Abstract
Introduction
Understanding comorbid conditions with type 2 diabetes mellitus (T2DM) is critical for clinical decision-making regarding the choice of pharmacotherapy. This study aimed at describing the prevalence and co-prevalence of comorbidities, including chronic kidney disease (CKD) and cardiovascular disease (CVD) (coronary artery disease (CAD), cerebrovascular disease, peripheral arterial disease (PAD) and congestive heart failure (CHF)) among patients with T2DM.
Methods
A cross-sectional multi-center observational study on 300 patients with T2DM. Data were collected from patients’ records during the enrollment visit.
Results
Overall, 38%, 10% and 2% of the patients had one, two and three comorbidities, respectively, with the number of comorbidities significantly increasing with age. The most prevalent comorbidities were CVD (17.3%), CAD (15%) and CKD (44.3%), mostly stages 2 and 3. However, the prevalence of CHF (0.7%), PAD (2.3%) and cerebrovascular diseases (1.3%) was low. The highest percentage of anti-hyperglycemic agents used was metformin (81%), dipeptidyl peptidase-4 inhibitors (46%), sodium-glucose co-transporter 2 inhibitors (37%), insulin (36%) and sulfonylurea (34%). The choice of the anti-hyperglycemic class did not change across age groups and gender.
Conclusion
Half of the patients had T2DM only. The most prevalent comorbidity found was CKD, mainly stage 2. The comorbidity burden tended to increase significantly in older age groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Understanding comorbid conditions with type 2 diabetes mellitus (T2DM) is critical for clinical decision-making regarding the choice of pharmacotherapy. |
This study aimed at describing the prevalence and co-prevalence of comorbidities, including chronic kidney disease (CKD) and cardiovascular disease (coronary artery disease (CAD), cerebrovascular disease, peripheral arterial disease (PAD) and congestive heart failure (CHF)), among patients with T2DM. |
The most prevalent comorbidities were CKD (44.3%), mostly stages 2 and 3, and CAD (15%). The prevalence of CHF (0.7%), PAD (2.3%) and cerebrovascular diseases (1.3%) was low. |
Clinicians need to proactively screen for the presence of comorbid conditions with T2DM, especially CKD and CAD. The CHF co-prevalence may be underestimated and underdiagnosed, being a relatively newly focused emerging comorbidity. |
Highlights
Chronic kidney disease is a main concern in the management of type 2 diabetes mellitus. Comorbidity burden is of additional significance in elderly patients.
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.14054798.
Introduction
Diabetes mellitus is a progressive disease affecting an estimated 415 million people worldwide [1]. Type 2 diabetes mellitus (T2DM) accounts for 85–95% of all cases of diabetes.
The association between T2DM and cardiovascular disease (CVD) has been studied extensively over the past 30 years, with reference to the Framingham study, wherein patients with T2DM had a higher incidence of CVD than those without T2DM [2]. Specifically, the risk of heart disease or stroke is 2–4 times higher in patients with diabetes than in those without diabetes. Furthermore, at least 68% of diabetes patients who are 65 years of age or older are expected to die as a result of heart disease, while 16% are expected to die of a stroke [3].
Recent trials on cardiovascular outcomes have demonstrated that certain antihyperglycemic agents could have benefits beyond glucose lowering, especially for patients with established CVD. For example, a trial on cardiovascular outcomes of empagliflozin, a sodium-glucose co-transporter 2 inhibitor (SGLT2i), demonstrated a significant reduction in the composite outcome of major adverse cardiovascular events [4]. Some trials for the glucagon-like peptide 1 (GLP-1) analog class have shown lower rates of the same composite end point [5, 6].
Although many classes of antihyperglycemic agents are currently available to treat T2DM, it is imperative to match the patient’s clinical profile to the appropriate antihyperglycemic agent. Given the heterogeneity within the T2DM population, the American Diabetes Association guidelines underscore the importance of individualizing a patient’s T2DM management based on their profile, which includes comorbid conditions [7]. While CVD is an important factor in patient management, the clinical profile of patients with T2DM remains complex. Moreover, various factors, such as chronic kidney disease (CKD), risk of hypoglycemia and many others should be considered.
