Abstract
Introduction
Although diabetes is associated with hypertension, whether high blood glucose levels promote hypertension remains controversial. In this study we compared the predictive power of fasting plasma glucose (FPG), 2-h postprandial blood glucose (2hPG), and glycated hemoglobin (HbA1c) for the development of hypertension.
Methods
This study was a substudy of the REACTION study, an ongoing longitudinal cohort study investigating the relationship of prediabetes and type 2 diabetes with the risk of cancer in an urban Northern Chinese population in Beijing. Logistic regression analysis was used to calculate odds ratios (ORs) after adjustment for risk factors for hypertension, including age, sex, body mass index, and triglycerides.
Results
Among the 3437 participants, 497 developed hypertension during the 4-year follow-up. The logistic regression analysis showed that elevated FPG and 2hPG levels (FPG: OR 1.529; 95% confidence interval [CI] 1.348–1.735; 2hPG: OR 1.144; 95% CI 1.100–1.191), but not HbA1c, were independent risk factors for the development of hypertension. In the highest quartile of FPG and 2hPG levels, the multivariable-corrected ORs were 2.115 (95% CI 1.612–2.777) and 2.346 (95% CI 1.787–3.080), respectively, compared with the lowest quartile. The adjusted models showed no significant correlations between quartile HbA1c levels and the development of hypertension.
Conclusion
Higher FPG and 2hPG levels, but not HbA1c levels, are independent risk factors for developing hypertension in an urban Northern Chinese population.
Trial Registration
ClinicalTrials.gov NCT01206869.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Hypertension and diabetes are two very common major diseases worldwide, which often coexist. Common mechanisms of pathogenesis play important roles in both diseases, including oxidative stress, obesity, and insulin resistance, with insulin resistance commonly present in prediabetes and diabetes. |
Fasting plasma glucose (FPG) and 2-h postprandial blood glucose (2hPG) levels are two glucose markers used to assess prediabetes and diabetes statuses. It is important to clarify the relationship between risk of hypertension (HTN) and blood glucose level, but the large number of studies performed to date have generated conflicting results. |
The aim of this study was to assess the association of FPG, 2hPG and glycated hemoglobin (HbA1c) levels with the development of HTN in a prediabetic population. |
What was learned from the study? |
Higher FPG and 2hPG levels, but not HbA1c level, are independent risk factors for HTN in an urban Northern Chinese population. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13664345.
Introduction
Hypertension (HTN) and diabetes are common chronic diseases worldwide, often coexisting [1,2,3]. The pathophysiological characteristics of HTN and diabetes are different, but they do share many common pathways, including oxidative stress, obesity, and insulin resistance [4, 5]. Among these characteristics, hyperinsulinemia is commonly observed in diabetes, and it promotes the development of HTN mainly through insulin resistance [6]. Insulin resistance is a significant determinant of the development and progression of diabetes and a major cause of morbidity and mortality [7].
Prediabetes refers to a condition in which the blood sugar level is higher than it should be but not high enough for a diagnosis of diabetes, i.e., borderline blood glucose levels; it is diagnosed before the overt development of diabetes itself [8]. A very close relationship has been demonstrated between prediabetes and insulin resistance [9]. Fasting plasma glucose (FPG), 2-h postprandial glucose (2hPG), and glycated hemoglobin A1c (HbA1c) levels are currently used to define prediabetes (i.e., impaired fasting glucose [IFG], impaired glucose tolerance [IGT], and HbA1c 5.7–6.4%) [8, 10]. FPG and 2hPG levels are two of the most common markers used to detect and assess prediabetes and diabetes status [11].
Since prediabetes is a risk factor for the development of diabetes and is associated with the occurrence of HTN, it is important to clarify whether prediabetes is an independent risk factor for HTN development. However, many of the studies that have been performed to date have generated conflicting results [12,13,14,15,16]. Therefore, the aim of this study was to assess the association of FPG, 2hPG, and HbA1c levels with HTN development in a prediabetic population.
Methods
Study Population
This study was performed as a substudy of the REACTION study, an ongoing longitudinal cohort study investigating the relationship of prediabetes and type 2 diabetes with risk of cancer in an urban Northern Chinese population. In 2011, the REACTION study included all permanent residents aged 40–85 years residing in three urban communities in Beijing (i.e., Jinding, Laoshan, and Gucheng). Those residents with good compliance to their treatment regimen and who volunteered to participate were selected as survey participants using the overall sampling approach. Residents with poor health, limited mobility, or poor compliance were excluded. In total, 10,216 residents were surveyed in 2011. The baseline data were collected, including general situation, past medical history, current medication situation, lifestyle, physical exercise, family history, and other basic information. The initial registration in the REACTION study was in 2011; the first follow-up was conducted in 2011–2012; and the second follow-up was conducted in 2015–2016.
