Abstract
Introduction
This study aimed to investigate the relationships between timing of the first physician visit after detection of an abnormal glycated hemoglobin (HbA1c) value at routine annual check and the time to antidiabetic treatment prescription; and understand treatment patterns in patients newly diagnosed with type 2 diabetes mellitus (T2DM).
Methods
This retrospective, longitudinal, observational cohort study examined data from JMDC Inc., an administrative claims database. Patients with HbA1c value of at least 6.5% at routine annual check, aged 20 years or older, and prescribed at least one antidiabetic drug were included. This cohort was classified into early physician visit and delayed physician visit groups based on the timing of the first physician visit relative to the median. Patients were monitored from the date of first HbA1c checkup of at least 6.5% to the date of first physician visit with an HbA1c test, and from the date of the first physician visit to the date of prescription of first-line and second-line T2DM treatments. The time to first prescription of antidiabetic treatment for the two groups was then compared.
Results
Of 4798 eligible patients, 54.8% were prescribed first-line T2DM therapy less than 2 months from the first physician visit for T2DM diagnosis. A lower percentage of the early group compared with the delayed group required T2DM pharmacological therapy in less than 2 months (46.1% vs. 63.4%). The early group had a longer median time to prescription of first-line therapy [92 days vs. 15 days, p < 0.0001; hazard ratio (HR) 1.31, 95% confidence interval (CI) 1.24, 1.39] and second-line therapy (1599 days vs. 1315 days, p < 0.0001; HR 1.22, 95% CI 1.11, 1.34) compared with the delayed group.
Conclusion
In Japanese patients with T2DM, early physician visit after abnormal HbA1c detection at routine annual check is associated with a longer period before T2DM medication requirement, and may improve disease course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The number of patients suspected of having diabetes in Japan continues to increase, which poses significant morbidity, mortality, and healthcare costs. Delayed detection and commencement of treatment is associated with negative outcomes. |
It is expected that early visits after detection of abnormalities in clinical test values will help prevent the worsening of lifestyle-related diseases. This study was conducted to investigate the relationships between the timing of physician visit after a diagnostic HbA1c test for type 2 diabetes mellitus (T2DM) and the time to prescription of the first antidiabetic treatment in the real-world setting. |
Our study showed that a lower percentage of the early group compared with the delayed group required T2DM drug treatment in less than 2 months from diagnosis. |
Compared to the delayed group, they also had a 77-day longer median time to being prescribed first-line therapy, and 284-day longer median time for the second-line therapy. |
Our study suggests that early physician visits after the diagnosis of T2DM may help improve the disease course and delay disease progression. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14681097.
Introduction
Type 2 diabetes mellitus (T2DM) is one of the major causes of morbidity and mortality worldwide. Globally, the number of people with diabetes mellitus (DM) has quadrupled in the last 30 years [1]. About 1 in 11 adults have DM, 90% of whom have T2DM. In Asia, T2DM is a rapidly emerging major public health issue [2]. In the USA, the total estimated cost of diagnosed DM is $245 billion, with the largest components of medical expenditures being hospital inpatient care (43% of the total medical cost), prescription medications to treat the complications of diabetes (18%), antidiabetic agents and DM supplies (12%), physician office visits (9%), and nursing/residential facility stays (8%) [3].
The number of people suspected of having diabetes in Japan continues to increase, rising from an estimated 8.9 million in 2007 to an estimate of over 10 million in 2016, according to the National Health and Nutrition Survey of the Ministry of Health, Labor and Welfare [4]. The increasing prevalence of diabetes and the growing number of patients receiving treatment pose a significant economic burden, with an increase in total healthcare cost in Japan for diabetes from JPY 1.117 trillion in 2005 to JPY 1.224 trillion in 2017—an increase of around 10% [5, 6].
Delayed detection and commencement of treatment is associated with negative outcomes. Improved glycemic control lowers the risk of microvascular complications in patients with T2DM [7]. Every one percent drop in glycated hemoglobin (HbA1c) is associated with improved outcomes over the long term with no threshold effect [8]. Initial intervention should include adequate lifestyle modification, such as diet and exercise therapy, as recommended by the Japanese Clinical Practice Guideline for Diabetes 2016 [9]. In the guidelines, glucose-lowering agents are indicated for patients who fail to achieve favorable glycemic control with adequate trial of lifestyle modification of 2–3 months’ duration. The choice of glucose-lowering agents should be individualized according to patient’s age, level of obesity, disease conditions, liver and kidney functions, and patient’s preference. If a patient fails on monotherapy, increasing the dosage, switching, or combination therapy is recommended.