Given that T2DM is among the leading causes of CKD, patients with T2DM often develop decreased renal function. Accordingly, selecting appropriate therapy requires physicians to consider the presence of CKD. For example, metformin is not suitable for patients with estimated glomerular filtration rate (eGFR) < 30 and requires precautions for use in patients with an eGFR < 45 [8]. Sulfonylureas can cause hypoglycemia and have been linked to increased risk of both mortality and CVD in some studies [8, 9], while most dipeptidyl peptidase-4 inhibitors (DPP-4i) require a renal dose adjustment. SGLT2i, the newest class of oral antihyperglycemic agents for patients with T2DM [10], is contraindicated in patients with severe renal impairment and warrants cautious use among those with less severe renal insufficiency.
Understanding comorbid conditions is critical for clinical decision-making regarding the choice of pharmacotherapy. Although previous studies have examined the prevalence of select comorbidities in patients with T2DM, no recent study in the Gulf countries has examined the prevalence of CVD and CKD in patients with T2DM. Therefore, this descriptive study sought to quantify the prevalence of comorbidities, including CKD and CVD [coronary artery disease (CAD), cerebrovascular disease, peripheral arterial disease (PAD) and congestive heart failure (CHF)] among patients with T2DM. Additionally, we aimed to determine the prescription patterns of antihyperglycemic agents in terms of class in patients with T2DM and CVD, CKD and CHF.
Methods
Ethical Conduct of the Study
This study complied with the recommendations of the 18th World Health Congress (Helsinki, 1964) and all applicable amendments, as well as the laws and regulations and any applicable guidelines of Kuwait and the UAE, where the study was conducted. The authors state that they have received approval from the following institutional review boards on the conduct of the study: Dubai Health Authority DSREC (Dubai Scientific Research Ethics Committee), UAE Ministry of Health & Prevention Research Ethics Committee, Dasman Diabetes Institute Kuwait Ethics Review Committee and Kuwait Ministry of Health Ethics Review Committee. All subjects provided informed consent to participate in the study.
Study Design
This cross-sectional multi-center observational study included patients who visited six study sites across the UAE and Kuwait between 7 February 2019 and 31 May 2019. The first 300 patients with T2DM who satisfied the inclusion criteria and signed the consent forms were included. The sites in each country included one secondary care public hospital, one primary care public clinic and one private clinic or hospital. Patients were distributed over the six sites while trying to ensure even distribution among the three different sectors. If any of the sites were unable to recruit the target number of patients, other sites were used to compensate for the lack of patients. Data from patients’ records were collected at the enrollment visit.
Population
A total of 300 residents of UAE or Kuwait with T2DM who visited the study sites within the indicated period were enrolled. All inclusion and exclusion criteria were reviewed by the investigator or a qualified designee to ensure that each patient was qualified for the study. Patients were identified as having the disease of interest based on either their recorded diagnosis or medications used. In sites using EMR, codes were used to determine the diagnosis.
Inclusion Criteria
-
Patients diagnosed with T2DM by a physician prior to enrollment.
-
Eighteen years or older at the enrollment visit.
-
Patients visiting the study site at least once during the period of 1 September 2018 to 31 May 2019.
-
Patients who have had a clinical record in the healthcare center for at least 1 year prior to enrollment.
-
Patients with records of current anti-hyperglycemic agents available at enrollment.
Exclusion Criteria
-
Patients diagnosed with type 1 diabetes mellitus.
-
Patients with gestational diabetes mellitus.
-
Patients with other form of secondary diabetes.
-
Inability to provide consent.
Medication
This is an observational study; patients received treatments based on the physician’s preference without any interference. As part of the secondary objectives of this study, anti-hyperglycemic agents were recorded per patient and analyzed in terms of class.
