Abstract
Introduction
The efficacy and safety of ertugliflozin have not been well characterized in Asian populations with type 2 diabetes (T2D) and overweight or obesity as defined by the Chinese Diabetes Society [body mass index (BMI) ≥ 24 kg/m2].
Methods
These post hoc analyses of pooled data from two randomized, double-blind, 26-week studies assessed the efficacy and safety of ertugliflozin (5 mg or 15 mg) compared with placebo in participants from Asia with T2D and baseline BMI ≥ 24 kg/m2, with inadequate glycemic control on metformin. Longitudinal analyses were used to calculate least squares (LS) mean [95% confidence interval (CI)] change from baseline in glycemic indices and body weight. The proportions of participants achieving efficacy targets and experiencing adverse events (AEs) were assessed.
Results
The 445 participants had a mean age of 55.5 years, T2D duration 6.6 years, glycated hemoglobin (HbA1c) 8.1%, and BMI 27.6 kg/m2. At week 26, placebo-adjusted LS mean (95% CI) changes from baseline for ertugliflozin 5 mg and 15 mg, respectively, were − 0.78% (− 0.95% to − 0.61%) and − 0.80% (− 0.98% to − 0.63%) for HbA1c, and − 1.74 kg (− 2.29 kg to − 1.19 kg) and − 2.04 kg (− 2.60 kg to − 1.48 kg) for body weight. A greater proportion of participants receiving ertugliflozin 5 mg and 15 mg versus placebo, respectively, achieved HbA1c < 7.0% (42.1% and 46.3% vs. 13.9%), body weight reduction ≥ 5% (35.5% and 38.3% vs. 11.1%), and systolic blood pressure < 130 mmHg (42.4% and 34.5% vs. 21.7%). The proportion of participants with AEs was 52.6% (ertugliflozin 5 mg), 52.3% (ertugliflozin 15 mg), and 55.6% (placebo).
Conclusions
In participants from Asia with T2D inadequately controlled by metformin monotherapy, and BMI ≥24 kg/m2, ertugliflozin (5 mg or 15 mg) resulted in greater glycemic and body weight reductions compared with placebo and was generally well tolerated.
Trial Registration
Clinicaltrials.gov identifiers NCT02033889, NCT02630706.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Asian populations have different associations between body mass index (BMI) and health risks than other populations, and so the definition of overweight or obesity differs. |
Ertugliflozin improves glycemic and metabolic control in people with type 2 diabetes (T2D) but its efficacy and safety have not been well characterized in Asian populations with T2D and overweight or obesity as defined by the Chinese Diabetes Society (BMI ≥24 kg/m2). |
These pooled post hoc analyses aimed to assess the efficacy and safety of ertugliflozin in a population from Asia with T2D, inadequately controlled by metformin monotherapy, and BMI ≥24 kg/m2. |
What was learned from the study? |
The analyses showed that for ertugliflozin (5 mg or 15 mg) versus placebo at week 26, reductions from baseline in HbA1c and body weight were greater, higher proportions of participants achieved glycated hemoglobin <7.0%, body weight reduction ≥5%, or systolic blood pressure <130 mmHg, and the incidence of adverse events was generally similar. |
With the increasing prevalence of diabetes with overweight/obesity in Asia, it is important to understand the efficacy and safety of therapies in this population, and these analyses showed that ertugliflozin (both doses) resulted in greater reductions in glycemic indices and body weight than placebo and was generally well tolerated. |
Introduction
The morbidity and mortality associated with type 2 diabetes (T2D) is a global problem [1]. The prevalence of both diabetes and obesity has increased across Asia in recent decades [2,3,4,5,6,7,8], with dietary, lifestyle, socioeconomic, ethnic, and cultural differences influencing regional differences [2, 9,10,11]. Compared with populations from Europe and the USA, people of Asian ancestry are at increased risk of T2D due to higher total and visceral adiposity, and are at high risk of complications [12, 13]. In Asia, as in other regions, metformin is generally recommended as first-line drug treatment for T2D, with other classes of antihyperglycemic agents, including sodium-glucose cotransporter 2 (SGLT2) inhibitors, added as indicated [14, 15]. The efficacy and safety of SGLT2 inhibitors in people from Asia with T2D have generally been established [16,17,18,19,20], but it is important to have data specific to those with overweight/obesity given the increasing prevalence of diabetes with overweight/obesity in Asia.
The selective SGLT2 inhibitor ertugliflozin is approved as an adjunct to diet and exercise to improve glycemic control in adults with T2D [21, 22]. The large global phase III VERTIS program in adults with T2D showed that when administered alone or in combination with metformin and/or sitagliptin, ertugliflozin significantly reduced glycated hemoglobin (HbA1c) and fasting plasma glucose (FPG) and was associated with reductions in body weight and blood pressure [23,24,25,26,27,28,29]. The VERTIS program included Asian participants, and the VERTIS ASIA study was conducted in people from Asia with T2D, confirming that ertugliflozin improved glycemic control and reduced body weight and blood pressure over 26 weeks when added to metformin in this population [30].