The study protocol was approved by the Ethics Committee of the PLA General Hospital (#2011-14) and was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments. All participants in the study provided written informed consent. The REACTION trial is registered (ClinicalTrials.gov NCT01206869).
Clinical and Other Measurements
The two follow-up examinations included completing a standard questionnaire on demographic characteristics, physical examinations, and laboratory tests on biochemical parameters. The specific follow-up screening procedures included: (1) completion of detailed questionnaires, which assessed age, sex, menstruation, family history of diabetes, surgical history, and medication status; (2) physical examination, which assessed height, weight, waist circumference, hip circumference, neck circumference, blood pressure, body fat, and pulse wave velocity measurements; and (3) laboratory tests, such as routine blood tests, routine urine tests, FPG, HbA1c, oral glucose tolerance test (OGTT), and blood lipid levels. Height and weight were measured with participants wearing light clothing without shoes. Body mass index (BMI) was calculated by dividing weight by height squared (kg/m2). Blood pressure was measured on the left upper arm three times after a 5-min rest in the sitting position; the average value of the three measurements was recorded as the blood pressure value. HTN was defined as systolic blood pressure ≥ 140 mmHg and/or a diastolic blood pressure ≥ 90 mmHg at the time of visit, and/or a self-reported history of HTN, and/or current use of antihypertensive medications. Diabetes was defined as FPG levels ≥ 7.0 mmol/L (126 mg/dl) and/or OGTT 2-h blood glucose levels ≥ 11.1 mmol/L (200 mg/dl), and/or HbA1c ≥ 6.5%, self-reported history of diabetes, or FPG ≥ 126 mg/dl with insulin or oral hypoglycemic agents. Prediabetes was defined as FPG ≥ 5.6 (100 mg/dl) and < 7.0 mmol/L (126 mg/dl), and/or OGTT 2-h blood glucose ≥ 7.8 mmol/L (140 mg/dl) and < 11.1 mmol/L (200 mg/dl), and/or HbA1c ≥ 5.7 and < 6.5% [8].
Statistical Analysis
The continuous variables are presented as means ± standard deviations (SD), and the categorical variables are presented as numbers and percentages. Continuous variables were compared using the independent t test. Categorical variables were compared using the chi-square test. Associations between independent clinical variables were analyzed using univariable and multivariable logistic regression analyses. FPG, 2hPG, and HbA1c were analyzed as continuous variables. Baseline data were assessed using logistic regression analysis of increments or quartiles (Q), and the odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. To investigate the impact of factors affecting the association between glucose metabolic markers and HTN, we used models with the following adjustments: age and sex (model 1), model 1 + BMI (model 2), and model 2 + triglyceride levels (model 3). A multivariable model (model 4) included age, sex, BMI, triglyceride levels, diastolic blood pressure, high-density lipoprotein (HDL)-cholesterol, and total cholesterol (TC)/HDL. All statistical analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Results
The cohort in the REACTION study consisted of 10,216 participants, of whom 30.29% were men; all were initially recruited between 2011 and 2012. Of these 10,216 participants, 3437 had no HTN and diabetes at baseline and were followed in this substudy for 4 years (Fig. 1).
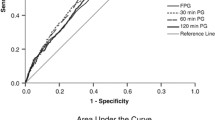
The mean (± SD) age of the participants was 54.70 ± 7.07 years (Table 1). Of the 3437 participants without HTN and diabetes at baseline, 497 (14.5%) developed HTN over the 4-year follow-up. The baseline characteristics of the study population are shown in Table 1. Among the study participants, 1434 (41.7%) had normal blood glucose levels and 2003 (58.3%) had prediabetes. Compared with the normal blood pressure group, the participants in the HTN group were older and had higher blood pressure, higher BMI, greater waist-to-hip ratio, higher waist-to-height ratio, higher triglycerides, higher FPG, higher 2hPG, higher HbA1c, and lower HDL-cholesterol levels. There were no clinically significant differences in TC and low-density lipoprotein-cholesterol levels between the two groups (Table 1). The ORs were calculated per SD increase in FPG, 2hPG, and HbA1c (Fig. 2) and were 1.529 (95% CI 1.348–1.735), 1.144 (95% CI 1.100–1.191), and 1.414 (95% CI 1.189–1.681), respectively, in the unadjusted model (Fig. 2). After adjustment for variables included in the multivariable models, FPG and 2hPG levels remained significant predictors of future HTN. HbA1c was only significantly correlated with future HTN in model 1, adjusted for age and sex; HbA1c levels had no predictive value for future HTN in the other models.