Outcomes
Primary Outcomes
The primary outcomes included the co-prevalence data, which encompassed the prevalence of CKD and CVD, in addition to the individual components of CVD [cerebrovascular disease, peripheral arterial disease (PAD), congestive heart failure (CHF) and coronary artery disease, which included patients diagnosed with one or more of the following conditions: coronary artery disease, prior MI, prior coronary artery bypass grafting (CABG), prior percutaneous coronary intervention (PCI) and ischemic heart disease] as well as the proportion of patients with one, two or three conditions.
Secondary Outcomes
The secondary outcomes included the prevalence of CVD, CHF and CKD stratified by age, gender, country and clinic type as well as the counts and percentage of patients with different stages of CKD defined as per their eGFR levels, the prevalence of each CKD stage with other comorbidities included in this study, the count and percentage of patients having T2DM and CVD and CKD according to anti-hyperglycemic agent class.
Statistical Analysis
Sample Size
We estimated that around 300 patients would be recruited during the index period within the study sites. The study aimed to recruit a diverse selection of patients with T2DM from the included sites in the UAE and Kuwait.
Statistical Methods
Descriptive statistics were used to describe the baseline demographic data and clinical characteristics. This included variables such as age, gender, race, smoking status, residential location, duration of T2DM, most recent HbA1c, blood pressure, lipid levels, kidney function, most recent weight/body mass index (BMI), distribution of T2DM treatment by class and the proportion of patients by treatment type (none, mono, dual and triple). Categorical variables were presented by percentages, whereas continuous variables were initially assessed for normality using the Kolmogorov-Smirnov test or Shapiro-Wilk test. Data found to be normal were presented by means and standard deviations, or medians and interquartile ranges when the distribution was non-normal or skewed, thus following a non-parametric distribution. The strength of the association between two comorbidities was studied using phi correlation coefficients.
The significance level was two sided, with a type 1 error of 5%. All analyses were conducted using the Statistical Package for Social Sciences version 24 (SPSS-24).
Results
Patients Characteristics
The study enrolled 300 patients with T2DM. All 300 patients fulfilled the exclusion and inclusion criteria. About 130 patients were recruited from UAE centers, while 170 patients were recruited from Kuwait centers.
Demographics and Baseline Characteristics
Demographics
Patients had a median age of 57 years with an interquartile range (IQR) between 49 and 64, with 58% being males (n = 174), 42.3% (n = 127) being Kuwaiti and 15.3% (n = 46) being Emirati. Most patients (69.3%) were never smokers and lived in urban areas (89.7%). Gender distribution, smoking status and residence location did not differ significantly across age groups. Smoking was significantly more common among males than females (19% vs. 1.6%; p < 0.001). The majority of Emirati patients (n = 31, 67.4%) and Asians (n = 36, 70.7%) were recruited from primary care public clinics, and the majority of Kuwaiti patients (n = 67, 52.7%) were recruited from secondary care public hospitals, whereas Arabs other than Emirati and Kuwaiti nationals were recruited mainly (n = 64, 78.5%) from private hospitals, with the difference being significant (p = 0.001). About 93% of suburban patients were recruited from private hospitals compared to 26% of urban patients (p = 0.001). Patients attending secondary care public hospitals [62 (56–67) years old] were significantly older than those attending primary care public clinics [54 (47–62) years old] and private hospitals [55 (47–62) years old] (p < 0.001). Supplementary Table 1 summarizes the description of socio-demographic characteristics of the study population, overall, by age group and by gender.