The efficacy and safety of ertugliflozin have been investigated in participants with T2D and a body mass index (BMI) of ≥ 25 kg/m2 [31]. This cutoff is based on the definitions of overweight (BMI ≥ 25 kg/m2) and obesity (BMI ≥ 30 kg/m2) widely used for Western populations [32]. Since Asian populations have different associations between BMI, percentage body fat, and health risks compared with Europeans [33], the Chinese Diabetes Society (CDS) defines overweight as BMI 24 kg/m2 to < 28 kg/m2 and obesity as BMI ≥ 28 kg/m2 [14, 34]. The efficacy and safety of ertugliflozin have not been well characterized in Asian populations with T2D and overweight or obesity as defined in Asian countries.
The aim of these analyses was to evaluate pooled data from two phase III studies, VERTIS MET [29] and VERTIS ASIA [30], to assess the efficacy and safety of ertugliflozin in a population from Asia with T2D and overweight or obesity (BMI ≥ 24 kg/m2), using definitions of overweight/obesity and efficacy targets recommended by the CDS [14, 15].
Methods
Study Design
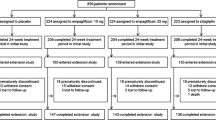
This was a post hoc analysis of pooled data from two randomized, double-blind, placebo-controlled 26-week studies with similar overall designs and enrollment criteria: VERTIS MET (NCT02033889) [29] was conducted in 14 countries/regions that included Australia, South Africa, USA, Hong Kong, and Taiwan, and VERTIS ASIA (NCT02630706) [30] was conducted in five countries/regions (mainland China, Philippines, Hong Kong, Republic of Korea, and Taiwan). During VERTIS MET (n = 621) [29] and VERTIS ASIA (n = 506) [30], a total of 1127 participants were randomized across all sites. Both studies were conducted in compliance with the ethical principles of the Declaration of Helsinki and all International Conference on Harmonisation Good Clinical Practice Guidelines. For each study, informed consent was obtained from participants, and the final protocol and informed consent documentation were reviewed and approved by the institutional review board or independent ethics committee at each investigational center [29, 30].
The study designs and eligibility criteria for VERTIS MET [29] and VERTIS ASIA [30] have been reported previously. Briefly, adults with T2D inadequately controlled with metformin monotherapy (HbA1c, 7.0–10.5% [53–91 mmol/mol] inclusive) were randomized to treatment with placebo, ertugliflozin 5 mg, or ertugliflozin 15 mg once daily for 26 weeks [29, 30]. Key inclusion criteria were a minimum BMI of 18 kg/m2 in both studies, with a maximum of 40 kg/m2 for VERTIS MET and no upper limit in VERTIS ASIA [29, 30]. Key exclusion criteria for both studies were body weight changes d≥ 5% in the previous 6 months associated with the use of a weight loss program, weight loss medication, or other medication associated with weight changes; and history of bariatric surgery.
In both studies, participants received glycemic rescue therapy (glimepiride) if they met (repeated and confirmed) prespecified FPG thresholds: > 270 mg/dL after randomization through week 6, > 240 mg/dL after week 6 through week 12, and > 200 mg/dL after week 12 through week 26. Counseling on appropriate dietary and lifestyle guidelines for T2D occurred at screening and participants were asked to maintain these guidelines throughout. Body weight was measured with a standardized digital scale, at approximately the same time of day after voiding, and the mean of duplicate readings used in the analysis. Sitting systolic blood pressure (SBP) was measured in triplicate with an automated oscillometric device. Laboratory analyses were performed at a central laboratory.
Participants
The current pooled analyses focused on adults with T2D inadequately controlled with metformin monotherapy, who identified as Asian race and were enrolled in either VERTIS MET or VERTIS ASIA, and who had a baseline BMI measurement of ≥ 24 kg/m2. This is the definition of overweight/obesity recommended by the CDS [14, 15]. The CDS definition was considered to be the most appropriate BMI cutoff for these analyses because the majority of the participants were from mainland China, and none were recruited in Malaysia, Singapore, or India. Additional analyses of those participants from Asia who were not eligible for the main analyses were conducted separately to cover the whole spectrum of body weights.
Study Measures
Efficacy analyses included changes from baseline in HbA1c and body weight, assessed at weeks 6, 12, 18, and 26, and changes from baseline in FPG and SBP, assessed at week 26. The proportions of participants meeting efficacy targets were assessed at week 26, including those with HbA1c < 7.0%, body weight reduction from baseline of ≥ 5%, or SBP < 130 mmHg. These clinical targets are recommended by the CDS [14, 15]. Changes from baseline in blood lipids, including triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C), were assessed at week 26.
Safety and tolerability were assessed on the basis of the incidences of adverse events (AEs), discontinuations due to AEs, serious adverse events (SAEs), and AEs of interest for SGLT2 inhibitors (symptomatic hypoglycemia, AEs of urinary tract infection, AEs of genital mycotic infection, and AEs of hypovolemia). AEs of interest for SGLT2 inhibitors were identified as such in the protocols, and sites were encouraged to report and treat them. Custom Medical Dictionary for Regulatory Activities (MedDRA) queries were used to define these AEs during the VERTIS program, the preferred terms for which have been reported previously [35]. For genital mycotic infection, the preferred terms included balanitis candida, balanoposthitis, balanoposthitis infective, erosive balanitis, gangrenous balanitis, genital candidiasis, genital infection, genital infection female, genital infection fungal, genital infection male, penile infection, vaginal infection, vaginal inflammation, vulvitis, vulvovaginal candidiasis, vulvovaginal mycotic infection, and vulvovaginitis [35]. For volume depletion, the preferred terms included blood pressure orthostatic decreased, circulatory collapse, dehydration, diastolic hypotension, dizziness postural, hypotension, hypovolemia, hypovolemic shock, orthostatic hypotension, orthostatic intolerance, postural orthostatic tachycardia syndrome, presyncope, shock, syncope, and urine output decreased [35].
Statistical Analyses
Analyses of pooled data for participants from Asia with baseline BMI ≥ 24.0 kg/m2 were conducted post hoc. Additional analyses of those participants from Asia who were excluded from the main analyses (i.e., with baseline BMI meeting the inclusion criteria for the two studies but < 24.0 kg/m2) were conducted separately. For both efficacy and safety analyses, data obtained after the initiation of glycemic rescue therapy were excluded.
Least squares (LS) mean changes from baseline in HbA1c, body weight, FPG, SBP, and blood lipids for each ertugliflozin group were calculated and compared with placebo using a constrained longitudinal data analysis model with fixed effects for study (VERTIS MET or VERTIS ASIA), treatment group, baseline estimated glomerular filtration rate (eGFR), study visit (i.e., time) as a categorical variable, and the interaction of visit and treatment group. Subgroup analyses according to baseline BMI (≥ 24 kg/m2 and < 28 kg/m2, and ≥ 28 kg/m2) were conducted similarly for LS mean changes from baseline in HbA1c, body weight, and SBP.
The proportion of participants who were responders at week 26, defined as meeting the efficacy targets HbA1c < 7%, body weight loss ≥ 5%, or SBP < 130 mmHg (among the subgroup with ≥ 130 mmHg at baseline), were analyzed using logistic regression models with fixed effects for treatment group, baseline value, baseline eGFR, and study, with multiple imputation for missing data.
The proportions of participants with ≥ 1 treatment-emergent AE, of all causalities, discontinuations from study medication due to AEs, and SAEs were calculated. The AEs of interest for SGLT2 inhibitors (symptomatic hypoglycemia, AEs of urinary tract infection, AEs of genital mycotic infection, and AEs of hypovolemia) were prespecified in the individual studies.
Results
Overall, 39.5% (445/1127) of the pooled participants in the two studies were Asian and had a baseline BMI d≥ 24 kg/m2 and so were eligible for inclusion in these post hoc analyses.
Demographics and Clinical Characteristics
The 445 participants from Asia with baseline BMI ≥ 24 kg/m2 included in the current analyses originated from VERTIS MET (n = 80) and VERTIS ASIA (n = 365), and in those studies they received ertugliflozin 5 mg (n = 152), ertugliflozin 15 mg (n = 149), or placebo (n = 144). They had a mean age of 55.5 years, duration of T2D 6.6 years, HbA1c 8.1%, and body weight 74.9 kg (Table 1). The mean baseline BMI for the population was 27.6 kg/m2; 60.7% of participants had BMI ≥ 24 kg/m2 and < 28 kg/m2, and 39.3% had BMI ≥ 28 kg/m2 (Table 1). Across the three treatment groups, the proportion of participants aged < 45 years ranged from 7.6% to 15.8%, and the proportion of female participants ranged from 38.3% to 49.3% (Table 1). Clinical characteristics were similar across the three treatment groups (Table 1).
Efficacy
Glycemic Control
At week 26, reductions from baseline in HbA1c were greater for ertugliflozin 5 mg and ertugliflozin 15 mg compared with placebo. The LS mean (95% CI) changes from baseline in HbA1c at week 26 were − 1.00% (− 1.13% to − 0.87%) for ertugliflozin 5 mg, − 1.02% (− 1.15% to − 0.90%) for ertugliflozin 15 mg, and − 0.22% (− 0.36% to − 0.08%) for placebo, with placebo-adjusted changes of − 0.78% (− 0.95% to − 0.61%) for ertugliflozin 5 mg and − 0.80% (− 0.98% to − 0.63%) for ertugliflozin 15 mg (Fig. 1A). Greater reduction in HbA1c with ertugliflozin, compared with placebo, was observed at the first post-baseline measurement (week 6) and continued throughout the treatment period (Fig. 2A). The LS mean changes from baseline in HbA1c at week 26 were similar for the subgroup with overweight and the subgroup with obesity (Fig. 3A) and were consistent with the main analyses.