Odds ratios (OR) and 95% confidence intervals (CI) for the development of HTN at 5 years after baseline examination by increments of 1 SD for fasting blood glucose (FBG), 2-h postprandial blood glucose (PBG), and glycated hemoglobin (HbA1c) levels. Model 1: ORs were adjusted by age and sex. Model 2: ORs were adjusted by age, sex, and body mass index (BMI). Model 3: ORs were adjusted by age, sex, BMI, and triglycerides (TG). Model 4: ORs were adjusted by age, sex, BMI, TG, diastolic blood pressure, high-density lipoprotein (HDL), and total chloresterol/HDL
The OR values between quartiles of FPG, 2hPG, and HbA1c levels and the development of HTN are shown in Table 2. Compared with the lowest quartile (Q1) of FPG (Q1: FPG < 4.81 mmol/L), the OR for developing HTN was not significantly different in the second quartile (Q2: FPG 4.81–5.09 mmol/L), but it was significantly greater in the third (Q3: FPG 5.09–5.42 mmol/L; OR 1.338, 95% CI 1.002–1.787) and fourth (Q4: FPG ≥ 5.43 mmol/L; OR 2.115, 95% CI 1.612–2.777) quartiles in the unadjusted model. In models 1–4, only the highest quartile (Q4: FPG ≥ 5.43 mmol/L) predicted the development of HTN. Compared with the lowest quartile of 2hPG (Q1: 2hPG < 5.89 mmol/L) the OR for developing HTN was not significantly different in the second quartile (Q2: 5.89–6.91 mmol/L), but it was significantly greater in the third (Q3: 6.91–8.35 mmol/L; OR 1.365, 95% CI 1.020–1.828) and fourth (Q4: ≥ 8.35 mmol/L OR 2.346, 95% CI 1.787–3.080) quartiles. In the adjusted models, the fourth quartile in all models (1–4) and the third quartile (Q3: 6.91–8.35 mmol/l; OR 1.341, 95% CI 1.000–1.799) in model 1 predicted the development of HTN. In contrast, there were no significant increases in HbA1c or in the OR value for HTN in any of the models.
After 4 years of follow-up, the incidence of HTN in the overall study population was 14.5% in 2015, 12.6% in the normoglycemic group, and 15.8% in the prediabetes group. Compared with patients with normal blood glucose levels, the incidence of HTN in patients with prediabetes was significantly higher (P < 0.001) (Table 3). The overall prevalence of HTN among the IFG/IGT populations was 19.9%. The prevalences of HTN in the elevated HbA1c, IFG, IGT, and IFG + IGT groups were 10.3, 16.6, 20.6, and 23.3%, respectively. No significant differences were found among the IFG, IGT and IFG + IGT groups (all P > 0.05) (Table 4). However, comparison of patients with HbA1c ≥ 5.7% and those with HbA1c < 6.5% revealed that the prevalence of HTN in the IFG, IGT and IFG + IGT groups was significantly higher (P = 0.002, P < 0.001, P < 0.001), respectively. This result indicates that the risk of future HTN is significantly higher in the prediabetic population than in individuals with normal blood glucose levels. Moreover, a significant lower prevalence only was observed in patients with elevated HbA1c.
Discussion
In this longitudinal retrospective cohort study of urban Northern Chinese individuals without diabetes and HTN, there were significant positive correlations between the risk of HTN and the levels of FPG, 2hPG, and HbA1c. In the multivariable adjustment model, the association between HbA1c and the risk of HTN disappeared after the inclusion of BMI. In contrast, the relationships between FPG and 2hPG and the risk of HTN persisted in all adjusted models. These results strongly suggest that FPG and 2hPG levels are independent risk factors for HTN and that elevated levels of these parameters significantly increase the risk for developing HTN.
