Abstract
Introduction
The COVID-19 pandemic led to an international health crisis and restrictions. While the phenotype associated with COVID-19 severity in people with diabetes has rapidly been explored, the impact of restrictive measures, including lockdown, and tertiary care disruption on metabolic control and access to healthcare remained unknown. The aim of our study was to provide a comprehensive assessment on the overall management of diabetes during lockdown, including glucose control, weight changes, health care consumption and use of alternative forms of care such as telemedicine services, in a large sample of patients with type 1 (T1DM) or type 2 diabetes mellitus (T2DM).
Methods
A prioritization of a care self-administered questionnaire was sent at the end of the first COVID-19 lockdown to all patients with diabetes routinely followed by diabetologists from the University Hospital of Nancy (France). This observational cross-sectional single-center study focused on data from patients with diabetes who returned the questionnaire along with medical records. The primary outcome was the change in HbA1c levels between the 6 months preceding and the 6 weeks following the lockdown. Data are expressed as numbers (%) or medians (quartiles). This study is registered with ClinicalTrials.gov (NCT04485351).
Results
We analyzed data from 870 patients with diabetes: 549 T2DM (63.1%), 520 males (59.8%), age 65.0 (57.0, 72.0), body mass index 28.6 (25.1, 32.9) and diabetes duration 20.0 (10.0, 30.0) years. HbA1c levels pre- and post-lockdown were respectively 7.7% (7.1, 8.4) and 7.4% (6.8, 8.2), translating into a significant reduction of − 0.1% (− 0.6, 0.15) (p < 0.0001). Stratified analyses suggested a consistent significant reduction of HbA1c independently of diabetes type. HbA1c reduction was significantly different according to weight changes: − 0.3% (− 0.8, 0.0), − 0.1% (− 0.5, 0.1) and − 0.1% (− 0.5, 0.3) for patients who lost, had stable or gained weight, respectively (p = 0.0029). Respectively, 423 (49.4%) and 790 (92.3%) patients did not consult their general practitioner and diabetologist. Blood tests were undergone by 379 (44.8%) patients, 673 (78.3%) did refill their prescriptions, and 269 (32.1%) used teleconsultation services.
Conclusions
Despite the implementation of a lockdown and disruption in healthcare, no deterioration, rather an improvement, in metabolic control was observed in a large sample of patients with T1DM and T2DM.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Why carry out this study? |
COVID-19 pandemic has enforced restrictions, including lockdown and stay-at-home orders. |
The impact of the lockdown itself and tertiary care disruption on metabolic control and access to healthcare in patients with diabetes are discussed. |
No comprehensive assessment of the overall management of diabetes during lockdown, including glucose control, weight changes, health care consumption and use of alternative forms of care such as telemedicine services, was performed in a large sample of patients with both T1DM and T2DM. |
What was learned from the study? |
Metabolic control of patients with type 1 and type 2 diabetes improved during lockdown. |
Weight changes during lockdown were associated with different metabolic outcomes. |
Drastic reductions in routine healthcare consumption were observed during lockdown, but continuity of care was ensured through strong mobilization of primary care lines. |
Introduction
In late 2019, the emergence of a new coronavirus in Wuhan (China) that causes severe acute respiratory syndrome (SARS-CoV-2) led to a global pandemic and an unprecedented international health crisis [1, 2]. Since then, exceptional measures have been taken by governments worldwide, guided by public health authorities, to slow the virus’ spread and prevent healthcare systems from becoming overloaded. In France, a national lockdown was established with stay-at-home orders for approximately 2 months (from 16 March to 13 May 2020) to increase social distancing and restrict population movements. In addition, hospital routine care appointments were cancelled to reallocate medical resources toward coronavirus disease-2019 (COVID-19) units and to limit contacts between patients in hospitals or waiting rooms. Based on several epidemiological studies [3,4,5], the French High Council for Public Health considered some patients with underlying medical conditions as being at higher risk from SARS-CoV-2, including patients with diabetes, who were either uncontrolled or presenting with secondary complications, and advised extreme caution [6]. While these measures certainly helped to contain the pandemic and keep vulnerable patients safe, they also generated a drastic decrease in the use of non-COVID-19 medical care [7]. A popular French medical appointment scheduling platform notably recorded a 44% drop in the activity of general practitioners (GP) and 71% of specialist physicians between January and April 2020 [8]. Reasons for renouncement to healthcare included fear of being infected (38%), fear of disturbing the physician (28%) and medical office closure (17%). Additionally, stay-at-home orders have enforced changes in daily habits, including limitation of physical activity, changes in diet or even in stress and anxiety levels, which may have affected glycemic control or treatment adherence in patients with diabetes [9]. Indeed, two studies conducted among patients with type 2 diabetes (T2DM) reported adverse changes in dietary patterns and food cravings following COVID-19 confinement, specifically an increase in carbohydrate, sugary food and snacks intake while physical activity decreased, though glycated hemoglobin (HbA1c) was not assessed [10, 11]. A third study reported a non-significant increase in weight, HbA1c and fasting glucose [12]. Conversely, several studies have showed either neutral or beneficial effects of lockdown, specifically in type 1 diabetes (T1DM) using continuous or flash glucose monitoring (CGM/FGM), suggesting that having a more regular lifestyle and more time for self-management may help improve glucose control, at least in the short term [13,14,15,16,17,18].