In order to improve the outcomes of patients with metabolic syndrome and T2DM, specific health checkups and specific health guidance have been implemented since 2008 based on the Japanese Law on Securing Medical Care for the Elderly [10]. The specified health checkup is a program to provide early screening for patients at risk of metabolic syndrome and to prevent the development of diabetes, hypertension, and dyslipidemia, which cause heart and cerebrovascular diseases [11]. On the basis of the results of the checkup, health guidance and consultation recommendations are given, and measures are taken to improve glycemic control in T2DM or to provide early treatment. Information from the specified health checkups was made available in nation-wide databases, such as JMDC [12], enabling evaluation of this program.
It is expected that early physician visits after detection of abnormalities in clinical test values will help prevent the worsening of lifestyle-related diseases. However, the association between early physician visit and prevention in T2DM has not been evaluated fully. We therefore sought to evaluate the benefits of early physician visits using claims-based cohort data from the JMDC database. Specifically, this study aimed to investigate the relationships between the timing of physician visit after a diagnostic HbA1c test for T2DM and the time to prescription of the first antidiabetic treatment in the claims-based cohort setting.
Furthermore, since there are a few reports on types of T2DM pharmacological therapies after health checkup, we aimed to clarify the actual treatment pattern, including injectable therapies.
Methods
Study Design and Data Source
We conducted a retrospective, longitudinal, observational cohort study, using data extracted from the JMDC administrative claims database (https://www.jmdc.co.jp/), which captures patient information and prescriptions from large samples of primary and secondary care physicians in Japan [13, 14]. The JMDC database contains medical and pharmacy (inpatient, outpatient, and pharmacy administrative) claims for employees of middle- and large-sized companies and their families, from several Japanese insurance companies belonging to the Health Insurance Association. The database mainly covers people between the ages of 20 and 74, and does not include those over the age of 75 years. The medical claims include basic demographics, diagnoses, procedures, and fees. This database is unique in that clinical data of an employee collected during annual health checks can be linked to receipt data from healthcare providers to the insurer, when the employee visits the healthcare provider allowing longitudinal analyses on events such as physician visits and drug prescriptions at the patient level [15, 16]. In the current study, data was analyzed from health checks recorded in JMDC, which contains claims data of approximately 5.2 million Japanese company employees from multiple health insurance providers. Permission to access the database was acquired from JMDC Inc. Since JMDC is a database of anonymized information, ethics committee approval and patient consent were not required. In this study, index date V1 was defined as the date of the first HbA1c checkup value of at least 6.5% (Supplementary Fig. S1); index date V2 as the first physician visit with an HbA1c test (Medical fee index, procedure code D005-9); index date V3 as the date of prescription of the first-line T2DM treatment; and index date V4 as the date of prescription of the second-line T2DM treatment. Patients were followed up for at least 24 months after the index date V3 (post-index period). A minimum period of 12 months of continuous enrollment in the database was required prior to index date V1 (the pre-index period) to determine patients’ characteristics.
Study Population
Adult patients who were naïve to T2DM treatment (those who were not prescribed any antidiabetic drug for at least 1 year prior to the index date V1) and had at least one health checkup record of an HbA1c value of at least 6.5% (National Glycohemoglobin Standardization Program, NGSP) during the selection period (1 January 2012–31 December 2016) were designated as the source cohort. The source cohort included people with at least one drug prescription intended to treat T2DM, after index date V1 during the study period. Those prescribed injectable antidiabetic agents at index date V3 were excluded from the time-to-event analysis as the database did not specify whether these treatments were prescribed for short-term treatment or long-term T2DM maintenance therapy.
Study Outcome
Study outcomes described treatment patterns in early vs. delayed physician visit for T2DM treatment, and the timing of commencing first-line and second-line T2DM treatment (defined as the duration from V2 to V3/V4), and prescription patterns of T2DM treatment in Japan.