Clinical Characteristics
The median HbA1c level was 7.4% in the overall population and was similar across all age and gender groups (p = 0.27 and p = 0.30, respectively). The median (IQR) total cholesterol, low-density lipoprotein (LDL) and triglyceride levels were 151 (128–193) mg/dl, 85 (59–120) mg/dl and 131 (89–177) mg/dl, respectively. These values all decreased with increasing age when comparing patients aged < 65 years and those aged between 65 and 74 years (p = 0.01). No statistical difference in any of the aforementioned clinical parameters was observed among those aged 75 and above and other age groups, perhaps due to the small number of patients aged 75 and above (n = 15). The median (IQR) high-density lipoprotein (HDL) level was 43 (35–50) mg/dl, with no significant difference across age groups. Moreover, we found no significant differences in triglycerides and LDL levels between males and females (p = 0.08). However, females had significantly higher total cholesterol and HDL levels compared to males (p = 0.004 and p < 0.001, respectively) (Table 1). A total of 99 patients (33%) had an LDL level < 70 mg/dl.
The overall population had a median BMI of 30.4 (27.0–34.5) kg/m2, with no significant difference across age groups (p = 0.45). However, females had a higher median BMI of 31.9 (28.2–36.3) kg/m2 than males [29.1 (26.0–33.1) kg/m2] (p = 0.007) (Table 1). Table 2 summarizes the distribution of clinical parameters according to clinic type, showing that patients attending private hospitals had a higher BMI compared to those attending primary care public clinics (p = 0.02). Regarding total cholesterol and LDL levels, those attending private hospitals had the highest levels, followed by those attending primary care public clinics and secondary care public hospitals (p < 0.001), whereas, no differences were observed in HDL and HbA1C levels across different clinic types.
Regarding triglyceride levels, those attending primary and secondary care public clinics/hospitals had lower levels compared to those attending private hospitals (p = 0.014 and 0.005, respectively). Patients from secondary care public hospitals had significantly higher serum creatinine levels, had longer T2DM duration and were older when diagnosed with T2DM (p < 0.001). Additionally, secondary care public hospitals had a higher proportion of patients with one and two comorbidities compared to primary care clinics and private hospitals (Table 2).
Description of Comorbidities
Half of the patients had T2DM only with no associated CVD or CKD, 38% had one comorbidity, 10% had two comorbidities, and 2% had three comorbidities in addition to T2DM. The number of comorbidities significantly increased with age (p < 0.001) (Table 1).
Study Outcomes
Primary Outcome: Prevalence of All Comorbidities
The prevalence of CVD, CAD and all stages of CKD was 17.3%, 15% and 44.3%, respectively. The prevalence of CHF, PAD and cerebrovascular diseases was 0.7%, 2.3% and 1.3%, respectively. Most patients with CKD had stage 2 (21%) or stage 3 (14%). CKD prevalence was higher in Kuwait (60%) compared to the UAE (24%) (p < 0.001); however, no statistically significant difference was shown between countries regarding CVD and CAD, as shown in Table 3, which demonstrates the distribution and co-distributions of major comorbidities, overall and across countries.
Secondary Outcomes
Stratification of Demographic and Clinical Variables According to Specified Age Groups and Gender
Our results show that CVD, CAD and CKD increased significantly with increasing age (p < 0.001). Furthermore, the proportions of males with CAD and CVD were significantly higher compared to females (p = 0.04 and p = 0.015, respectively). CKD distribution did not differ between males and females (p = 0.8); however, it was the only comorbidity that was significantly more frequently found among patients enrolled in Kuwait compared to those enrolled in the UAE (60% vs. 24%; p < 0.001). Patients attending secondary care public hospitals had the highest rates of CVD (35%) and CKD (69%) compared to those attending other types of clinics (Table 4).
Among the study population, the combination of CVD and CKD (11.7%) demonstrated the highest co-prevalence, followed by CAD and CKD (9.7%). Moreover, CKD was associated with both CVD and CAD (p < 0.001), with a phi correlation coefficient of 0.23 and 0.19, respectively.
Supplementary Table 2 describes the co-prevalence (%) of comorbidities in patients with T2DM by gender.