As no comprehensive assessment of diabetes management was performed, we hypothesized that the “lockdown effect” could have affected patients with diabetes beyond glucose metrics. Hence, we conducted a cross-sectional study in a large population sample of patients with T1DM and T2DM aiming at assessing the global impact of the lockdown and stay-at-home orders due to COVID-19 on metabolic control and healthcare consumption.
Methods
Study Design and Participants
The CONFI-DIAB study was an observational cross-sectional single-center study in a tertiary care center (University Hospital of Nancy, France) aiming at describing the impact of the COVID-19 lockdown on metabolic control and access to healthcare in a population sample of patients with diabetes.
The study was sponsored by the Regional University Hospital of Nancy. The protocol was declared and approved by the local Institutional Ethics Committee ([Comité d’Ethique du CHRU de Nancy], Ref. saisine n°CO-21). This study is registered with ClinicalTrials.gov, number NCT04485351. The study was conducted in accordance with the Declaration of Helsinki 1964 and its later amendments. According to the European General Data Protection Regulation, all subjects were informed that their data might be used for research purposes and of their right to prevent their data from being processed. Patients who objected to the reuse of their data were not included in this study, in accordance with French legislation. Results are reported in accordance with the STROBE statement.
Procedures
To identify patients who urgently needed medical care at the end of the first COVID-19 lockdown in France, a self-administered questionnaire was sent the week before the end of the lockdown by postal mail to all people with diabetes who were being followed for routine care within the 6 months prior to the lockdown by a diabetologist from the Regional University Hospital of Nancy, France (N = 2076). We analyzed data from all adult patients with diabetes known for at least 6 months who returned the fulfilled prioritization of care questionnaire along with data from existing medical records for the purpose of our study.
Outcomes
The primary outcome was the change in HbA1c levels between the period preceding and following the COVID-19 lockdown implemented from 17 March 2020 to 11 May 2020 (55 consecutive days). Data from the 6 months preceding the start of the lockdown (± 1 week), between 18 September 2019 and 24 March 2020, were compared with data from the 6 weeks following the end of the lockdown, between 11 May 2020 and 20 June 2020. Primary endpoint analysis was based on patients with self-reported and/or laboratory confirmed HbA1c levels available pre- and post-lockdown. A sensitivity analysis based on the type of collected HbA1c levels (laboratory confirmed or self-reported) was performed to assess for robustness.
Secondary outcomes were: (1) pre- and post-lockdown biological characteristics, (2) proportion of patients reporting changes in weight, physical activity or alcohol/tobacco consumption, (3) incidence of clinically significant events including ketosis, ketoacidosis, severe hypoglycemia and hospitalization, (4) proportion of people who forgot and/or discontinued one or several medication(s), (5) consumption of care and medical goods and (6) COVID-19 infection rate.
Stratified analyses for the primary outcome were conducted according to diabetes type (T1DM versus T2DM versus other), baseline age (≤ 65 versus > 65), self-reported weight change between pre- and post-lockdown periods (loss versus stable versus gain), self-reported treatment compliance (patients who reported having forgotten or interrupted any of their medication during lockdown versus those who did not) and healthcare consumption (people who benefited from a face-to-face or remote consultation with their GP and/or diabetologist during lockdown versus those who did not).