Statistical Analysis
Coding of medical terms and medications was performed using the International Classification of Diseases (ICD)-10 and Anatomical Therapeutic Chemical Classification (ATC) codes, respectively. Included patients were grouped into the early and delayed physician visit groups, with the cutoff being the median number of days from the date of the first HbA1c value of at least 6.5% in the health checkup (index date V1) to the date of the first physician visit having HbA1c test (index date V2). The time to the first-line T2DM prescription and the time to second-line T2DM prescription of the two groups were compared using Kaplan–Meier survival analysis. The median (interquartile range, IQR), mean (standard error, SE), and 12-month rates were estimated. Both variables were further analyzed using multivariate Cox regression models, adjusting for relevant patient characteristics, including age group (20–34, 35–44, 45–54, 55–64, 65–74 years), sex, and comorbidities (hypertension, dyslipidemia) at baseline. All “time-to” analyses were only provided for the patients who were not treated by injection therapy in the first line. All analyses were performed using SAS software version 9.3.
Results
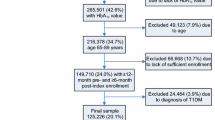
From the JMDC database, 101,699 patients with at least one HbA1c measure of at least 6.5% (index date V1) between 1 January 2012 and 31 December 31, 2016 were identified, of whom 5005 were followed up by a physician visit (index date V2) and subsequently prescribed antidiabetic treatment (index date V3). The mean age of the cohort was 50.4 years, with 82.7% male. The mean baseline HbA1c at index date V1 was 7.4%. A total of 34.1% of patients had hypertension and 25.6% had hyperlipidemia as comorbid conditions. These patients were classified into the early (n = 2506) or delayed (n = 2499) group, based on their time to first physician visit relative to the median of 109 days (42.0, 370.0) (Fig. 1). The baseline characteristics of the two groups and the overall population are summarized in Table 1 and Supplementary Table S1. From this cohort, 207 patients were excluded because of prescription of injection therapy at index date V3, leaving 4798 patients in the final analysis.
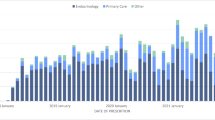
Dipeptidyl peptidase 4 inhibitors (DPP4i) were the most commonly prescribed therapeutic class in first-line therapy, both as monotherapy and combination treatment. Of all patients receiving first-line therapy, 59.5% received a prescription for DPP4i (Table 1). For patients on monotherapy, 52.4% of prescriptions were for DPP4i. Biguanides (BG) were the most commonly prescribed second-line therapy, with 35.2% of all patients receiving this drug class (Supplementary Tables S5 and S6). Other classes of T2DM therapies captured in the JMDC database include alpha-glucosidase inhibitors (α-GI), sodium-glucose cotransporter 2 inhibitors (SGLT2i), sulfonylureas (SU), insulin, thiazolidinediones (TZD), glinides, and glucagon-like peptide 1 receptor agonists (GLP-1RA).
Of the total population analyzed, 54.8% were prescribed their first-line T2DM therapy less than 2 months after detection of abnormal HbA1c (Table 2). Of the early group, 46.1% of patients were prescribed T2DM therapy in less than 2 months, whereas in the delayed group 63.4% of patients were prescribed T2DM therapy in the same time frame.
There was an increasing trend for prescription of T2DM therapy in less than 1 month as the baseline HbA1c increased (HbA1c 6.5–7.0% vs. HbA1c ≥ 9%; 37.8% vs. 86.1%, respectively; no statistical analysis) (Supplementary Table S2). In patients with HbA1c from 6.5% to 7%, 31.7% and 55.2% of patients in the early and delayed physician visit groups, respectively, were prescribed antidiabetics in less than 2 months. In patients with HbA1c from 7% to 8%, the corresponding prescription rates at 2 months were 48.0% and 66.3%, respectively. In patients with HbA1c ≥ 8%, minimal differences were observed between groups.