There is no agreement on which glucose indicator (i.e., FPG, 2hPG, or HbA1c) can best predict the risk of HTN. Similar to the present study, a previous study from Japan compared the correlation between FPG quartiles and the risk of HTN. Higher blood glucose levels were associated with an elevated risk of high blood pressure in healthy individuals, whereas normal range HbA1c was not [12]. Many studies have reported similar results, suggesting that FPG is an independent risk factor for future occurrence of HTN [13, 15, 17,18,19,20]. Nevertheless, some studies have shown conflicting results [21, 22]. IGT is another indicator of blood glucose used in the diagnosis of prediabetes. Both IFG and IGT may be related to insulin resistance [11]. IFG results in elevated hepatic glucose production in the fasting state, while IGT is caused by muscle insulin resistance [16]. Due to the complexity and cost of OGTT compared with FPG measurement, relatively few studies have investigated the relationship between postprandial blood glucose and HTN. In the AusDiab study. After adjustments for related multivariable factors, higher 2hPG levels during OGTT were associated with an elevated risk of HTN at 5 years [14]. Another study from Hong Kong and the STOP-NIDDM study showed that 2hPG or IGT was an independent predictor of new HTN [5, 23]. The association between IGT and HTN might be explained by the hypothesis that the two conditions share one or more pathogenic factors (i.e., insulin resistance or sympathetic nervous system hyperactivity), which induce the deterioration of blood pressure control, followed by hyperglycemia [24]. Still, in a Korean study, multiple logistic regression analyses demonstrated that both IFG and IGT had no predictive value for the occurrence of HTN [21, 25]. In this study, the participants in the fourth quartile of FPG and 2hPG had a significantly increased prevalence of HTN, suggesting that the risk of hypertension increases with an increase of FPG and 2hPG within normal ranges. Several previous studies have yielded conflicting results, with some studies finding no correlation between HbA1c levels and risk of HTN [12, 13, 26,27,28], while another study found an independent association between HbA1c level and the risk of HTN [29]. In the present study, the relationship between HbA1c level and HTN gradually disappeared after several adjustments, and there were no significant differences in the risk of HTN by HbA1c quartile, indicating that HbA1c does contribute to the elevated risk of HTN, but that it is not an independent risk factor for HTN and increased the risk of HTN when intermixed in a clade with age and obesity.
In the present study, we found that participants with prediabetes exhibited significantly higher levels of risk for HTN than those with normoglycemia. The risk of HTN was not significantly different among different types of prediabetic (IFG, IGT, and IFG + IGT) individuals other than elevated HbA1c.
Many studies have shown that a discordance between prediabetic or diabetic ranges of FPG, 2hPG, and HbA1c tests. It is well-known that FPG and HbA1c levels identify different pathological abnormalities in glucose metabolism. As HbA1c levels are influenced by the glycation of body proteins due to hyperglycemia, it has been suggested that glucose concentrations may more directly reflect the pathogenesis of HTN development compared to HbA1c, which is an indirect measure of dysglycemia. At the present time, diabetes is mainly diagnosed using FPG, 2hPG, and HbA1c levels [30]. HbA1c is an approximate measure of blood glucose control that reflects the average blood glucose level over the past 3 months; therefore, it does not correctly reflect extreme blood glucose values and blood glucose variability [10]. On the basis of FPG and 2hPG abnormalities, patients can be divided into the IFG and IGT groups. IFG is associated with hepatic insulin resistance, and IGT is caused by muscle insulin resistance [21]. In addition, in some diseases and conditions (e.g., sickle cell disease, pregnancy, glucose 6-phosphate dehydrogenase deficiency, hemodialysis, and recent blood loss or transfusion), the relationship between HbA1c and blood glucose is altered so that the true blood glucose level is not fully reflected [10]. Metabolic studies have shown that the relationship of HbA1c with insulin resistance and insulin secretion is weak compared to that of FPG and 2hPG with these parameters [31]. Increases in HbA1c are affected by protein glycosylation in vivo, which constitutes a secondary factor underlying high glucose levels. Thus, glucose levels might more directly reflect the pathogenesis of the development of HTN based on hyperinsulinemia and insulin resistance, compared to HbA1c [32].
Our study had some limitations. First, the study population included a cohort established using residents of several Beijing neighborhoods. Thus, the cohort may not be fully representative of all ethnic groups in North and South China. Second, the study did not assess the point of HTN development in patients with new HTN; notably, HTN was diagnosed based on the blood pressure measured on the day of the physical examination or using a self-reported history of HTN or history of antihypertensive medication use. Therefore, survival analysis could not be performed. Our study also had some important strengths. First, it included a large cohort of participants, comprising both men and women. Second, unlike most previous studies, this study performed a comprehensive assessment of the relationship between abnormal blood glucose metabolism and HTN using FPG and 2hPG, assessed with the OGTT. Third, the participants were divided into quartiles based on HbA1c levels, but each quartile covered a very narrow range of HbA1c values. It is not impossible that this design contributed to the lack of association between HbA1c quartiles and the development of HTN. Fourth, lifestyle habits (nutrition, physical activity, smoking, and alcohol use) and family history of hypertension that are closely related to the development of hypertension were not taken into account in the study.