Measures
Data collection was performed by a physician and double-checked by a pharmacist. Data collected from medical records included: baseline age, gender, type of diabetes, weight, height, type of urban area and diabetes duration; laboratory-confirmed HbA1c levels (pre- and post-lockdown); biological parameters including hemoglobin, thyroid stimulating hormone (TSH), fasting blood glucose, hepatic profile, lipid profile, serum creatinine and estimated glomerular filtration rate (eGFR) using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula, microalbuminuria and urine albumin-to-creatinine ratio (UACR); comorbidities including cardiovascular disease (myocardial infarction, stroke or transient cerebrovascular attack, coronaropathy, cardiovascular surgery, chronic heart failure NYHA class III or IV, peripheral artery disease), hypertension, nephropathy (microproteinuria and/or macroproteinuria and/or eGFR ≤ 60 ml min–1 [1.73 m] –2 [CKD-EPI]), neuropathy (sensory or motor peripheral neuropathy, neuropathic pain) and diabetic retinopathy (mild, moderate and severe non-proliferative and proliferative). Self-reported data included: self-reported HbA1c (pre- and post-lockdown); changes in weight (loss, stable or gain; absolute value), physical activity (intensity and frequency), alcohol consumption (absolute and relative) and tobacco consumption (smokers proportion, smoking relapse) between pre- and post-lockdown periods; self-reported occurrence of severe hypoglycemia, ketosis and ketoacidosis; treatments including doses and compliance estimates; COVID-19 infection status and clinical evolution; self-reported healthcare consumption during lockdown (face-to-face or remote visit with a GP, diabetologist, nurse, pharmacist and/or bio-medical laboratory) and related reasons.
Statistical Analysis
Data were analyzed using SAS v9.4. Categorical data are expressed as numbers and percentages; continuous data are expressed as median associated with quartile values. Differences between pre- and post-lockdown were assessed using the Wilcoxon signed rank test when both measures were available. Sensitivity analyses based on subgroups were performed using Wilcoxon test or Kruskal-Wallis test. A p-value < 0.05 was considered statistically significant.
Results
Demographic and Clinical Characteristics
This analysis focused on 870 patients with diabetes: 520 (59.8%) were male, age was 65.0 (57.0, 72.0) years, BMI was 28.6 (25.1, 32.9), 549 (63.1%) had T2DM (T1DM, 30.7%), and diabetes duration was 20.0 (10.0, 30.0) years. Main clinical and biological characteristics of study participants are shown in Tables 1 and 2.
Changes in HbA1c
HbA1c levels pre- and post-lockdown were respectively of 7.7% (7.1, 8.4) and 7.4% (6.8, 8.2), which translated into a significant reduction between the two periods of − 0.1% (− 0.6, 0.15) (p < 0.0001) (Table 3). Sensitivity analyses conducted in patients with either biologically confirmed only or self-reported only HbA1c found similar significant reductions in the primary outcome.
Clinical Self-Assessment
From pre- to post-lockdown periods, 32.1% and 15.9% of patients reported respectively weight gain (+ 2.0 kg [2.0, 4.0]) and weight loss (− 2.5 kg [− 4.0, − 2.0]). Respectively, 9.2%, 45.8% and 45.0% of patients reported higher, similar and lower levels of physical activity than usual. In addition, duration and frequency of physical activity were assessed as being of 30 min once or twice per week in 48.1%, three or four times per week in 24.1% and five times or more per week in 27.8% of patients. Eighty-five (10.0%) patients were smokers and 21 (2.6%) resumed smoking during lockdown. Regarding alcohol, 656 (90.9%) people reported consuming fewer than two drinks per day for women or three for men during lockdown. This consumption was estimated to be higher, usual and lower than usual in respectively 41 (5.9%), 577 (83.1%) and 76 (11.0%) people.
Severe hypoglycemia episodes have been reported by 36 (4.3%) of 840 patients, while 21 (2.8%) of 756 reported an episode of ketosis/ketoacidosis. Twelve patients reported RT-PCR confirmed COVID-19, including four COVID-19-related hospitalization (three within an intensive care unit).
Changes in Biological Parameters
No significant change in biological parameters between pre- and post-lockdown period was observed, with the exception of minor but significant changes in hepatic aspartate-aminotransferase AST (+ 2.0 IU/l (− 1.0, 6.0); p < 0.0001), creatinine (0.1 mg/l; (− 0.5, 0.8); p < 0.0001) and eGFR (− 0.8 ml/min/1.73 m2 (− 5.0, 3.6); p < 0.02).