Description of Antihyperglycemic Agent Classes
Metformin was the most frequently prescribed antihyperglycemic agent (81%), followed by DPP4 inhibitors (46%), SGLT2 inhibitors (37%), insulin (36%) and sulfonylureas (34%). The choice of the anti-hyperglycemic class did not change across age groups and gender. Approximately 32% of patients were being treated with a combination of two antihyperglycemic agents and 30% with a combination of three antihyperglycemic agents. There was no significant difference across age groups and gender (p = 0.1).
Patients with T2DM and CVD were most frequently prescribed metformin (69%), followed by insulin (58%), DPP4 inhibitors (53.8%) and SGLT2 inhibitors (38%). Patients with T2DM and CKD were most frequently prescribed metformin (74.4%), followed by insulin (58%), DPP4 inhibitors (41.4%), SGLT2 inhibitors (37%) and sulfonylureas (35%). Similarly, patients with T2DM who had no comorbidities were most frequently prescribed metformin (87.4%), followed by DPP4 inhibitors (47.7%), SGLT2i (35.1%) and SUs (34.4%) (Table 5). Metformin was significantly more frequently prescribed when no comorbidities were present (p = 0.007), whereas insulin and GLP-1RA were significantly more frequently prescribed among those with CKD than among those with CVD and no comorbidities (p < 0.001 and p = 0.011, respectively). There was no association observed between the presence or absence of comorbidities and the prescription of DPP4 inhibitors, SGLT2 inhibitors or SUs.
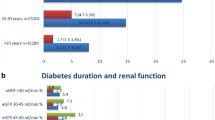
The presence of CVD, CAD and PAD was significantly associated with a longer T2DM duration (13 vs. 5 years, p < 0.001; 12 vs. 5 years; p = 0.001; and 25 vs. 7 years, respectively; p = 0.001) (Supplementary Table 3).
After comparing T2DM disease durations according to CKD stages, we found that patients with stage 1 CKD had significantly lower disease duration compared to stages 2, 3 and 5 (p = 0.004, p < 0.001 and p = 0.01, respectively). Patients with stage 2 CKD had significantly lower disease durations compared to those with stage 3 (p = 0.012). The co-prevalence of CVD and CKD was significantly associated with longer T2DM disease duration (Supplementary Table 3).
Among the included patients, 11 (3.7%) did not have CVD, were aged ≥ 50 years, were obese or were classified as current or former smokers.
The HbA1c levels were significantly higher among patients with CAD (7.9% vs. 7.4%; p = 0.027) and CKD (7.7 vs. 7.1; p = 0.03) compared to those without. The co-prevalence of comorbidities was not significantly associated with HbA1C levels.
The HbA1C levels were also significantly associated with the number of anti-hyperglycemic agents. Patients receiving one agent had a significantly lower HbA1C level (7.0% ± 1.4%) compared to those receiving three (8.1% ± 1.5%) or four agents (8.5% ± 1.7%) (p < 0.001 in both cases). Patients receiving two agents had a significantly lower HbA1C level (7.3% ± 1.4%) compared to those receiving three (8.1% ± 1.5%) or four agents (8.5% ± 1.7%) (p = 0.002 and p < 0.001, respectively). The mean HbA1C level reached 8.5% ± 1.6% among insulin users. The highest percentage of insulin users was among study participants attending secondary care hospitals, where insulin users represented 66% of patients enrolled from secondary care hospitals compared to 29% in private clinics and 13% in primary care clinics.
Among the 52 patients with CVD, 6 (11.5%) received GLP1 RA only, 14 (27%) received SGLT2 inhibitors only, and 6 (11.5%) received both GLP1 RA and SGLT2 inhibitors. Overall, 50% of CVD patients received GLP1 RA and/or SGLT2 inhibitors. Among the patients without CVD, 14 (5.6%) received GLP1 RA only, 64 (25.8%) were on SGLT2 inhibitors only, and 27 (10.9%) received both GLP1 RA and SGLT2 inhibitors. The association between the use of these two anti-hyperglycemic agents and their combination and CVD status did not reach statistical significance.
A total of 12 patients had CVD and an eGFR below 45, among whom one individual (8%) received SGLT2 inhibitors. Furthermore, 40 patients had CVD and an eGFR ≥ 45, among whom 19 (48%) received SGLT2 inhibitors.
Discussion
In this cross-sectional, observational study, the prevalence of comorbidities among 300 patients with T2DM was determined, including CKD and CVD (CAD, cerebrovascular disease, PAD and CHF).
The median age of patients enrolled in the present study was 57 years, the median HbA1c level was 7.4%, the median BMI was 30.4 (27.0–34.5) kg/m2, and the median LDL was 85 (59–120) mg/dl. Additionally, 69.3% of the total population had never smoked. These clinical characteristics were generally similar to those in another study conducted in the UAE by Jelinek et al. on 490 patients with T2DM, where the mean age of patients was 61, the mean BMI was 32, the mean HbA1c was 7.75%, the mean LDL was 2.01 mmol/l (78 mg/dl), and 72% of patients had never smoked [11]. However, patients included in that study were all recruited from tertiary hospitals while patients in our study were recruited, based on an even distribution, from secondary care public hospitals, primary care public clinics and private clinics/hospitals.
Our study found that the most common comorbidity among patients with T2DM was CKD—mainly stage 2, followed by CVD and CAD, representing 44.3%, 17.3% and 15%, respectively, whereas CHF was the least common, representing only 0.7%. Additionally, CKD, CVD and CAD were found to increase significantly with age. Similarly, the study by Jelinek et al. showed that 54% of the patients had eGFR < 90 and 10% had CAD. This study also showed that the number of complications varied with age, where multiple complications were typically seen in patients over the age of 65 years [11]. Moreover, a systematic review from across the world conducted by Einarson et al. reported that 32.2% of 4,549,481 patients with T2DM had CVD, 29.1% had atherosclerosis, 21.2% had coronary heart disease, 14.9% had heart failure, 14.6% had angina, 10.0% had MI, and 7.6% had a stroke [12]. The study by Jelinek et al. reported one or more diagnosed complications in 83.47% of patients with T2DM. The most prevalent diabetic complications were found to be retinopathy (13.26%) and CAD (10.20%). Additionally, nephropathy and neuropathy were the most prevalent combined complication (8.57%). Nephropathy was only found in 5.92% of patients despite the high frequency of suboptimal renal profiles [11].
Furthermore, a study by Iglay et al. regarding the prevalence and co-prevalence of comorbidities among patients with T2DM in the US found that CKD, CVD and CHF had a prevalence of 24.1%, 21.6% and 7.4%, respectively. This same study also showed that the comorbidity burden tended to increase in older age groups [13]. Another study conducted in Kuwait also showed that the coexistence of comorbidities and T2DM increased with advancing age, where it increased to 47.3% in the age group > 55 years [14].
Moreover, in our study, the proportion of males with CAD and CVD were significantly higher compared to females; however, the CKD distribution did not differ between the two genders, which is consistent with the study by Iglay et al. also showing that comorbidities among patients with T2DM are more prevalent in males [13]. However, another study conducted by Nowakowska et al. on 102,394 patients showed different findings, where comorbidities were more commonly found in female patients; this study included a wider selection of 18 different comorbidities, including CHD, CKD, atrial fibrillation, stroke, rheumatoid arthritis, osteoporosis, depression and hypothyroidism, compared to the present study [15].
Additionally, our study showed that CKD prevalence was higher in Kuwait (60%) compared to the UAE (24%) (p < 0.001), which could be due to the fact that 70 patients in Kuwait were recruited from a secondary care public hospital compared to only 30 patients in the UAE.
Approximately 50% of the patients in our study had T2DM with no associated CVD or CKD while 38% had one comorbidity, 10% had two comorbidities, and 2% had three comorbidities in addition to T2DM. The highest co-prevalence was seen as a combination of CVD and CKD (11.7%), followed by CAD and CKD (9.7%). Furthermore, the presence of CVD, CAD and PAD was significantly associated with longer T2DM duration. This is in agreement with other studies showing that CKD and CVD are among the most common comorbid conditions associated with T2DM [11, 13]. Moreover, the following co-prevalence was also noted in the study by Iglay et al.: CVD + CKD 8.6%, CVD + CHF 4.2% and CKD + CHF 4.1% [13].