Change from BL in A HbA1c, B FPG, C body weight, and D SBP at week 26 in the population from Asia with T2D and BMI ≥ 24 kg/m2. All randomized participants who took ≥ 1 dose of study medication and with ≥ 1 assessment after BL. Data obtained after the initiation of glycemic rescue therapy were excluded. Sample size shown is for LS mean change. For full BL data see Table 1. To convert FPG mg/dL to mmol/L, divide by 18.0182. aLS mean difference (95% CI) versus placebo. BL baseline, BMI body mass index, CI confidence interval, FPG fasting plasma glucose, HbA1c glycated hemoglobin, LS least squares, SBP systolic blood pressure, T2D type 2 diabetes
Change from BL in A HbA1c and B body weight through 26 weeks in the population from Asia with T2D and BMI ≥ 24 kg/m2. All randomized participants who took ≥ 1 dose of study medication and with ≥ 1 assessment after BL. Data obtained after the initiation of glycemic rescue therapy were excluded. For full BL data see Table 1. BL baseline, BMI body mass index, CI confidence interval, HbA1c glycated hemoglobin, LS least squares, T2D type 2 diabetes
Change from BL at week 26 in A HbA1c, B absolute body weight, C percentage change in body weight, and D SBP: subgroup analyses according to baseline BMI (≥ 24 kg/m2 and < 28 kg/m2, and ≥ 28 kg/m2) in the population from Asia with T2D. All randomized participants who took ≥ 1 dose of study medication and with ≥ 1 assessment after BL (and additionally at BL for the percent body weight analysis). Data obtained after the initiation of glycemic rescue therapy were excluded. Sample sizes (for LS mean changes) for subgroup with BMI ≥ 24 kg/m2 and < 28 kg/m2, n = 80 (placebo), n = 91 (ertugliflozin 5 mg), and n = 91 (ertugliflozin 15 mg); and subgroup with BMI ≥ 28 kg/m2, n = 59 (placebo), n = 59 (ertugliflozin 5 mg), and n = 55 (ertugliflozin 15 mg). At BL, in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively, mean (SD) HbA1c was 8.19 (0.95)%, 8.01 (0.85)%, and 8.04 (0.97)% in the subgroup with BMI ≥ 24 kg/m2 and < 28 kg/m2 and 8.17 (0.84)%, 8.27 (0.96)%, and 8.19 (0.88)% in the subgroup with BMI ≥ 28 kg/m2. Similarly, respectively, mean (SD) body weight was 70.04 (8.79) kg, 70.05 (6.93) kg, and 71.29 (7.44) kg in the subgroup with BMI ≥ 24 kg/m2 and < 28 kg/m2, and 82.17 (10.36) kg, 82.24 (10.81) kg, and 81.01 (9.44) kg in the subgroup with BMI ≥ 28 kg/m2; and mean (SD) SBP was 128.29 (12.62) mmHg, 126.19 (12.42) mmHg, and 127.50 (12.00) mmHg in the subgroup with BMI ≥ 24 kg/m2 and < 28 kg/m2, and 133.17 (14.73) mmHg, 130.31 (13.13) mmHg, and 128.52 (11.70) mmHg in the subgroup with BMI ≥ 28 kg/m2. aLS mean difference (95% CI) versus placebo. BL baseline, BMI body mass index, CI confidence interval, HbA1c glycated hemoglobin, LS least squares, SBP systolic blood pressure, SD standard deviation, T2D type 2 diabetes
A greater proportion of participants in the ertugliflozin 5 mg (42.1%, 64/152) and ertugliflozin 15 mg (46.3%, 69/149) groups, compared with the placebo group (13.9%, 20/144), achieved HbA1c < 7.0% at week 26 (Fig. 4A), with adjusted odds ratios (95% CI) relative to placebo of 5.75 (3.14–10.54) for ertugliflozin 5 mg and 6.89 (3.68–12.87) for ertugliflozin 15 mg.
Proportion of participants with A HbA1c < 7%, B body weight reduction ≥ 5%, and C SBP < 130 mmHg (in those with baseline measurement ≥ 130 mmHg) at week 26 in the population from Asia with T2D and BMI ≥ 24 kg/m2. Observed data, with missing data counted as nonresponders. All randomized participants who took ≥ 1 dose of study medication and with ≥ 1 measurement at or after baseline. Data obtained after the initiation of glycemic rescue therapy were excluded. BMI body mass index, HbA1c glycated hemoglobin, SBP systolic blood pressure, T2D type 2 diabetes
At week 26, reductions from baseline in FPG were greater for ertugliflozin 5 mg and ertugliflozin 15 mg compared with placebo. The LS mean (95% CI) changes from baseline in FPG at week 26 were − 36.48 mg/dL (− 41.20 mg/dL to − 31.76 mg/dL) for ertugliflozin 5 mg, − 36.70 mg/dL (− 41.43 mg/dL to − 31.97 mg/dL) for ertugliflozin 15 mg, and − 8.40 mg/dL (− 13.37 mg/dL to − 3.43 mg/dL) for placebo, with placebo-adjusted changes of − 28.08 mg/dL (− 33.88 mg/dL to − 22.29 mg/dL) for ertugliflozin 5 mg and − 28.30 mg/dL (− 34.14 mg/dL to − 22.46 mg/dL) for ertugliflozin 15 mg (Fig. 1B).