Healthcare Consumption During Lockdown and Discontinuation Reasons
Respectively, 423 (49.4%) and 790 (92.3%) patients did not consult their GP and diabetologist (Table 4). One hundred ninety-five (23.0%) patients were supported with home nursing care. Blood tests were done by 379 (44.8%) patients, while 673 (78.3%) did refill their prescriptions. Two hundred sixty-nine (32.1%) patients used teleconsultation services at least once. Among them, 43.4% reported an online visit with their GP, 47.9% with their diabetologist and 30.5% with their diabetes specialist nurse. Among the 569 patients who did not use teleconsultation services, 87.6% reported absence of need and 10.0% did not have internet access. Finally, 716 (86.4%) patients reported being well informed about teleconsultation services (access to remote medical services and medical prescription, health insurance cover) and 588 (71.5%) would not be willing to use remote medical services for future routine clinical practice.
Treatment Compliance
During the lockdown, 83 patients (9.7%) reported forgetting to take their medication, mostly with a frequency of once per month (40.0%) or once per week (25.0%). Medications involved were mainly antidiabetics, cardiovascular and to a lesser extent lipid-lowering agent. Twenty patients (2.4%) discontinued their medication, including six discontinuations for medical reasons, five for unavailable prescription and nine for various personal reasons.
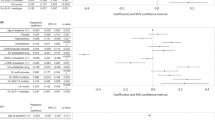
Stratified Analyses
Even though pre- and post-lockdown HbA1c levels were significantly different across diabetes types, stratified analyses of the primary outcome suggested a consistent significant reduction of HbA1c during lockdown independently of diabetes type (Table 5). Furthermore, a significantly different reduction in HbA1c was found in participants who lost weight, had stable weight or weight gain during lockdown, respectively, − 0.3% (− 0.8, 0.0), − 0.1% (− 0.5, 0.1) and − 0.1% (− 0.5, 0.3) (p = 0.0029) (Table 6). Detailed weight changes according to T1DM and T2DM subgroups were respectively as follows: baseline weight of 74.0 kg (64.0, 83.5) and 87.5 kg (78.0, 100.0); weight gain in 30.2% (+ 2.0 kg [1.5, 3.0]) and 34.0% (+ 3.0 kg [2.0, 4.0]) of patients; weight loss in 18.1% (− 2.0 kg [− 1.5, − 3.0]) and 15.0% (− 3.0 kg [− 2.0, − 4.0]) of patients. Finally, no heterogeneity on HbA1c change was found across subgroups based on age, self-reported treatment compliance or healthcare consumption.
Discussion
CONFI-DIAB is the largest study conducted to assess the impact of the COVID-19 lockdown on metabolic control and healthcare consumption, through a comprehensive approach going beyond glucose metrics, in our population sample of patients with T1DM and T2DM from tertiary care. Unexpectedly, our study including 870 patients with diabetes demonstrated no deleterious effect of COVID-19 lockdown and stay-at-home orders on glycemic control. Indeed, a statistically significant reduction in HbA1c between pre- and post-lockdown periods was observed in our population sample, independently of diabetes type, patient’s age, treatment compliance and healthcare consumption. Only subgroups based on weight change during lockdown were associated with significantly different HbA1c outcomes, i.e., a slight HbA1c decrease (− 0.1%) observed in patients who gained weight or had stable weight, and a greater HbA1c decrease (− 0.3%) in people who lost weight. Also, patients with the highest weight at baseline were more prone to have gained weight after the lockdown period. No clinically significant changes in the biologic parameters of interest were observed, despite minor changes in AST, creatinine and eGFR.