Conclusions
In conclusion, higher FPG and 2hPG levels, but not HbA1c levels, were significantly independently correlated with the development of HTN in an urban Northern Chinese population. Our findings indicate that IFG and IGT are key predictors of HTN occurrence, and not the limited independent outcomes of abnormal HbA1c levels.
References
Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601–10. https://doi.org/10.1016/s0140-6736(12)60987-8.
Cheung BM, Li C. Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep. 2012;14(2):160–6. https://doi.org/10.1007/s11883-012-0227-2.
Sun D, Zhou T, Heianza Y, et al. Type 2 diabetes and hypertension. Circ Res. 2019;124(6):930–7. https://doi.org/10.1161/CIRCRESAHA.118.314487.
Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370(9587):591–603. https://doi.org/10.1016/s0140-6736(07)61299-9.
Cheung BM, Wat NM, Tso AW, et al. Association between raised blood pressure and dysglycemia in Hong Kong Chinese. Diabetes Care. 2008;31(9):1889–91. https://doi.org/10.2337/dc08-0405.
Soleimani M. Insulin resistance and hypertension: new insights. Kidney Int. 2015;87(3):497–9. https://doi.org/10.1038/ki.2014.392.
Stenvers DJ, Scheer F, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15(2):75–89. https://doi.org/10.1038/s41574-018-0122-1.
[No authors listed]. Introduction: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Suppl 1):S1–2. https://doi.org/10.2337/dc21-Sint.
van der Schaft N, Schoufour JD, Nano J, et al. Dietary antioxidant capacity and risk of type 2 diabetes mellitus, prediabetes and insulin resistance: the Rotterdam Study. Eur J Epidemiol. 2019;34(9):853–61. https://doi.org/10.1007/s10654-019-00548-9.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S13–28. https://doi.org/10.2337/dc19-S002.
Carnevale Schianca GP, Rossi A, Sainaghi PP, Maduli E, Bartoli E. The significance of impaired fasting glucose versus impaired glucose tolerance: importance of insulin secretion and resistance. Diabetes Care. 2003;26(5):1333–7. https://doi.org/10.2337/diacare.26.5.1333.
Heianza Y, Arase Y, Kodama S, et al. Fasting glucose and HbA1c levels as risk factors for the development of hypertension in Japanese individuals: toranomon hospital health management center study 16 (TOPICS 16). J Hum Hypertens. 2015;29(4):254–9. https://doi.org/10.1038/jhh.2014.77.
Kuwabara M, Chintaluru Y, Kanbay M, et al. Fasting blood glucose is predictive of hypertension in a general Japanese population. J Hypertens. 2019;37(1):167–74. https://doi.org/10.1097/HJH.0000000000001895.
Boyko EJ, Barr EL, Zimmet PZ, Shaw JE. Two-hour glucose predicts the development of hypertension over 5 years: the AusDiab study. J Hum Hypertens. 2008;22(3):168–76. https://doi.org/10.1038/sj.jhh.1002316.
Zhao Y, Sun H, Wang B, et al. Impaired fasting glucose predicts the development of hypertension over 6years in female adults: results from the rural Chinese cohort study. J Diabetes Complications. 2017;31(7):1090–5. https://doi.org/10.1016/j.jdiacomp.2017.04.006.
Abdul-Ghani MA, Sabbah M, Kher J, Minuchin O, Vardi P, Raz I. Different contributions of insulin resistance and beta-cell dysfunction in overweight Israeli Arabs with IFG and IGT. Diabetes Metab Res Rev. 2006;22(2):126–30. https://doi.org/10.1002/dmrr.595).
Yan Q, Sun D, Li X , et al. Association of blood glucose level and hypertension in Elderly Chinese Subjects: a community based study. BMC Endocr Disord. 2016;16(1):40. https://doi.org/10.1186/s12902-016-0119-5.
Zheng R, Mao Y. Triglyceride and glucose (TyG) index as a predictor of incident hypertension: a 9-year longitudinal population-based study. Lipids Health Dis. 2017;16(1):175. https://doi.org/10.1186/s12944-017-0562-y.
Suematsu C, Hayashi T, Fujii S, et al. