Abstract
Introduction
Previous studies suggested that β-cell function markers such as fasting and postprandial serum C-peptide and C-peptide increment (FCPR, PCPR, and ΔCPR, respectively) may be useful in estimating glycemic response to glucagon-like peptide-1 receptor agonists. However, it remains elusive whether baseline glycemic control confounds these markers. Here we aimed to identify the least confounded β-cell function markers and investigate whether these markers could predict glycemic response to dulaglutide.
Methods
We evaluated FCPR, PCPR, and ΔCPR levels in patients with type 2 diabetes who initiated dulaglutide treatment after a standardized meal tolerance test (MTT). We first investigated the confounding effects of baseline HbA1c on β-cell function markers using Pearson’s correlation test. Then, we evaluated the association between each β-cell function marker and glycemic response (HbA1c change 0–6 months) to dulaglutide using generalized linear model and logistic regression analysis with adjustment for baseline HbA1c.
Results
In 141 patients, baseline HbA1c was significantly inversely correlated with PCPR and ΔCPR (P < 0.01 for both) but not with FCPR (r = 0.02; P = 0.853), suggesting that FCPR was the marker least confounded by baseline glycemic control. Of all patients, 59 continued dulaglutide for at least 6 months without initiating any additional glucose-lowering medications. Mean ± SE HbA1c change 0–6 months was − 1.16 ± 0.17% (P < 0.001 vs. baseline). The β-cell function markers were significantly associated with HbA1c change 0–6 months in the generalized linear model. FCPR was also a significant predictor for achieving a reduction in HbA1c of at least 1% (P = 0.044) with an area under the receiver operating characteristic curve of 0.83 (sensitivity = 0.81 and specificity = 0.79).
Conclusion
Fasting and meal-induced C-peptide levels are associated with glycemic response to dulaglutide, among which FCPR is least confounded by baseline glycemic control, suggesting its utility as a marker for glycemic response to dulaglutide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Previous studies reported that β-cell function markers, such as fasting and meal-induced C-peptide levels, might be useful in estimating the efficacy of glucagon-like peptide-1 receptor agonists. |
However, the following questions remain unanswered: Are these markers confounded by baseline glycemic control, and if so, what is the least confounded marker? What is the association between that marker and glycemic response to dulaglutide, a widely used glucagon-like peptide-1 receptor agonists? |
We aimed to (i) investigate the confounding effect of baseline glycemic control on the β-cell function markers to determine the least confounded marker and (ii) investigate whether the β-cell function markers are associated with HbA1c-lowering effects of dulaglutide, exploring a suitable marker of glycemic response to dulaglutide. |
What was learned from this study? |
Meal-induced C-peptide levels (PCPR and ΔCPR) were significantly affected by baseline glycemic control, whereas fasting C-peptide (FCPR) was not, suggesting that FCPR was the marker least confounded by baseline glycemic control. |
FCPR, PCPR, and ΔCPR were significantly associated with glycemic response to dulaglutide. Furthermore, FCPR was a significant predictor for achieving a reduction in HbA1c of at least 1%, suggesting its utility as a marker for glycemic response to dulaglutide in clinical settings. |
Introduction
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) stimulate insulin secretion from β-cells in a glucose-dependent manner [1]. Although GLP-1RAs have been widely used in clinical settings, the treatment response to GLP-1RAs is highly variable [2]. Therefore, identifying clinical markers predictive of glycemic response to GLP-1RAs is of critical importance.
Previous studies have shown that the glycemic response to several GLP-1RAs, mainly liraglutide or exenatide, is positively associated with β-cell function markers, such as fasting C-peptide (FCPR) [3,4,5,6,7] and postprandial C-peptide (PCPR) serum levels [7, 8]. However, clinical measurements can be confounded by baseline glycemic control, especially chronic hyperglycemia [9, 10]; thus, appropriate surrogates that are minimally influenced by baseline glycemic control are warranted in clinical settings. Furthermore, there are few studies on the relationship between clinical markers and glycemic response to dulaglutide despite its wide usage.
In the present study, we aimed to investigate the influence of baseline HbA1c (glycated hemoglobin) on β-cell function markers to determine the least confounded marker. In addition, we aimed to evaluate whether the β-cell function markers were associated with the HbA1c-lowering effects of dulaglutide to identify a suitable marker of glycemic response to dulaglutide.
Methods
Study Design and Participants
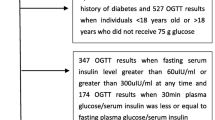
A schematic diagram of the inclusion and exclusion workflow of study patients is presented in Fig. 1. We studied the data of 141 patients with type 2 diabetes (T2D) who initiated dulaglutide treatment (0.75 mg) at the discretion of the physician in charge as part of usual diabetes care within 1 week after undergoing a standardized meal tolerance test (MTT) between September 2015 and December 2019 at the Tazuke Kofukai Medical Research Institute, Kitano Hospital, Osaka, Japan. At our institution, the MTT is performed on the second day of hospital admission for nonemergent glycemic control as routine clinical practice. Relevant data were collected retrospectively. Our study excluded patients with pancreatic or liver disease, a history of previous use of other classes of GLP-1RAs, endocrine disorders that can cause hyperglycemia, estimated glomerular filtration rate (eGFR) of no greater than 30 mL/min/1.73 m2, or anti-glutamic acid decarboxylase antibodies, as well as those taking agents known to promote hyperglycemia such as glucocorticoids. Physical examination and laboratory evaluation were performed at the baseline before the initiation of dulaglutide treatment and the MTT. All patients who had previously received dipeptidyl peptidase-4 (DPP-4) inhibitors stopped receiving them 1 day before the initiation of dulaglutide treatment. The present study was performed in accordance with the Declaration of Helsinki and approved by the local ethics board committee of Kitano Hospital (No. 1807005, approved on April 8, 2020). Informed consent was waived because of the retrospective nature of this study.
First-Step Analysis: Confounding Effects of Baseline HbA1c on Clinical β-Cell Function Markers
Pearson’s product-moment correlation coefficient (r) was calculated to determine correlations between baseline HbA1c and the β-cell function markers (FCPR, PCPR, and C-peptide increment [ΔCPR]). Pearson’s correlation test results with a P value less than 0.05 were considered as significant correlations, indicating the confounding effect of baseline glycemic control on the marker.
Second-Step Analysis: Association Between the β-Cell Function Markers and Glycemic Response to Dulaglutide
Second, we analyzed the association between the β-cell function markers and the treatment response to dulaglutide (HbA1c change 0–6 months, defined as a change from baseline HbA1c to HbA1c at 6 months) in the remaining patients who continued dulaglutide for at least 6 months without initiating any additional glucose-lowering medications.
Generalized Linear Model Analysis
We assessed the relationship between each variable (sex, age, body mass index [BMI], duration of T2D, fasting plasma glucose [FPG], postprandial plasma glucose [PPG], FCPR, PCPR, ΔCPR, high-density lipoprotein [HDL] cholesterol, and triglycerides) and the treatment response using a generalized linear model with adjustment for baseline HbA1c as a covariate. We also evaluated additional variables, including fasting immunoreactive insulin, homeostasis model assessment of β-cell function (HOMA2-%β), and homeostasis model assessment of insulin sensitivity (HOMA2-%S), in non-insulin-treated patients. We adjusted HbA1c change 0–6 months for baseline HbA1c as recommended previously, considering that a higher baseline HbA1c level denotes a greater response to glucose-lowering therapies [11,12,13].
Logistic Regression Analysis
We also conducted logistic regression to evaluate the association between HbA1c change 0–6 months and each β-cell function marker with adjustment for baseline HbA1c as a covariate.
Patients with an HbA1c change 0–6 months of at least 1% were defined as good responders and those with an HbA1c change 0–6 months of less than 1% as poor responders. For logistic regression, C-peptide measurements were standardized to have unit variance to enable comparisons of their odds ratios [14].