More specifically, we included 267 patients with T1DM in our analysis, monitored by glucose meters or FGM, whose median baseline HbA1c, which was similar to HbA1c reported previously for a representative sample of French patients with T1DM [19], decreased from 7.8% pre-lockdown to 7.6% post-lockdown. Maddaloni et al. reported no significant deterioration in the ambulatory glucose profile of 55 Italian patients, mainly with T1DM, on intensive insulin therapy during the first 14 days of lockdown [16]. Another study on 307 patients with T1DM using FGM compared data from the 14 days prior to and after lockdown and demonstrated significant improvements in mean glucose level, estimated HbA1c (from 7.4 to 7.1%) and time in range (from 57.8 to 62.5%) after 8 weeks of lockdown [20]. Notably, a recent observational study conducted in 1378 T1DM using data from self-reported only glycemic information from FGM and a questionnaire on behavioral changes during lockdown also reported a significant improvement in mean glucose level, which was, however, associated with an increased frequency of hypoglycemia events (OR 1.67 (1.13–2.46)) [18]. Other studies demonstrated similar results suggesting that a more regular lifestyle and less stress might help achieving better glucose control in T1DM [13,14,15, 17]. Nevertheless, these studies were mostly conducted on small series of T1DM only, even though patients with T2DM remain the majority population in France and were advised strict self-quarantine as well [21, 22]. Our study included 63.1% patients with T2DM, whose HbA1c levels decreased from a median of 7.6 to 7.3%, suggesting effective patient education for diabetes self-management even in people with long diabetes duration, several comorbidities and/or intensive insulin therapy. In contrast, in a Turkish study on 101 patients with T2DM, mean HbA1c rose from 7.7 to 8.1%, although not significantly [12]. Hence, lockdown had no deleterious effect on metabolic control in our study, regardless of diabetes type, did not result in a high incidence of acute metabolic complications (severe hypoglycemia, 4.3%; ketosis and/or ketoacidosis, 2.8%) and seemed effective in preventing the spread of SARS-CoV-2 considering the prevalence of diabetes in patients with COVID-19, with only 12 confirmed infection cases [23, 24].
Besides, 32.1% and 15.9% of patients reported having respectively gained and lost weight during lockdown. More specifically, proportions of patients who respectively gained or lost weight were similar across T1DM and T2DM subgroups with a median change of about 2–3 kg. Other studies conducted in either obese or T2DM have previously reported similar results, with proportions of patients respectively gaining and losing weight ranging from 19.0 to 39.6% and 33.0 to 38.6% and absolute mean changes of 0.8–1.5 kg [11, 12, 25]. Furthermore, self-reported weight changes were observed elsewhere in patients with T1DM, with 30.4% reporting weight gain and 13.5% weight loss, which matched our results [18]. The lockdown effect on weight was thus heterogeneous. Possible reasons included changes in daily habits, particularly in more obese patients with T2DM, who increased their sugary food and snack intakes along with more frequent cravings and decreased physical activity as represented by the time spent seated [10]. Despite the implementation of guidance by the World Health Organization to stay physically active during self-quarantine [26], decreased physical activity levels were also reported in both T2DM and T1DM (respectively 42% and 70%), which was not surprising given the stay-at-home orders [11, 13]. In our study, respectively, 45.8% and 45.0% of patients declared similar or lower levels of physical activity during lockdown compared to pre-lockdown, which was consistent with the results of a study conducted by the French High Council for Public Health on a representative sample of the French population [27]. Additionally, the French Society of Diabetes recommends 150–300 min of moderate-intensity or 75–150 min of vigorous-intensity physical activity per week, or a combination of both; about half of the patients reported achieving the recommended minimum levels (≥ three times 30 min per week) [28]. Alcohol consumption was estimated as being reasonable (fewer than two or three drinks per day for women or men, respectively) in 90.9% of patients.
The unique specificity of the CONFI-DIAB study was to put metabolic control into perspective in light of the integrated care pathway. First, a drastic reduction in health care consumption was observed because of postponed or cancelled appointments enabling the reallocation of resources to COVID-19 units as described in other countries [29]. Respectively, 49.4% and 92.3% of patients did not consult their GP and diabetologist during the lockdown and 32.1% used teleconsultation services as an alternative. Indeed, telemedicine services rapidly expanded [30] and were useful tools to avoid disrupting care. However, 10.0% of patients within our study reported no internet access, which questions the generalizability of remote medical services. Additionally, 71.5% declared not be willing to use those remote services for routine clinical practice even though discordant results have been previously reported showing higher satisfaction rates [31, 32]. Second, medication noncompliance was infrequent with monthly or weekly treatment compliance gaps reported in 9.7% of patients, primarily regarding antidiabetic and cardiovascular medications, and treatment interruption in 2.4% only. These results were confirmed in a large national study conducted by the French National Agency for the Safety of Medicines and Health Products and the National Health Insurance Fund, which found a maintained or even increased consumption of medicines in patients with diabetes (non-insulin antidiabetics, insulin and cardiovascular treatments) [33]. In contrast, a cross-sectional study performed in Indian patients with T1DM demonstrated that the observed glycemic worsening was mainly due to a lack of insulin and/or glucose strip availability during lockdown [34], which emphasizes the need of a fair distribution of community pharmacies across a territory. Hence, the key role of pharmacists in primary care was underlined in a recent cross-sectional study gathering data from > 10 million patients in the IMS longitudinal prescription database, which showed sustained dispensing activities during the pandemic [35]. Of note, no patient in our population sample indicated difficulty accessing a community pharmacy or refilling their prescriptions, in particular through an exceptional measure decided by the Ministry of Health to enable dispensing chronic medications even if the prescription expired. Moreover, only 1.3% and 3.5% of diabetes specialist nurses and biomedical laboratories, respectively, were unavailable during the lockdown. Even though the eastern region of France, where the study was conducted, was the most affected by the pandemic, national public health measures have been implemented, regardless of the regions, hence suggesting that our results might be generalizable to France. Similarly, a study on patients with T1DM from another French region reported an improvement in glycemic control partly explained by an easier diabetes control perception [18]. However, implementation of public health advices during lockdown might have been different between countries, with the example of the implementation of protective measures, which were highest among participants from Italy, who suffered the most from the COVID-19 epidemic and associated restrictive measures, compared to other European countries [36].
Our study had some limitations. First, a definite causal relationship between lockdown and metabolic control could not be established given the observational cross-sectional nature of the study and the large time frames defining pre- and post-lockdown study periods. Moreover, some data were extracted from a self-administered questionnaire, which might lead to clear biases. Third, a detailed assessment of other relevant factors that might have influenced glycemic measures, such as lifestyle changes, adherence to dietary guidelines, diabetogenic factors, stress levels and/or mental health during lockdown, was not performed. Finally, our single-center population sample might not be representative of the global French population of patients with diabetes since (1) the ratio of patients with T1DM/T2DM and patients' insulin status did not match previously published prevalence data by the French High Council for Public Health [37], and (2) our analysis was performed on patients actively engaged in managing their disease and likely to return the questionnaire.
Conclusion
Despite major changes within the health care system enforced by the local government, metabolic control was maintained or even improved in patients with T1DM and T2DM during the COVID-19 lockdown, particularly in patients who did manage to lose weight. Continuity of care during lockdown was, however, ensured through mobilization of primary care lines, implementation of remote healthcare solutions and probably patients' high level of education in diabetes self-management. Indeed, teleconsultation services have been shown to be effective channels to help patients in need and make sure no one is left behind. It would be interesting to assess whether patients who benefited from remote consultations presented better outcomes than those who did not. Advanced continuous educational programs for self-management and adherence, which are well integrated in the care pathway of patients with diabetes, could also serve as a model for the support of patients with other chronic diseases to convey solutions to everyday practical challenges. Insights from our study might help health authorities and government decision-making processes to deal with future public health outbreaks or epidemics.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio-Medica Atenei Parm. 2020;91(1):157–60.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2020;94:91–5.
Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–64.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–81.
Prise en charge ambulatoire des patients atteints de diabète de type 1 et 2 [Internet]. Haute Autorité de Santé. Disponible sur: https://www.has-sante.fr/jcms/p_3179836/fr/prise-en-charge-ambulatoire-des-patients-atteints-de-diabete-de-type-1-et-2
Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–43.
Coronavirus: un tiers des patients aurait renoncé à des soins pendant l’épidémie selon Doctolib | Le Généraliste [Internet]. LeGénéraliste.fr. 2020. Disponible sur: https://www.legeneraliste.fr/actu-pro/coronavirus-un-tiers-des-patients-aurait-renonce-des-soins-pendant-lepidemie-selon-doctolib
Alshareef R, Al Zahrani A, Alzahrani A, Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab Syndr. 2020;14(5):1583–7.
Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, et al. COVID-19 Lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020;12(8):2327.
Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020;14(5):917–20.
Önmez A, Gamsızkan Z, Özdemir Ş, Kesikbaş E, Gökosmanoğlu F, Torun S, et al. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab Syndr déc. 2020;14(6):1963–6.
Capaldo B, Annuzzi G, Creanza A, Giglio C, De Angelis R, Lupoli R, et al. Blood glucose control during Lockdown for COVID-19: CGM metrics in Italian adults with type 1 diabetes. Diabetes Care. 2020;43(8):e88–9.
Bonora BM, Boscari F, Avogaro A, Bruttomesso D, Fadini GP. Glycaemic control among people with type 1 diabetes during Lockdown for the SARS-CoV-2 outbreak in Italy. Diabetes Ther. 2020;11(6):1369–79.
Aragona M, Rodia C, Bertolotto A, Campi F, Coppelli A, Giannarelli R, et al. Type 1 diabetes and COVID-19: the «lockdown effect». Diabetes Res Clin Pract. 2020;170: 108468.
Maddaloni E, Coraggio L, Pieralice S, Carlone A, Pozzilli P, Buzzetti R. Effects of COVID-19 Lockdown on Glucose Control: continuous glucose monitoring data from people with diabetes on intensive insulin therapy. Diabetes Care. 2020;43(8):e86–7.
Tornese G, Ceconi V, Monasta L, Carletti C, Faleschini E, Barbi E. Glycemic control in type 1 diabetes mellitus during COVID-19 quarantine and the role of in-home physical activity. Diabetes Technol Ther. 2020;22(6):462–7.
Potier L, Hansel B, Larger E, Gautier J-F, Carreira D, Assemien R, et al. Stay-at-home orders during the COVID-19 pandemic, an opportunity to improve glucose control through behavioral changes in type 1 diabetes. Diabetes Care. 2020;44(3):839–43.
SPF. Bulletin Epidémiologique Hebdomadaire, 12 novembre 2013, n°37–38Journée mondiale du diabète, 14 novembre 2013. Disponible sur: /maladies-et-traumatismes/diabete/bulletin-epidemiologique-hebdomadaire-12-novembre-2013-n-37-38journee-mondiale-du-diabete-14-novembre-2013
Fernández E, Cortazar A, Bellido V. Impact of COVID-19 lockdown on glycemic control in patients with type 1 diabetes. Diabetes Res Clin Pract. 2020;166: 108348.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157: 107843.
Fagot-Campagna A, Weill A, Paumier A, Poutignat N, Fournier C, Fosse S, et al. Que retenir du bilan d’ENTRED 2007–2010?: ENTRED 2007–2010: Which key-points? Médecine Mal Métaboliques. 2010;4(2):212–8.
Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020;63(8):1500–15.
Wargny M, Gourdy P, Ludwig L, Seret-Bégué D, Bourron O, Darmon P, et al. Type 1 diabetes in people hospitalized for COVID-19: new insights from the CORONADO study. Diabetes Care. 2020;43(11):e174–7.
Pellegrini M, Ponzo V, Rosato R, Scumaci E, Goitre I, Benso A, et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients. 2020;12(7). Disponible sur: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400808/.
Stay physically active during self-quarantine. Disponible sur: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/stay-physically-active-during-self-quarantine.
Santé Publique France. Physical activity and sedentary behaviour of french adults during the covid-19 lockdown: an overview of prevalence and perceived evolutions (COVIPREV, 2020).—Bulletin épidémiologique hebdomadaire. 2020. Disponible sur: http://beh.santepubliquefrance.fr/beh/2021/Cov_3/2021_Cov_3_1.html.
Duclos M, Oppert J-M, Verges B, Coliche V, Gautier J-F, Guezennec Y, et al. Physical activity and type 2 diabetes. Recommandations of the SFD (Francophone Diabetes Society) diabetes and physical activity working group. Diabetes Metab. 2013;39(3):205–16.
Cuschieri S. COVID-19 panic, solidarity and equity—the Malta exemplary experience. Z Gesundheitswissenschaften. 2020. https://doi.org/10.1007/s10389-020-01308-w.
Jones MS, Goley AL, Alexander BE, Keller SB, Caldwell MM, Buse JB. Inpatient transition to virtual care during COVID-19 Pandemic. Diabetes Technol Ther. 2020;22(6):444–8.
Kanc K, Komel J, Kos M, Wagner J. H(ome)bA1c testing and telemedicine: high satisfaction of people with diabetes for diabetes management during COVID-19 lockdown. Diabetes Res Clin Pract. 2020;166: 108285.
Anjana RM, Pradeepa R, Deepa M, Jebarani S, Venkatesan U, Parvathi SJ, et al. Acceptability and utilization of newer technologies and effects on glycemic control in type 2 diabetes: lessons learned from lockdown. Diabetes Technol Ther. 2020;22(7):527–34.
French National Agency for the Safety of Medicines and Health Products. Use of prescription medicines in France during the Covid-19 epidemic: a national review until 25th April 2021. Disponible sur: https://ansm.sante.fr/actualites/usage-des-medicaments-de-ville-en-france-durant-lepidemie-de-covid-19-point-de-situation-jusquau-25-avril-2021
Verma A, Rajput R, Verma S, Balania VKB, Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metab Syndr. 2020;14(5):1213–6.
Kostev K, Kumar S, Konrad M, Bohlken J. Prescription rates of cardiovascular and diabetes therapies prior to and during the COVID-19 lockdown in Germany. Int J Clin Pharmacol Ther. 2020;58(9):475–81.
Meier K, Glatz T, Guijt MC, Piccininni M, van der Meulen M, Atmar K, et al. Public perspectives on protective measures during the COVID-19 pandemic in the Netherlands, Germany and Italy: a survey study. PLoS ONE. 2020;15(8): e0236917.
SPF. Le poids du diabète en France en 2016. Synthèse épidémiologique. Disponible sur: maladies-et-traumatismes/diabete/le-poids-du-diabete-en-france-en-2016.-synthese-epidemiologique
Acknowledgements
The authors thank Marine Veston for her technical support with the zoning of urban areas across the European territory.
Funding
This work, including the Journal’s Rapid Service Fee, was supported by funds from Asten Santé SA, Dinno Santé, Elivie, Homeperf, ISIS Diabète, Linde Homecare France, Nestlé Home Care, ORKYN’ and Vitalaire Groupe Air Liquide. The corresponding author (Lisa Ludwig), Nicolas Scheyer, Thomas Remen and Bruno Guerci had full access to the data, and the corresponding author had the final decision to submit for publication.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Lisa Ludwig and Bruno Guerci created the concept and design of the study and manuscript. Bruno Guerci did the fund acquisition. Lisa Ludwig developed the first draft of the paper. Lisa Ludwig and Bruno Guerci did the literature review. Nicolas Scheyer and Lisa Ludwig contributed to the data acquisition. Thomas Remen performed the statistical analysis. Lisa Ludwig, Bruno Guerci, Nicolas Scheyer and Thomas Remen did the data analysis. All co-authors contributed to critically revising the manuscript for important intellectual content and all co-authors approved the final manuscript.
Disclosures
Dr. LUDWIG reports grants from Asten Santé SA, grants from Dinno Santé, grants from Elivie, grants from Homeperf, grants from ISIS Diabète, grants from Linde Homecare France, grants from Nestlé HomeCare, grants from ORKYN' and grants from Vitalaire Groupe Air Liquide during the conduct of the study; personal fees from ELI LILLY and Company, outside the submitted work; Dr. Scheyer has nothing to disclose; Dr. REMEN has nothing to disclose, and Prof. GUERCI reports grants, personal fees and non-financial support from Sanofi, personal fees from Orkyn (provider), grants, personal fees and non-financial support from Vitalaire/Air Liquide (provider), personal fees and non-financial support from Abbott, personal fees and non-financial support from Novo Nordisk, grants, personal fees and non-financial support from Eli Lilly, personal fees and non-financial support from Boehringer Ingelheim, personal fees and non-financial support from Roche Diagnostic, personal fees and non-financial support from Astra Zeneca, personal fees and non-financial support from MSD, grants and personal fees from Medtronic, personal fees and non-financial support from Dinno Santé (provider), grants from Asten Santé, grants from Elivie, grants from Homeperf, grants from ISIS Diabète, grants from Linde Homecare France, grants from Nestlé HomeCare, from null, outside the submitted work.
Compliance with Ethics Guidelines
The study was sponsored by the Regional University Hospital of Nancy. The protocol was declared and approved by the local Institutional Ethics Committee ([Comité d’Ethique du CHRU de Nancy], Ref. saisine n°CO-21). This study is registered with ClinicalTrials.gov, number NCT04485351. The study was performed in accordance with the Declaration of Helsinki 1964 and its later amendments. According to the European General Data Protection Regulation, all subjects were informed that their data might be used for research purposes and of their right to prevent their data from being processed. Patients who objected to the reuse of their data were not included in this study, in accordance with French legislation. Results are reported in accordance with the STROBE statement.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ludwig, L., Scheyer, N., Remen, T. et al. The Impact of COVID-19 Lockdown on Metabolic Control and Access to Healthcare in People with Diabetes: the CONFI-DIAB Cross-Sectional Study. Diabetes Ther 12, 2207–2221 (2021). https://doi.org/10.1007/s13300-021-01105-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01105-y