The early group experienced a longer median time to prescription of first-line (Fig. 2) and second-line (Fig. 3) antidiabetic drugs compared with the delayed group. For first-line treatment, the median time to prescription in the early vs. delayed physician visit groups was 92 days vs. 15 days (p < 0.0001), with a 12-month rate of 73.7% vs. 84.1% and a hazard ratio (HR) of 1.31 [95% confidence interval (CI) 1.24, 1.39] (Fig. 2). The early group had a statistically significant delay in time to prescription across all baseline HbA1c levels below 9% (Supplementary Table S3). For second-line treatment, the median time to prescription for the early vs. the delayed group was 1599 days vs. 1315 days (p < 0.0001), with a 12-month rate of 12.7% vs. 21.2% and an HR of 1.22 (95% CI 1.11, 1.34) (Fig. 3). The early group had a statistically significant delay in time to prescription across all baseline HbA1c levels (Supplementary Table S4). The delayed group was also more likely to receive combination therapy as first-line treatment than the early group (two-class combination: 11.5% vs. 6.3%; three classes or greater: 2.1% vs. 1.3%) (Table 1).
First-line treatment patterns: Time to first T2DM drug prescription (Kaplan–Meier curve) from V2 in study cohort. a Estimated using Kaplan–Meier analysis. b Multivariate Cox model adjusted on baseline characteristics: age, gender, BMI, comorbidities, T2DM drug at index date. BMI body mass index, CI confidence interval, HR hazard ratio, IQR interquartile ratio, KM Kaplan–Meier, T2DM type 2 diabetes mellitus
Second-line treatment patterns: Time to T2DM drug add-on (Kaplan–Meier curve) from V2 in study cohort. a Estimated using Kaplan–Meier analysis. b Multivariate Cox model adjusted on baseline characteristics: age, gender, BMI, comorbidities, T2DM drug at index-date. BMI body mass index, CI confidence interval, HR hazard ratio, IQR interquartile ratio, KM Kaplan–Meier, T2DM type 2 diabetes mellitus
Discussion
The Specific Health Examination and Specific Health Guidance System, which were introduced in Japan in 2008, were designed to screen and identify patients with undiagnosed T2DM or metabolic syndrome. It was expected that through early detection and physician visit, the clinical course of T2DM or metabolic syndrome may have a better outcome. No reports have examined the effectiveness of the program. This analysis provides important insight into the association of the timing of physician visit, early intervention, and progression of the treatment course of T2DM in the Japanese population, through analysis of claims data from the largest claims database, JMDC, which includes data from approximately 5.2 million people.
The key significance of this study is the demonstration of the benefit of early consultation after the detection of hyperglycemia at a health checkup in the claims-based cohort setting. In this study, early physician visit was associated with a delay in requiring prescription of first-line (92 vs. 15 days, p < 0.0001) as well as second-line T2DM therapies (1599 vs. 1315 days, p < 0.0001). Among patients with baseline HbA1c from 6.5% to 8%, a higher percentage of patients in the early physician visit group were not prescribed antidiabetic drugs, in less than 2 months, compared to the delayed physician visit group. It is presumed that the patients were commenced on medical nutrition and exercise therapy for less than 2 months, which is recommended by the Japanese Clinical Practice Guideline for Diabetes. One possible explanation for the longer time to requiring first- or second-line T2DM medications is the early effect of glycemic control, known as “legacy effect” [17]. On the basis of Supplementary Tables S3 and S4, the number of days between the first-line treatment and the second-line treatment was particularly large in the early physician visit group, indicating the potential effect of early physician visit and instituting diet and exercise therapy.
It is noteworthy that patients with comorbidities such as hypertension, dyslipidemia, and older age had an earlier first consultation with a physician. This may be due to prioritization of these patients by physicians after an abnormal HbA1c finding and increased cardiovascular risk profile. Equally, patients with comorbid conditions may seek earlier medical intervention because of health concerns. The higher prevalence rates of hypertension and dyslipidemia in the group who visited the hospital earlier may also be due to the earlier finding of hyperglycemia during patient visits for the treatment of comorbidities. The presence of hypertension and dyslipidemia has been reported to increase the risk of T2DM [18, 19]. However, despite the high prevalence of hypertension and dyslipidemia, subsequent antidiabetic treatment after an early visit (for the treatment of diabetes) was delayed. Since it has also been reported that antihypertensive drugs and antihyperlipidemic drugs affect the onset of T2DM [20, 21], it may be necessary to investigate the effect of early consultation on subsequent antidiabetic drugs and the progression of diabetic conditions in the population without hypertension or dyslipidemia. Usual care for hypertension and dyslipidemia may also affect the timing of diabetes treatment; these effects may also need further investigation.
