetes Australia Research Trust/Program and The National Health and Medical Research Council of Australia. Also received honoraria for lectures from Eli Lilly, Boehringer Ingelheim, Novo Nordisk, Sanofi Aventis, AstraZeneca, Gilead, Inova and Merck Sharp & Dohme and has been or is on the advisory boards for Novo Nordisk, Eli Lilly, AstraZeneca, Inova and Pfizer. Has been a principal investigator for industry-sponsored clinical trials run by Novo Nordisk, Eli Lilly, Boehringer Ingelheim and Merck Sharp & Dohme. Co-authorship of manuscripts assisted by medical writing from Novo Nordisk. Priya Sumithran: Has received research grants paid to the Institution from National Health and Medical Research Council. Co-authorship of manuscripts assisted by medical writing from Novo Nordisk. Roy Rasalam: Has provided medical education consultancy or been on advisory boards for AstraZeneca, Boehringer Ingelheim, Eli Lilly Australia, MSD Australia, Novo Nordisk and Sanofi-Aventis Australia.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
MacIsaac, R.J., Deed, G., D’Emden, M. et al. Challenging Clinical Perspectives in Type 2 Diabetes with Tirzepatide, a First-in-Class Twincretin. Diabetes Ther 14, 1997–2014 (2023). https://doi.org/10.1007/s13300-023-01475-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01475-5