Our study showed that metformin (81%) was the most commonly administered antihyperglycemic agent, followed by DPP4 inhibitors (46%). This is similar to the findings of a study conducted in Qatar, stating that the most commonly prescribed diabetes medication was metformin (89.9%), followed by DPP4 inhibitors (61.1%) and sulfonylureas (49.3%) [16]. In the present study, the choice and number of the anti-hyperglycemic agents/class did not differ across age and gender. Patients with T2DM and CVD or CKD were also most frequently prescribed metformin. This is consistent with the consensus recommendations by Basheir et al. [17] and a diabetes study in the Arabian Gulf [18].
Our study was focused on CVD and CKD. Data related to other key comorbidities such as hypertension, dyslipidemia or retinopathy were not collected. Therefore, this study has a limitation correlated to the co-existence of these key comorbidities in this study population. Additional limitations of our study include restricted generalizability because of the small sample size, which may not provide a generalized representation of the population of patients with T2DM in the Gulf countries. Additionally, possible selection bias may have existed, considering that the study was conducted in some but not all clinics in the region. However, the sample did include patients from two different Gulf countries, with evenly distributed patients across three different sectors: secondary care public hospitals, primary care public clinics and private clinics/hospitals. Furthermore, some information on diagnoses, laboratory measurements and prescriptions may have been missing from the patients’ charts.
Conclusion
Around half of the recruited T2DM patients did not have associated comorbidities. The most prevalent comorbidity observed among patients with T2DM was CKD, mainly in stage 2, whereas the prevalence of CHF, PAD and cerebrovascular diseases were low. Patients attending secondary care public hospitals had the highest proportion of CVD and CKD compared to those attending other types of clinics. Among the study population, the co-prevalence of CVD and CKD was determined to be the most common, followed by CAD and CKD. Furthermore, with increasing age, the number of comorbidities was found to increase significantly. The presence of CVD, CAD and PAD was significantly associated with a longer duration of T2DM.
Overall, metformin was the most frequently used anti-hyperglycemic agent, followed by DPP4 inhibitors.
References
International Diabetes Federation. IDF diabetes atlas, 7th edn. Brussels, Belgium: International Diabetes Federation; 2015.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016. https://doi.org/10.1161/CIR.0000000000000350.
American Heart Association. Cardiovascular disease & diabetes. http://www.heart.org/HEARTORG/Conditions/Diabetes/WhyDiabetesMatters/Cardiovascular-Disease-Diabetes_UCM_313865_Article.jsp/#.V-Vy5U3rvwo. Accessed Mar 2019 n.d.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28. https://doi.org/10.1056/NEJMoa1504720.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JFE, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22. https://doi.org/10.1056/NEJMoa1603827.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44. https://doi.org/10.1056/NEJMoa1607141.
American Diabetes Association. Standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S1-2. https://doi.org/10.2337/dc20-Sint.
Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Køber LV, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373:2247–57. https://doi.org/10.1056/NEJMoa1509225.
Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373:232–42. https://doi.org/10.1056/NEJMoa1501352.
Scirica BM, Braunwald E, Raz I, Cavender MA, Morrow DA, Jarolim P, et al. Heart failure, saxagliptin, and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial. Circulation. 2014;130:1579–88. https://doi.org/10.1161/CIRCULATIONAHA.114.010389.
Jelinek HF, Osman WM, Khandoker AH, Khalaf K, Lee S, Almahmeed W, et al. Clinical profiles, comorbidities and complications of type 2 diabetes mellitus in patients from United Arab Emirates. BMJ Open Diabetes Res Care. 2017;5:e000427. https://doi.org/10.1136/bmjdrc-2017-000427.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:1–19. https://doi.org/10.1186/s12933-018-0728-6.
Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32:1243–52. https://doi.org/10.1185/03007995.2016.1168291.
Channanath AM, Farran B, Behbehani K, Thanaraj TA. State of diabetes, hypertension, and comorbidity in Kuwait: showcasing the trends as seen in native versus expatriate populations. Diabetes Care. 2013;36:e75–e75. https://doi.org/10.2337/dc12-2451.
Nowakowska M, Zghebi SS, Ashcroft DM, Buchan I, Chew-Graham C, Holt T, et al. The comorbidity burden of type 2 diabetes mellitus: patterns, clusters and predictions from a large English primary care cohort. BMC Med. 2019;17:1–10. https://doi.org/10.1186/s12916-019-1373-y.
Attal S, Mahmoud MH, Aseel MT, Candra A, Amuna P, Elnagmi M, et al. Indicators of quality of clinical care for type 2 diabetes patients in primary health care centers in Qatar: a retrospective analysis. Int J Endocrinol. 2019. https://doi.org/10.1155/2019/3519093.
Bashier A, Bin Hussain A, Abdelgadir E, Alawadi F, Sabbour H, Chilton R. Consensus recommendations for management of patients with type 2 diabetes mellitus and cardiovascular diseases. Diabetol Metab Syndr. 2019;11:1–28. https://doi.org/10.1186/s13098-019-0476-0.
Ellahham S. Diabetes and its associated cardiovascular complications in the Arabian Gulf: challenges and opportunities. J Clin Exp Cardiol. 2020;11:1–5. https://doi.org/10.4172/2329-6607.1000650.
Acknowledgements
We thank the participants of the study.
We would also like to thank Dr. Zufana Nazir for conducting data entry as well as Dr. Dina Omar and Mohammed Jalali for data entry and study-related activities. We thank Nidhi Sharma for her hard work; she has worked closely on the study and was responsible for managing the clinical study at the hospital site since the site initiation till closure; she was also involved in all the activities. Once the eligible patients were enrolled, she conducted data entry, data query resolution, site organization and monitoring visits with the sponsor, in addition to coordinating with the local and central EC. With her help, we were able to complete our planned recruitment, despite the short allocated time. Additionally, we thank Paulette Wanis from the MSD Medical Affairs Department who supported the study execution in Kuwait.
Funding
This study was funded by and the protocol was developed by MSD IDEA Middle East. The publication and journal’s Rapid Service Fee were funded by MSD IDEA Middle East.
Medical Writing and Additional Assistance
Medical writing was provided by Shaymaa El Awady in Clinart MENA and funded by MSD IDEA Middle East, and statistical analysis services were provided by Clinart MENA and funded by MSD IDEA Middle East.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Compliance with Ethics Guidelines
The authors state that they have received approval from the following institutional review boards on the conduct of the study: Dubai Health Authority DSREC (Dubai Scientific Research Ethics Committee), UAE Ministry of Health & Prevention Research Ethics Committee, Dasman Diabetes Institute Kuwait Ethics Review Committee and Kuwait Ministry of Health Ethics Review Committee. The authors also confirm that their study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and that all subjects provided informed consent to participate in the study.
Disclosures
All authors, Ebaa Al-Ozairi, Mahir Jallo, Khadija Hafidh, Dalal Alhajeri, Tarek Ashour and Eissa Mahmoud, have nothing to disclose. Zeyad Abd Elaal and Maysoon Loulou are employees of MSD IDEA Middle East, a subsidiary of Merck & Co., Inc., Kenilworth, NJ.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al-Ozairi, E., Jallo, M.K., Hafidh, K. et al. Prevalence of Cardiovascular and Renal Co-morbidities in Patients with Type 2 Diabetes in the Gulf, a Cross-sectional Observational Study. Diabetes Ther 12, 1193–1207 (2021). https://doi.org/10.1007/s13300-021-01038-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01038-6