The slower progression of the treatment course of T2DM associated with early physician visits in this study may result in significant economic benefits, with a potential reduction in costs from reduced diabetic complications and cost of T2DM medications [22]. This potential economic benefit may be particularly important in the setting of an aging population with potentially increased T2DM prevalence in Japan [23]. Therefore, not only early visit but also prevention of clinical inertia and appropriate diabetes education may lead to economic benefits, so it is necessary to pay attention to them, but further analysis is required in the future.
The Japanese guidelines recommend at least 2–3 months of treatment by lifestyle modifications before prescribing antidiabetic medications [9]. However, in this study, 54.8% of patients were prescribed oral hypoglycemics in less than 2 months. In addition, combination therapy as first-line therapy was also more frequently observed in the delayed physician visit group. These deviations demonstrated a substantial gap between the national guidelines and the current clinical practice in Japan. If this is due to a lack of knowledge of the guidelines among physicians who diagnose and treat patients with T2DM, there may be a role for more intensive education on the benefits of lifestyle modification, to bridge knowledge gaps. Alternatively, this gap could be due to patients not adhering to physician advice [24], in which case, tailored educational efforts could be directed at patients. We believe further research may be required to better understand the practice gap in order to develop interventions enhancing T2DM patient care.
It is interesting to note that DPP4i was the most frequently prescribed T2DM therapeutic class in first-line therapy. In global T2DM guidelines, such as those of the American Diabetes Association [25], metformin is recommended as first-line pharmacological therapy. Metformin is a relatively safe oral hypoglycemic agent, with a well-established safety profile and is generally inexpensive. However, Japanese T2DM guidelines do not specify the order of use of different classes of T2DM therapies. Rather, physicians are encouraged to tailor therapeutic choice on the basis of patient characteristics, which partly explains the variance with international practice. The finding of DPP4i being the most frequently prescribed T2DM therapy in Japan is also consistent with previously published data from Nishimura et al. [26]. Another possible explanation is that JMDC captured patients whose T2DM therapies were covered by insurance, therefore de-incentivizing prescribing physicians from limiting treatment costs.
The key strength of this study is the large pool of patients provided by the JMDC database, covering 5.2 million patients. As this is not a randomized controlled trial, many of the potential selection biases and confounding factors have been accounted for by using an adjusted model.
One limitation of this study is that the study design is not a prospective randomized controlled trial. In the study, the onset of T2DM was assumed to be at the time of an abnormal HbA1c reading at an annual health check. This is because in the JMDC database test values at the time of health check can be identified, but test values at the time of medical examination cannot be identified because of insufficient registration. But in reality, the commencement of the disease is insidious and likely to precede the time of abnormal HbA1c, and the actual time of onset of T2DM in each case is not known. Furthermore, the data captured for each patient are dependent on the quality of the information input by the healthcare professional, which is a common limitation in studies using electronic medical records. Another limitation is the demographic range of the patients in this database (20–74 years old), which does not cover a significant number of aged adult patients (75 years or older) with new-onset of T2DM [13, 27]. There was also a scarcity of data for patients aged 65 years or older in the dataset used in this study. Patient factors may also be a limitation, in that it was assumed that all patients filled their prescriptions and were adherent to their medication. In addition, this health check system is unique to Japan and may not be generally applicable to overseas subjects. Finally, as this study is a retrospective analysis from a claims database, some important data was not captured, which could have provided relevant information, such as reasons for stopping treatment, pill dumping or stockpiling, whether adequate diet and exercise treatment was instituted by the physician at the first visit and practiced by the patient, follow-up HbA1c at V2 and V3 time points, and the incidence of macro- and microvascular complications.
Conclusion
This claims-based cohort study demonstrated that early physician visit following the diagnosis of T2DM in Japanese patients is associated with an improved clinical course of their disease, as demonstrated by a longer period of time before requiring T2DM medications. There is an opportunity to improve physicians’ adherence to the Japanese DM guidelines by instituting adequate lifestyle modifications prior to prescribing T2DM treatments.
References
WHO. Diabetes 2018. https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed on 23 April 2020.
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. https://doi.org/10.1038/nrendo.2017.151.
American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–46. https://doi.org/10.2337/dc12-2625
National Healthcare Expenditure 2017. Tokyo: Japan Ministry of Health, Labor and Welfare; 2017.
Overview of 2005 National Healthcare Expenditure. Tokyo: Ministry of Health, Labor and Welfare.
Overview of 2017 National Healthcare Expenditure. Tokyo: Ministry of Health, Labor and Welfare.
Paul SK, Klein K, Thorsted BL, Wolden ML, Khunti K. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14:100. https://doi.org/10.1186/s12933-015-0260-x.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–53.
Haneda M, Noda M, Origasa H, et al. Japanese clinical practice guideline for diabetes 2016. Diabetol Int. 2018;9(1):1–45. https://doi.org/10.1007/s13340-018-0345-3.
Work Group for Studying the Effects of the Specific Health Checkups and Specific Health Guidance on Health Care Expenditures. Effects of rationalization of medical expenses for specific medical examinations and health guidance 2020. Tokyo: Ministry of Health, Labour and Welfare; 2020.
Yamamoto H. Health checkups and healthcare advice with a particular focus on the metabolic syndrome in the health care system reform. J Natl Inst Public Health. 2008;57(1):3–8.
Tsushita K, Hosler AS, Miura K, et al. Rationale and descriptive analysis of specific health guidance: the nationwide lifestyle intervention program targeting metabolic syndrome in Japan. J Atheroscler Thromb. 2018;25(4):308–22. https://doi.org/10.5551/jat.42010.
Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20(5):413–9.
Tanaka S, Seto K, Kawakami K. Pharmacoepidemiology in Japan: medical databases and research achievements. J Pharm Health Care Sci. 2015;1:16. https://doi.org/10.1186/s40780-015-0016-5.
Takeuchi M, Kawakami K. Association between hemoglobin and hemoglobin A(1c): a data-driven analysis of health checkup data in Japan. J Clin Med. 2018;7(12):539. https://doi.org/10.3390/jcm7120539.
Ihana-Sugiyama N, Sugiyama T, Tanaka H, Ueki K, Kobayashi Y, Ohsugi M. Comparison of effectiveness and drug cost between dipeptidyl peptidase-4 inhibitor and biguanide as the first-line anti-hyperglycaemic medication among Japanese working generation with type 2 diabetes. J Eval Clin Pract. 2020;26(1):299–307. https://doi.org/10.1111/jep.13171.
Chalmers J, Cooper ME. UKPDS and the legacy effect. N Engl J Med. 2008;359(15):1618–20. https://doi.org/10.1056/NEJMe0807625.
Haile K, Timerga A. Dyslipidemia and its associated risk factors among adult type-2 diabetic patients at Jimma university medical center, Jimma, Southwest Ethiopia. Diabetes Metab Syndr Obes. 2020;26(13):4589–97. https://doi.org/10.2147/DMSO.S283171.
Díaz Vera AS, Abellán Alemán J, Segura Fragoso A, et al. The prevalence and risk factors associated with dyslipidemia in type 2 diabetic patients in the autonomous region of Cantabria. Endocrinol Diabetes Nutr. 2020;67(2):102–12.
Grimm C, Köberlein J, Wiosna W, Kresimon J, Kiencke P, Rychlik R. New-onset diabetes and antihypertensive treatment. GMS Health Technol Assess. 2010;6:Doc03. https://doi.org/10.3205/hta000081.
Chogtu B, Magazine R, Bairy KL. Statin use and risk of diabetes mellitus. World J Diabetes. 2015;6(2):352–7. https://doi.org/10.4239/wjd.v6.i2.352.
Pratley RE. The early treatment of type 2 diabetes. Am J Med. 2013;126(9 Suppl 1):S2-9. https://doi.org/10.1016/j.amjmed.2013.06.007.
Kalyani RR, Golden SH, Cefalu WT. Diabetes and aging: unique considerations and goals of care. Diabetes Care. 2017;40(4):440–3. https://doi.org/10.2337/dci17-0005.