Body Weight
At week 26, reductions from baseline in body weight were greater for ertugliflozin 5 mg and ertugliflozin 15 mg compared with placebo. The LS mean (95% CI) changes from baseline in absolute body weight at week 26 were − 3.00 kg (− 3.40 kg to − 2.61 kg) for ertugliflozin 5 mg, − 3.30 kg (− 3.70 kg to − 2.91 kg) for ertugliflozin 15 mg, and − 1.26 kg (− 1.68 kg to − 0.84 kg) for placebo, with placebo-adjusted changes of − 1.74 kg (− 2.29 kg to − 1.19 kg) for ertugliflozin 5 mg and − 2.04 kg (− 2.60 kg to − 1.48 kg) for ertugliflozin 15 mg (Fig. 1C). Greater reduction in absolute body weight with ertugliflozin, compared with placebo, was observed at the first post-baseline measurement (week 6) and continued throughout the treatment period (Fig. 2B). The LS mean (95% CI) percent changes from baseline in body weight at week 26 were − 4.07% (− 4.61% to − 3.53%) for ertugliflozin 5 mg, − 4.44% (− 4.98% to − 3.90%) for ertugliflozin 15 mg, and − 1.70% (− 2.27% to − 1.13%) for placebo, with placebo-adjusted changes of − 2.37% (− 3.12% to − 1.62%) for ertugliflozin 5 mg and − 2.74% (− 3.50% to − 1.98%) for ertugliflozin 15 mg. The subgroup analyses showed significant reductions in body weight with ertugliflozin versus placebo at week 26 for the subgroup with overweight and the subgroup with obesity, with a larger placebo response in those with obesity (Fig. 3B, C).
A greater proportion of participants in the ertugliflozin 5 mg (35.5%, 54/152) and ertugliflozin 15 mg (38.3%, 57/149) groups, compared with the placebo group (11.1%, 16/144), achieved body weight reduction ≥ 5% at week 26 (Fig. 4B), with adjusted odds ratios (95% CI) relative to placebo of 4.16 (2.26–7.65) for ertugliflozin 5 mg and 5.22 (2.79–9.76) for ertugliflozin 15 mg.
Blood Pressure
At week 26, reductions from baseline in SBP were greater for ertugliflozin 5 mg and ertugliflozin 15 mg compared with placebo. The LS mean (95% CI) changes from baseline in SBP at week 26 were − 4.78 mmHg (− 6.67 mmHg to − 2.88 mmHg) for ertugliflozin 5 mg, − 4.50 mmHg (− 6.40 mmHg to − 2.59 mmHg) for ertugliflozin 15 mg, and − 0.28 mmHg (− 2.29 mmHg to 1.73 mmHg) for placebo, with placebo-adjusted changes of − 4.50 mmHg (− 7.10 mmHg to − 1.89 mmHg) for ertugliflozin 5 mg and − 4.22 mmHg (− 6.84 mmHg to − 1.59 mmHg) for ertugliflozin 15 mg (Fig. 1D). The LS mean changes from baseline in SBP at week 26 were similar for the subgroup with overweight and the subgroup with obesity (Fig. 3D) and were generally consistent with the main analyses, although the reduction did not reach significance for ertugliflozin 15 mg versus placebo in the subgroup with baseline BMI ≥ 28 kg/m2.
In those participants with SBP ≥ 130 mmHg at baseline, a greater proportion in the ertugliflozin 5 mg (42.4%, 28/66) and ertugliflozin 15 mg (34.5%, 20/58) groups, compared with the placebo group (21.7%, 15/69), achieved SBP < 130 mmHg at week 26 (Fig. 4C), with adjusted odds ratios (95% CI) relative to placebo of 2.32 (1.08–4.97) for ertugliflozin 5 mg and 1.60 (0.71–3.57) for ertugliflozin 15 mg.
Lipids
Small changes from baseline at week 26 were seen in triglycerides, total cholesterol, LDL-C, and HDL-C (Fig. 5).
Change from BL in A triglycerides, B total cholesterol, C LDL-C, and D HDL-C at week 26 in the population from Asia with T2D and BMI ≥ 24 kg/m2. All randomized participants who took ≥ 1 dose of study medication and with ≥ 1 assessment after BL. Data obtained after the initiation of glycemic rescue therapy were excluded. Sample size shown is for LS mean change. For full BL data see Table 1. aLS mean difference (95% CI) versus placebo. BL baseline, BMI body mass index, CI confidence interval, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, LS least squares, T2D type 2 diabetes
Safety
The proportion of participants with AEs was 52.6%, 52.3%, and 55.6% in the ertugliflozin 5 mg, ertugliflozin 15 mg, and placebo groups, respectively (Table 2). Discontinuations from study medication due to AEs occurred in 1.3% of participants in each of the ertugliflozin groups and 2.8% of participants in the placebo group (Table 2). SAEs occurred in 5.9% of participants in the ertugliflozin 5 mg group and 7.4% in the ertugliflozin 15 mg group, compared with 2.1% in the placebo group (Table 2) with no apparent pattern (data not shown). The incidence of AEs of interest for SGLT2 inhibitors is shown in Table 2.
Analyses of Participants from Asia with Baseline BMI < 24 kg/m2
Analyses of the 161 participants from Asia with baseline BMI meeting the inclusion criteria for the two studies but < 24 kg/m2 (Tables S1–S5 in the supplementary material) were generally consistent with the main analyses with regards to the efficacy and safety of ertugliflozin 5 mg or 15 mg versus placebo. In this population, BMI (rounded) was 19–24 kg/m2 (Table S1).
Discussion
These analyses from the VERTIS phase III program showed that, in participants from Asia with T2D inadequately controlled on metformin and with overweight/obesity (BMI ≥ 24 kg/m2) as defined by the CDS [14, 15], ertugliflozin resulted in greater glycemic and body weight reductions than placebo. Compared with placebo, more participants receiving ertugliflozin achieved the targets for glycemic control, weight loss, and blood pressure recommended by the CDS [14, 15]. The efficacy and safety of ertugliflozin in participants from Asia with T2D and BMI ≥ 24 kg/m2 were consistent with data for the overall VERTIS phase III clinical trial program [35, 36] and overall populations from Asia [30, 37].
Reductions in HbA1c were evident as early as week 6 and persisted through all subsequent visits in this 26-week analysis. More participants receiving ertugliflozin achieved the target HbA1c < 7% at week 26 compared with placebo. The magnitude of placebo-adjusted reductions from baseline in HbA1c with ertugliflozin was similar to the results of previous pooled analyses of ertugliflozin study participants with BMI ≥ 25 kg/m2 [31]. The glycemic efficacy of SGLT2 inhibitors is independent of baseline BMI [31, 38], supporting the current findings of similar HbA1c reductions for the subgroup with overweight and the subgroup with obesity, as well as the population with BMI < 24 kg/m2.
Reductions in body weight were evident at week 6 and persisted through all later study visits. The placebo-adjusted reductions in absolute body weight with ertugliflozin in the current population were similar to those reported previously for the pooled ertugliflozin study participants with BMI ≥ 25 kg/m2 [31]. The proportion of ertugliflozin-treated participants who achieved the target of ≥ 5% body weight reduction at week 26 was, however, notably higher (35.5–38.3%) in the current analyses compared with that reported for the population with BMI ≥ 25 kg/m2 (28.1–28.5%) [31], with a similar placebo response. Both those with overweight and those with obesity experienced greater weight loss with ertugliflozin than with placebo. Similar changes from baseline in absolute body weight were observed with ertugliflozin in both subgroups. While the larger placebo response in the subgroup with obesity suggests a lower placebo-adjusted percent change in body weight than in the subgroup with overweight, the findings should be interpreted with caution because of the small sample size. Previously, it was reported that percentage body weight reduction was similar across BMI subgroups [31]. It is feasible that ethnicity and/or culture could influence the likelihood of achieving body weight goals. Weight loss was progressive through 26 weeks in the current analyses.
As with other populations with T2D, people from Asia often have concomitant hypertension [39]. The current analyses found that SBP was reduced at week 26 with ertugliflozin, and more participants receiving ertugliflozin achieved the SBP target < 130 mmHg at week 26, compared with placebo. Similar findings were reported for the pooled population with BMI ≥ 25 kg/m2 [31].
Both doses of ertugliflozin were generally well tolerated in this population from Asia with T2D and overweight or obesity. The proportion of participants with AEs was generally similar across the three groups (52.3–55.6%) and AEs were consistent with the tolerability reported previously for the pooled population with BMI ≥ 25 kg/m2 [31]. The proportion of participants with SAEs was 5.9–7.4% in the ertugliflozin groups compared with 2.1% for placebo, consistent with the overall VERTIS ASIA study population [30] and with no apparent pattern in terms of system organ class evident. The incidence of AEs of interest for SGLT2 inhibitors was generally consistent with the existing safety data for ertugliflozin [35].
These analyses provide data for ertugliflozin added on to metformin in Asian participants with T2D and overweight or obesity that help to inform clinical practice. On the basis of these efficacy and safety data, ertugliflozin could be considered as a component of the treatment of patients with T2D and overweight or obesity in Asian countries where ertugliflozin has been approved.
Although a large number of studies of SGLT2 inhibitors have been conducted in Asian populations with T2D [16], many are not specific to participants with overweight/obesity. Where obesity is an inclusion criterion, a regional definition of obesity [40] can complicate comparisons with other studies. A dapagliflozin study utilized the CDS cutoffs for obesity but was active-controlled [41]. Considering the prevalence of overweight/obesity in people with T2D this may explain the lack of specific data.
This study has limitations. The analyses were post hoc, some of the sample sizes were small, and the duration of follow-up was 26 weeks. The VERTIS MET study had a 78-week extension [42] but not the VERTIS ASIA study [30] so pooling beyond week 26 to assess longer-term efficacy and safety was not possible for the current analyses. Nonetheless, long-term efficacy and safety were observed with ertugliflozin through 104 weeks in the overall VERTIS MET population [42]. As a result of geographical limitations, the population studied herein was not representative of the entire Asian population. The VERTIS MET and VERTIS ASIA clinical trials did not recruit from sites in South Asia.
Conclusions
In this pooled analysis of participants from Asia with T2D inadequately controlled by metformin monotherapy and with overweight or obesity (BMI ≥ 24 kg/m2), treatment with ertugliflozin (5 mg or 15 mg) resulted in greater glycemic and body weight reductions than placebo at week 26. Additionally, more participants receiving ertugliflozin achieved their metabolic goals compared with placebo at week 26. Ertugliflozin was generally well tolerated.
References
Safiri S, Karamzad N, Kaufman JS, et al. Prevalence, deaths and disability-adjusted-life-years (DALYs) due to type 2 diabetes and its attributable risk factors in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. Front Endocrinol (Lausanne). 2022;13: 838027.
Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–40.
Hills AP, Arena R, Khunti K, et al. Epidemiology and determinants of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. 2018;6:966–78.
Ruan Y, Yan QH, Xu JY, et al. Epidemiology of diabetes in adults aged 35 and older from Shanghai, China. Biomed Environ Sci. 2016;29:408–16.
Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369: m997.
Wang L, Peng W, Zhao Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326:2498–506.
Yuan H, Li X, Wan G, et al. Type 2 diabetes epidemic in East Asia: a 35-year systematic trend analysis. Oncotarget. 2018;9:6718–27.
Sun X, Yan AF, Shi Z, et al. Health consequences of obesity and projected future obesity health burden in China. Obesity (Silver Spring). 2022;30:1724–51.
Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408–18.
Wu H, Meng X, Wild SH, Gasevic D, Jackson CA. Socioeconomic status and prevalence of type 2 diabetes in mainland China, Hong Kong and Taiwan: a systematic review. J Glob Health. 2017;7: 011103.
Vijayakumar V, Mavathur R, Sharma MNK. Ethnic disparity and increased prevalence of type 2 diabetes among south Asians: aetiology and future implications for diabetes prevention and management. Curr Diabetes Rev. 2018;14:518–22.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann NY Acad Sci. 2013;1281:64–91.
Gujral UP, Pradeepa R, Weber MB, Narayan KM, Mohan V. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann NY Acad Sci. 2013;1281:51–63.
Jia W, Weng J, Zhu D, et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev. 2019;35: e3158.
Chinese Diabetes Society. [Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition)] 中国2型糖尿病防治指南 (2020年版). Chin J Diabetes Mellitus. 2021;13:315–409 [Article in Chinese].
Sheu WHH, Chan SP, Matawaran BJ, et al. Use of SGLT-2 inhibitors in patients with type 2 diabetes mellitus and abdominal obesity: an Asian perspective and expert recommendations. Diabetes Metab J. 2020;44:11–32.
Khoo CM, Deerochanawong C, Chan SP, et al. Use of sodium-glucose co-transporter-2 inhibitors in Asian patients with type 2 diabetes and kidney disease: an Asian perspective and expert recommendations. Diabetes Obes Metab. 2021;23:299–317.
Deerochanawong C, Chan SP, Matawaran BJ, et al. Use of sodium-glucose co-transporter-2 inhibitors in patients with type 2 diabetes mellitus and multiple cardiovascular risk factors: an Asian perspective and expert recommendations. Diabetes Obes Metab. 2019;21:2354–67.
Gan S, Dawed AY, Donnelly LA, et al. Efficacy of modern diabetes treatments DPP-4i, SGLT-2i, and GLP-1RA in white and Asian patients with diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2020;43:1948–57.
Scheen AJ. SGLT2 inhibitors as add-on therapy to metformin for people with type 2 diabetes: a review of placebo-controlled trials in Asian versus non-Asian patients. Diabetes Metab Syndr Obes. 2020;13:2765–79.
European Medicines Agency. Steglatro™ (Ertugliflozin) Summary of Product Characteristics. Hoddesdon, UK; 2018.
US Food and Drug Administration. Steglatro™ (Ertugliflozin) Prescribing Information. Whitehouse Station, NJ; 2017.
Dagogo-Jack S, Liu J, Eldor R, et al. Efficacy and safety of the addition of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sitagliptin: The VERTIS SITA2 placebo-controlled randomized study. Diabetes Obes Metab. 2018;20:530–40.
Grunberger G, Camp S, Johnson J, et al. Ertugliflozin in patients with stage 3 chronic kidney disease and type 2 diabetes mellitus: the VERTIS RENAL randomized study. Diabetes Ther. 2018;9:49–66.
Hollander P, Liu J, Hill J, et al. Ertugliflozin compared with glimepiride in patients with type 2 diabetes mellitus inadequately controlled on metformin: the VERTIS SU randomized study. Diabetes Ther. 2018;9:193–207.
Miller S, Krumins T, Zhou H, et al. Ertugliflozin and sitagliptin co-initiation in patients with type 2 diabetes: the VERTIS SITA randomized study. Diabetes Ther. 2018;9:253–68.
Pratley RE, Eldor R, Raji A, et al. Ertugliflozin plus sitagliptin versus either individual agent over 52 weeks in patients with type 2 diabetes mellitus inadequately controlled with metformin: The VERTIS FACTORIAL randomized trial. Diabetes Obes Metab. 2018;20:1111–20.
Terra SG, Focht K, Davies M, et al. Phase III, efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diabetes Obes Metab. 2017;19:721–8.
Rosenstock J, Frias J, Páll D, et al. Effect of ertugliflozin on glucose control, body weight, blood pressure and bone density in type 2 diabetes mellitus inadequately controlled on metformin monotherapy (VERTIS MET). Diabetes Obes Metab. 2018;20:520–9.
Ji L, Liu Y, Miao H, et al. Safety and efficacy of ertugliflozin in Asian patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy: VERTIS Asia. Diabetes Obes Metab. 2019;21:1474–82.
Heymsfield SB, Raji A, Gallo S, et al. Efficacy and safety of ertugliflozin in patients with overweight and obesity with type 2 diabetes mellitus. Obesity (Silver Spring). 2020;28:724–32.
World Health Organization. Factsheet: obesity and overweight, June 9, 2021. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Accessed 19 Aug 2022.
World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96.
Patel S, Hickman A, Frederich R, et al. Safety of ertugliflozin in patients with type 2 diabetes mellitus: pooled analysis of seven phase 3 randomized controlled trials. Diabetes Ther. 2020;11:1347–67.
Liu J, Tarasenko L, Terra SG, et al. Efficacy of ertugliflozin in monotherapy or combination therapy in patients with type 2 diabetes: a pooled analysis of placebo-controlled studies. Diab Vasc Dis Res. 2019;16:415–23.
Liu J, Patel S, Cater NB, et al. Efficacy and safety of ertugliflozin in East/Southeast Asian patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2020;22:574–82.
Cai X, Yang W, Gao X, Zhou L, Han X, Ji L. Baseline body mass index and the efficacy of hypoglycemic treatment in type 2 diabetes: a meta-analysis. PLoS ONE. 2016;11: e0166625.
So WY, Raboca J, Sobrepena L, et al. Comprehensive risk assessments of diabetic patients from seven Asian countries: The Joint Asia Diabetes Evaluation (JADE) program. J Diabetes. 2011;3:109–18.
Yokote K, Sano M, Tsumiyama I, Keefe D. Dose-dependent reduction in body weight with LIK066 (licogliflozin) treatment in Japanese patients with obesity. Diabetes Obes Metab. 2020;22:1102–10.
Zhaohu H, Xiao H, Hailin S, Feng H. Efficacy and safety of dapagliflozin versus liraglutide in patients with overweight or obesity and type 2 diabetes mellitus: a randomised controlled clinical trial in Tianjin, China. J Diabetes Res. 2022;2022:4126995.
Gallo S, Charbonnel B, Goldman A, et al. Long-term efficacy and safety of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy: 104-week VERTIS MET trial. Diabetes Obes Metab. 2019;21:1027–36.
Acknowledgments
Medical writing support was provided by Kim Russell, PhD, of Engage Scientific Solutions (Horsham, UK) and was funded by Merck Sharp & Dohme LLC., a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, in collaboration with Pfizer Inc., New York, NY, USA. The authors would like to thank the participants of both studies.
Funding
This analysis was sponsored by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA in collaboration with Pfizer Inc., New York, NY, USA. Publication fees (expenses to the journal for Rapid Service) were funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA in collaboration with Pfizer Inc., New York, NY, USA.
Authorship
Linong Ji, Jie Liu, Zhi Jin Xu, Zhiqi Wei, Ruya Zhang, Seema Malkani, Nilo B. Cater and Robert Frederich meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Linong Ji, Jie Liu, Zhi Jin Xu, Zhiqi Wei, Ruya Zhang, Seema Malkani, Nilo B. Cater and Robert Frederich contributed to the acquisition, analysis, or interpretation of the data, and had full access to all of the data. Linong Ji, Jie Liu, Zhi Jin Xu, Zhiqi Wei, Ruya Zhang, Seema Malkani, Nilo B. Cater and Robert Frederich contributed to drafting the manuscript and revising it critically for important intellectual content. Linong Ji, Jie Liu, Zhi Jin Xu, Zhiqi Wei, Ruya Zhang, Seema Malkani, Nilo B. Cater and Robert Frederich approved the final version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Prior Presentation
Some of these data were presented at the International Diabetes Federation World Diabetes Congress, Lisbon, Portugal, December 5–8, 2022.
Disclosures
Linong Ji declares no conflict of interest. Zhiqi Wei and Ruya Zhang are employees of MSD China. Seema Malkani, Zhi Jin Xu, and Jie Liu are employees of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA and own stock in Merck & Co., Inc., Rahway, NJ, USA. Robert Frederich and Nilo B. Cater are employees and shareholders of Pfizer Inc.
Compliance with Ethics Guidelines
Both studies contributing data to this pooled analysis were conducted in compliance with the ethical principles of the Declaration of Helsinki and all International Conference on Harmonisation Good Clinical Practice Guidelines. For each study, informed consent was obtained from participants and the final protocol and informed consent documentation were reviewed and approved by the institutional review board or independent ethics committee at each investigational center.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Open Access
This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ji, L., Liu, J., Xu, Z.J. et al. Efficacy and Safety of Ertugliflozin Added to Metformin: A Pooled Population from Asia with Type 2 Diabetes and Overweight or Obesity. Diabetes Ther 14, 319–334 (2023). https://doi.org/10.1007/s13300-022-01345-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01345-6