For both analyses, HbA1c changes at 3 and 6 months were defined as 12 ± 1 and 24 ± 1 weeks, respectively, after the initiation of dulaglutide treatment. The last valid observation between 3 and 6 months was carried forward to 6 months only if the patients were missing HbA1c at 6 months and continued dulaglutide for at least 6 months; otherwise, the patients were excluded from further analysis. To ensure the validity of the last observation carried forward (LOCF) approach, we evaluated whether HbA1c changes from baseline to 3 months (HbA1c change 0–3 months) and 6 months were not significantly different, using the paired t test.
Additional Analysis: Cotreatment Changes
To rule out the confounding effect of changes in cotreatment on HbA1c change 0–6 months, we evaluated whether oral antidiabetic agent (OAD) dose changes/discontinuation during months 0–6 significantly affected HbA1 change 0–6 months using the unpaired t test. We used a univariable linear regression with HbA1c change 0–6 months as a dependent variable and insulin dose change as a continuous independent variable to evaluate the association between insulin dose change and HbA1c change 0–6 months.
Additional Analysis: Baseline OAD Use and β-Cell Function Markers
To assess the influence of baseline OADs use on β-cell function markers in the remaining patients who continued dulaglutide, we evaluated whether each OAD use affected C-peptide levels in the MTT using the unpaired t test. For the OAD significantly associated with β-cell function markers, we additionally evaluated the relationship between HbA1c change 0–6 months and each β-cell function marker, with baseline HbA1c and the OAD use as covariates, to investigate the confounding effects of baseline OAD use on the results of the second-step analysis.
Measurements
After the patients fasted overnight for at least 10 h, MTT was carried out to determine FCPR, PCPR, and ΔCPR serum levels in the MTT. PCPR was measured 2 h after a standardized test meal load, and ΔCPR was calculated according to the following formula: ΔCPR = PCPR − FCPR. Serum C-peptide was measured using a chemiluminescent immunoassay kit (Siemens Healthcare Diagnostics, Tokyo, Japan). HbA1c was measured using the latex agglutination inhibition method. The results are shown as National Glycohemoglobin Standardization Program values. The standardized test meal included 460 kcal, consisting of 60% carbohydrates, 10% protein, and 30% fat. Other laboratory measurements, including plasma glucose, were measured using standard assays.
Statistical Analysis
All analyses were performed using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria), and results with P < 0.05 were considered statistically significant.
Results
Baseline Characteristics
We identified 141 patients eligible for the first-step analysis who initiated dulaglutide treatment after the MTT in which FCPR, PCPR, and ΔCPR were measured. For the second-step analysis, 59 patients who continued dulaglutide for at least 6 months without initiating any additional glucose-lowering agents were included. For patients excluded from the second-step analysis, reasons for exclusion were discontinuation of dulaglutide within 6 months of the initiation, initiation of the new glucose-lowering medications, or loss to follow-up. Further details are provided in Supplementary Table 1. The baseline characteristics of all 141 patients for the first-step analysis and 59 for the second-step analysis are shown in Tables 1 and 2, respectively.
First-Step Analysis: Confounding Association Between Baseline HbA1c and Clinical β-Cell Function Markers
Baseline HbA1c showed a significant inverse correlation with PCPR and ΔCPR (r = − 0.25 and − 0.33, respectively; P < 0.01 for both), but not with FCPR (r = 0.02; P = 0.853) (Fig. 2), suggesting the confounding effect of baseline HbA1c on markers of meal-induced insulin secretion.
Relationship between baseline HbA1c and a fasting serum C-peptide (FCPR), b 2-h postprandial serum C-peptide (PCPR), and c serum C-peptide increment (ΔCPR) in 141 patients. ΔCPR is calculated according to the following formula: ΔCPR = PCPR − FCPR. Pearson’s correlation coefficients and P values are presented. HbA1c glycated hemoglobin
HbA1c Change from Baseline to 3 Months (HbA1c Change 0–3 Months) and to 6 Months (HbA1c Change 0–6 Months)
The mean ± standard error change in HbA1c from baseline was − 1.27 ± 0.20% at 3 months and − 1.16 ± 0.17% at 6 months (P < 0.001 for both; Fig. 3). The difference in HbA1c change between 3 and 6 months was not significant (P = 0.314), justifying the LOCF approach. LOCF was applied to eight patients.
Of 59 patients who continued dulaglutide for at least 6 months without any additional glucose-lowering medications, almost half (n = 29) achieved a reduction in HbA1c of at least 1% over 6 months. Baseline HbA1c was positively and significantly associated with the treatment response (r = 0.67; P < 0.001; Supplementary Fig. 1). On the contrary, we did not find an association between HbA1c change 0–6 months and OAD dose change (or discontinuation) or insulin dose change (P = 0.221 and 0.171, respectively). Thus, we did not adjust for OAD or insulin dose change.
Second-Step Analysis: Association Between β-Cell Function Markers and Glycemic Response to Dulaglutide
Generalized Linear Model Analysis
In the generalized linear model analysis with adjustment for baseline HbA1c as a covariate, the β-cell function markers were significantly associated with HbA1c change 0–6 months (regression coefficient for FCPR = − 0.71; P = 0.031; regression coefficient for PCPR = − 0.46; P = 0.015; regression coefficient for ΔCPR = − 0.52; P = 0.043) (Table 3). Other variables (age, sex, BMI, duration of T2D, FPG, PPG, HDL cholesterol, and triglycerides) lacked significant associations with the treatment response. As supplementary subgroup analyses, fasting immunoreactive insulin, HOMA2-%β, and HOMA2-%S were also evaluated in non-insulin-treated patients but were not significantly associated with the treatment response (P > 0.5 for all), possibly as a result of large variances (Supplementary Table 2).
Logistic Regression for Determining a Good Responder
Furthermore, in logistic regression with adjustment for baseline HbA1c as a covariate, FCPR was a significant predictor for achieving a reduction in HbA1c of at least 1% (odds ratio [OR], 2.08; 95% confidence interval [CI], 1.02–4.23; P = 0.044) (Table 4) with an area under the receiver operating characteristic curve (AUC) of 0.83 (95% CI 0.72–0.94) (Fig. 4). For discriminating good or poor responders, the probability (P) of achieving a reduction in HbA1c of at least 1% over 6 months was formulated using predictor variables X1 (baseline HbA1c) and X2 (FCPR) as follows:
where β0 = − 10.42 (intercept), β1 = 1.20 (coefficient for baseline HbA1c), and β2 = 0.73 (coefficient for FCPR) (Table 4). With a cutoff of P = 0.50, a sensitivity of 0.81 and specificity of 0.79 was achieved. Thus, if a patient who initiated dulaglutide treatment had a probability (P) of at least 0.50, which can be calculated with a patient’s baseline HbA1c (X1) and FCPR (X2) with the aforementioned formula, the patient is likely to be a good responder. Although neither PCPR nor ΔCPR was a significant predictor in logistic regression analysis, the results were directionally consistent with that of FCPR (for PCPR, OR 1.69 [95% CI 0.84–3.40]; AUC 0.81 [95% CI 0.70–0.92]; P = 0.143; for ΔCPR, OR 1.27 [95% CI 0.67–2.39]; AUC 0.80 [95% CI 0.69–0.91]; P = 0.467) (Table 4, Supplementary Fig. 2).
Treatment Response Analysis with Adjustment for Baseline DPP4 Inhibitors Use
In the 59 patients, baseline DPP-4 inhibitor use was significantly associated with higher FCPR and PCPR, while other baseline OADs use were not associated with baseline C-peptide (Supplementary Table 3). On the basis of these results, we additionally evaluated the relationship between HbA1c change 0–6 months and each β-cell function marker with baseline HbA1c and DPP-4 inhibitor use as covariates. In the generalized linear model, the β-cell function markers were significantly associated with HbA1c change 0–6 months regardless of the presence or absence of baseline DPP-4 inhibitor use (regression coefficient for FCPR = − 1.25; P = 0.007; regression coefficient for PCPR = − 0.51; P = 0.007; regression coefficient for ΔCPR = − 0.53; P = 0.036) (Supplementary Table 4). Moreover, FCPR was a significant predictor for achieving a reduction in HbA1c of at least 1% regardless of the presence or absence of baseline DPP-4 inhibitor use (OR 2.30 [95% CI 1.09–4.86]; AUC 0.84 [95% CI 0.74–0.94]; P = 0.029) (Supplementary Table 4). Although PCPR nor ΔCPR was a significant predictor, the results were directionally consistent with that of FCPR (for PCPR, OR 1.72 [95% CI 0.85–3.47]; AUC 0.81 [95% CI 0.701–0.919]; P = 0.129; for ΔCPR, OR 1.27 [95% CI 0.67–2.39]; AUC 0.80 [95% CI 0.69–0.91]; P = 0.467). Furthermore, in a subgroup of patients who switched from DPP-4 inhibitors to dulaglutide (n = 49), the β-cell function markers were significantly associated with HbA1c change 0–6 months in the generalized linear model (Supplementary Table 5).
Discussion
In this study, we conducted two-step analyses. The first-step analysis evaluated the confounding of baseline glycemic control on β-cell function markers to determine the least confounded marker; the second-step analysis investigated the association of β-cell function markers and glycemic response to dulaglutide. In the first-step analysis, baseline HbA1c was significantly inversely associated with PCPR and ΔCPR, indicating that chronic hyperglycemia may deteriorate meal-induced endogenous insulin secretion and confound these markers. On the contrary, FCPR was not associated with baseline HbA1c. Thus, we delineated FCPR as the least confounded marker. In the second-step analysis, all the β-cell function markers were significantly inversely associated with HbA1c change 0–6 months in the generalized linear model with adjustment for baseline HbA1c. Furthermore, FCPR was a significant predictor for achieving an HbA1c change 0–6 months of at least 1% (good responders) with the AUC of 0.83. Although neither PCPR nor ΔCPR was a significant predictor of the achievement of HbA1c reduction of at least 1%, the results of the logistic regression analysis were directionally consistent among the β-cell function markers studied.
Regarding the first-step analysis, our findings that PCPR and ΔCPR were confounded by baseline HbA1c were conceivable because meal-induced endogenous insulin secretion can be impaired by chronic hyperglycemia [15]. Furthermore, the study that examined factors influencing PCPR in 273 Japanese patients with T2D suggested that this factor might reflect the state of glucose toxicity-induced impaired insulin secretion [10]. Although some observational studies have shown that the PCPR is a potentially useful β-cell function marker for subsequent insulin treatment or successful switching from complex insulin therapy to GLP-1RA monotherapy [7, 8, 16], we should note that the patients in those previous studies had better baseline glycemic control than patients in the present study. Collectively, the markers of meal-induced insulin secretion might be slightly less valuable in estimating β-cell function in patients exposed to chronic hyperglycemia because baseline glycemic control may confound the association between these markers and glycemic response, distorting the estimation. Although the molecular mechanisms of glucose toxicity remain largely unclear, it may be partly attributable to the deterioration of β-cell responsiveness to glucose and the incretin effect, which can be recovered by improving glycemic control [9, 15, 17].
With regard to the second-step analysis, we indicated that the β-cell function markers assessed in the MTT were significantly associated with glycemic response to dulaglutide using the generalized linear model with adjustment for baseline HbA1c. In addition, FCPR could explain the variance with the AUC of 0.83 (sensitivity = 0.81; specificity = 0.79). Although neither PCPR nor ΔCPR was a significant predictor of the achievement of HbA1c reduction of at least 1%, the results were directionally consistent with that of FCPR. Because potentiation of β-cell insulin secretion is considered a major mechanism of action of GLP-1RAs, including dulaglutide [1, 18, 19], it is conceivable that a higher C-peptide, which reflects higher residual β-cell function, leads to better glycemic response to dulaglutide. A recent study evaluated the association between the β-cell mass and glycemic response to dulaglutide in rodent models, which showed a positive correlation [20]; this was consistent with our findings. Our findings also agree with previous clinical studies using GLP-1RAs other than dulaglutide, which showed that reduced residual β-cell functions were associated with insufficient glycemic response to liraglutide and exenatide [3,4,5,6,7,8, 21, 22]. However, these clinical studies investigated the effects of exenatide or liraglutide, but not dulaglutide.
Regarding the strengths of the present study, we measured β-cell function markers using the standardized MTT in patients hospitalized for nonemergent glycemic control. This ensured proper measurements and compared fasting and postprandial β-cell markers, highlighting confounding effects of baseline HbA1c on PCPR and ΔCPR, as well as the utility of FCPR as a marker of response to dulaglutide. Since there is scarce evidence regarding the association between β-cell function markers and response to dulaglutide, we believe our study provides an important suggestion on the useful clinical markers of response to dulaglutide. This study also has several limitations. First, the limited sample size potentially reduced the statistical power for some analyses, including the subgroup analyses on the associations of fasting immunoreactive insulin and HOMA2-%β with treatment response in non-insulin-treated patients. Second, because of the retrospective nature of the study, we could not completely eliminate the influence of unmeasured confounding factors. We also note that a certain proportion of the patients in the first-step analysis were excluded from the second-step analysis for various reasons (e.g., loss to follow-up); we could not eliminate the possibility that their exclusion affected the second-step analysis results. A prospective study with a large sample size is warranted to confirm our findings. Third, we assessed baseline β-cell function using serum C-peptide as readout, which could be affected by multiple factors, such as concurrent glucose, insulin sensitivity, and C-peptide clearance [23]. Although there are accurate tests for β-cell function, such as a hyperglycemic clamp or intravenous glucose tolerance tests, they are highly invasive and time-consuming, which makes the measurement of C-peptide the most suitable in routine clinical practice. Another potential limitation of C-peptide measurements is the possible modification of endogenous insulin secretion with concurrent use of exogenous insulin and OAD [24]. However, all 141 patients in this study had high fasting and postprandial glucose levels at baseline, and the difference between those treated with and without exogenous insulin was small (mean fasting glucose, 9.26 mmol/L and 9.14 mmol/L; mean postprandial glucose, 15.60 mmol/L and 16.18 mmol/L, respectively). Although baseline DPP-4 inhibitor use was significantly associated with FCPR and PCPR in the second-step analysis, the results with and without adjustment for DPP-4 inhibitors were consistent with each other, both showing significant associations with dulaglutide response for FCPR, PCPR, and ΔCPR in the generalized linear model and for FCPR in the logistic regression model. Fourth, the LOCF approach, in which the last valid observation between 3 and 6 months was carried forward for eight patients (13.6%) missing 6-month measurements, might have influenced the data in this study. However, we evaluated the difference in HbA1c change 0–3 months and HbA1 change 0–6 months, showing that the difference was small and not significant. Thus, our use of the LOCF approach should have had little influence on the results. Lastly, the dose of dulaglutide (0.75 mg), the approved dose in Japan used in the current study, was half of the maximum dose (1.5 mg) approved in many countries. However, the differences between the HbA1c-lowering effects of 0.75 mg and 1.5 mg of dulaglutide were small in multiple large-scale studies [25,26,27,28,29].
Conclusion
The current study suggests that fasting and meal-induced C-peptide are associated with glycemic response to dulaglutide, among which FCPR is least confounded by baseline glycemic control. FCPR can be a useful marker for glycemic response to dulaglutide in clinical settings.
References
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonist and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368(9548):1696–705.
Abd El Aziz MS, Kahle M, Meier JJ, Nauck MA. A meta-analysis comparing short- or long-acting GLP-1 receptor agonists versus insulin treatment form head-to-head studies in type 2 diabetic patients. Diabetes Obes Metab. 2017;19(2):216–27.
Jones AG, McDonald TJ, Shields BM, et al. Markers of β-cell failure predict poor glycemic response to GLP-1 receptor agonist therapy in type 2 diabetes. Diabetes Care. 2016;39(2):250–7.
Usui R, Yabe D, Kuwata H, et al. Retrospective analysis of safety and efficacy of insulin-to-liraglutide switch in Japanese type 2 diabetes: a caution against inappropriate use in patients with reduced β-cell function. J Diabetes Investig. 2013;4(6):585–94.
Usui R, Sakuramachi Y, Seino Y, et al. Retrospective analysis of liraglutide and basal insulin combination therapy in Japanese type 2 diabetes patients: the association between remaining β-cell function and the achievement of the glycated hemoglobin target 1 year after initiation. J Diabetes Investig. 2018;9(4):822–30.
Kozawa J, Inoue K, Iwamoto R, et al. Liraglutide is effective in type 2 diabetic patients with sustained endogenous insulin-secreting capacity. J Diabetes Investig. 2012;3(3):294–7.
Iwao T, Sakai K, Sata M. Postprandial serum C-peptide is a useful parameter in the prediction of successful switching to liraglutide monotherapy from complex insulin therapy in Japanese patients with type 2 diabetes. J Diabetes Complicat. 2013;27(1):87–91.
Thong KY, McDonald TJ, Hattersley AT, et al. The association between postprandial urinary C-peptide creatinine ratio and the treatment response to liraglutide: a multi-centre observational study. Diabet Med. 2014;31(4):403–11.
Rossetti L, Giaccari A, DeFronzo RA. Glucose toxicity. Diabetes Care. 1990;13:610–30.
Funakoshi S, Fujimoto S, Hamasaki A, et al. Analysis of factors influencing postprandial C-peptide levels in Japanese patients with type 2 diabetes: comparison with C-peptide levels after glucagon load. J Diabetes Investig. 2011;2(6):429–34.
Jones AG, Lonergan M, Henley WE, Pearson ER, Hattersley AT, Shields BM. Should studies of diabetes treatment stratification correct for baseline HbA1c? PLoS ONE. 2016;11(4):e0152428.
DeFronzo RA, Stonehouse AH, Han J, Wintle ME. Relationship of baseline HbA1c and efficacy of current glucose-lowering therapies: a meta-analysis of randomized clinical trials. Diabet Med. 2010;27(3):309–17.
Wysham C, Guerci B, D’Alessio D, Jia N, Botros ST. Baseline factors associated with glycaemic response to treatment with once-weekly dulaglutide in patients with type 2 diabetes. Diabetes Obes Metab. 2016;18(11):1138–42.
Hastie T, Tibshirani R, Friedman J. The elements of statistical learning: data mining, inference, and prediction. 2nd ed. New York: Springer; 2009.
Højberg PV, Vilsbøll T, Zander M, et al. Four weeks of near-normalization of blood glucose has no effect on postprandial GLP-1 and GIP secretion, but augments pancreatic B-cell responsiveness to a meal in patients with type 2 diabetes. Diabet Med. 2008;25(11):1268–75.
Saisho Y, Kou K, Tanaka K, et al. Postprandial serum C-peptide to plasma glucose ratio as a predictor of subsequent insulin treatment in patients with type 2 diabetes. Endocr J. 2011;58(4):315–22.
Knop FK, Vilsbøll T, Højberg PV, et al. Reduced incretin effect in type 2 diabetes: cause or consequence of the diabetic state? Diabetes. 2007;56(8):1951–9.
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8(12):728–42.
Mari A, Del Prato S, Ludvik D, et al. Differential effects of once-weekly glucagon-like peptide-1 receptor agonist and metformin on pancreatic β-cell and insulin sensitivity during a standardized test meal in patients with type 2 diabetes. Diabetes Obes Metab. 2016;18(8):834–9.
Murakami T, Fujimoto H, Fujita N, Hamamatsu K, Yabe D, Inagaki N. Association of glucagon-like peptide-1 receptor-targeted imaging probe with in vivo glucagon-like peptide-1 receptor agonist glucose-lowering effects. J Diabetes Investig. 2020;11(6):1448–56.