O’Connor PJ, Sperl-Hillen JM, Johnson PE, et al. Clinical inertia and outpatient medical errors. Advances in patient safety: from research to implementation (Volume 2: Concepts and Methodology). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005.
American Diabetes Association. 9. pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S90-S102. https://doi.org/10.2337/dc19-S009.
Nishimura R, Kato H, Kisanuki K, et al. Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims-based cohort study. BMJ Open. 2019;9(3):e025806. https://doi.org/10.1136/bmjopen-2018-025806.
JSPE Database Index. https://sites.google.com/view/jspedatabaseindex/jmdc-payer-based.
Acknowledgements
We acknowledge Vicki Tse of MIMS for writing support during the development of this manuscript, which was funded by Takeda Pharmaceutical Co. Ltd. (Tokyo, Japan), and complied with Good Publication Practice 3 ethical guidelines (Battisti et al., Ann Intern Med. 2015;163:461–464). We would also like to thank Yoshie Onishi, DrPH, employees of Creativ-Ceutical K.K., for data analysis support. We extend our thanks to the participants of this study.
Funding
This work was supported by the study sponsor, Takeda Pharmaceutical Company Limited, Tokyo, Japan. The study sponsor is also supporting the journal’s Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
HW, YK, KT, AO, NN, KF and MA contributed to the study design. YK, KT, AO, NN and KF contributed to the conduct and data collection. YK, KT, AO, NN, TN and KF contributed to the analysis.
Disclosures
Hirotaka Watada has received honoraria from Astellas Pharma K.K., AstraZeneca, Boehringer Ingelheim Co. Ltd, Dainippon Sumitomo Pharma Co. Ltd., Eli Lilly Japan K.K., Fuji Film, Kyowa Hakko Kirin, Mitsubishi Tanabe Pharma, Merck Sharp & Dohme, Novo Nordisk, Ono Pharmaceutical, Sanofi, Sanwa Kagaku Kenkyusho Co. Ltd. and Terumo Corporation. He has received research grants from Abbott Japan, Astellas Pharma K.K., Boehringer Ingelheim Co. Ltd, Daiichi Sankyo, Dainippon Sumitomo Pharma Co. Ltd., Kissei Pharma, Kowa Pharmaceutical Co. Ltd., Kyowa Hakko Kirin, Eli Lilly Japan K.K., Sanwa Kagaku Kenkyusho Co. Ltd., Mitsubishi Tanabe Pharma, Merck Sharp & Dohme, Novartis Pharma K.K., Novo Nordisk, Ono Pharmaceutical, Pfizer, Sanofi, Souiken, Takeda Pharmaceutical Co. Ltd, Teijin, Taisho-Toyama and Yakult Pharmaceutical Industry Co., Ltd. Manabu Akazawa has received consulting fees from Janssen Pharmaceutical K.K., Pfizer and Takeda Pharmaceutical Co. Ltd. Yasushi Kawakita, Keiko Tanaka, Akinori Oh, Nobuhiro Nishigaki, Tadashi Nakajima and Keita Fujikawa are employees of Takeda Pharmaceutical Co. Ltd.
Compliance with Ethics Guidelines
This was a retrospective study that included anonymized data from an insurance claims database. Hence, ethics committee approval was not required. Given the nature of the study, informed consent of each participant could not be acquired. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. Based on the Ethical Guidelines for Epidemiological Research issued by the Japanese Ministry of Health, Labour and Welfare, ethics approval was not applicable to this study and was not required. Permission to access the database was acquired from JMDC Inc.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due the need for the appropriate licenses from the owner (JMDC Inc.) to access the data. For inquiries about access to the data set used in this study, please contact JMDC (https://www.jmdc.co.jp). The study made use of de-identified data from the JMDC databases. The opinions, results and conclusions reported are those of the authors. No endorsement by JMDC or any of its funders or partners is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Watada, H., Kawakita, Y., Tanaka, K. et al. A Claims-Based Cohort Study on the Treatment Patterns of Japanese Patients with Type 2 Diabetes Mellitus and the Association of Early First Physician Visit with Time to Prescription of Oral Hypoglycemic Agents. Diabetes Ther 12, 2035–2047 (2021). https://doi.org/10.1007/s13300-021-01090-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01090-2