Kondo Y, Satoh S, Nagakura J, Kimura M, Nezu U, Terauchi Y. Defining criteria for the introduction of liraglutide using the glucagon stimulation test in patients with type 2 diabetes. J Diabetes Investig. 2013;4(6):571–5.
Araki H, Tanaka Y, Yoshida S, et al. Oral glucose-stimulated serum C-peptide predicts successful switching from insulin therapy to liraglutide monotherapy in Japanese patients with type 2 diabetes and renal impairment. J Diabetes Investig. 2014;5(4):435–41.
Jones AG, Hattersley AT. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet Med. 2013;30(7):803–17.
Albareda M, Rigla M, Rodríguez-Espinosa J, et al. Influence of exogenous insulin on C-peptide levels in subjects with type 2 diabetes. Diabetes Res Clin Pract. 2005;68(3):202–6.
Umipierrez G, Tofé Povedano S, Pérez Manghi F, Shurzinske L, Pechtner V. Efficacy and safety of dulaglutide monotherapy versus metformin in patients with type 2 diabetes in a randomized controlled trial (AWARD-3). Diabetes Care. 2014;37(8):2168–76.
Blonde L, Jendle J, Gross J, et al. Once-weekly dulaglutide versus bedtime insulin glargine, both in combination with prandial insulin lispro, in patients with type 2 diabetes (AWARD-4): a randomised, open-label, phase 3, non-inferiority study. Lancet. 2015;385(9982):2057–66.
Weinstock RS, Guerci B, Umipierrez G, Nauck MA, Skrivanek Z, Milicevic Z. Safety and efficacy of once-weekly dulaglutide versus sitagliptin after 2 years in metformin-treated patients with type 2 diabetes (AWARD-5): a randomized, phase III study. Diabetes Obes Metab. 2015;17(9):849–58.
Tuttle KR, Lakshmanan MC, Rayner B, et al. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): a multicentre, open-label, randomised trial. Lancet Diabetes Endocrinol. 2018;6(8):605–17.
Ludvik B, Frías JP, Tinahones FJ, et al. Dulaglutide as add-on therapy to SGLT2 inhibitors in patients with inadequately controlled type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2018;6(5):370–81.
Acknowledgements
Funding
Satoshi Yoshiji is a research fellow of the Japan Society for the Promotion of Science (DC1). This research did not receive any other specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Satoshi Yoshiji contributed to the study design and data analysis. Masashi Hasebe, Satoshi Yoshiji, and Jun Fujikawa contributed to data collection. Satoshi Yoshiji and Masashi Hasebe contributed to data interpretation and drafting and editing of the manuscript. Yorihiro Iwasaki, Kimitaka Shibue, Yamato Keidai, Yohei Seno, Kanako Iwasaski, Sachiko Honjo, and Akihiro Hamasaki contributed to data interpretation and editing of the manuscript. Akihiro Hamasaki supervised the study. All authors read and approved the final manuscript.
Prior Presentation
This study was presented in part at the Virtual 81st Scientific Sessions of the American Diabetes Association (June 25–29, 2021) and the Virtual 57th Annual Meeting of the European Association for the Study of Diabetes (September 28–October 1, 2021).
Disclosures
Satoshi Yoshiji, Masashi Hasebe, Yorihiro Iwasaki, Kimitaka Shibue, Yamato Keidai, Yohei Seno, Kanako Iwasaki, Sachiko Honjo, Jun Fujikawa and Akihiro Hamasaki have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the local ethics committee of Kitano Hospital (No. 1807005, approved on April 8, 2020). All procedures were performed in accordance with the Declaration of Helsinki of 1964, as revised in 2013. Informed consent and registration in a publicly accessible database were waived because of the retrospective nature of this study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yoshiji, S., Hasebe, M., Iwasaki, Y. et al. Exploring a Suitable Marker of Glycemic Response to Dulaglutide in Patients with Type 2 Diabetes: A Retrospective Study. Diabetes Ther 13, 733–746 (2022). https://doi.org/10.1007/s13300-022-01231-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01231-1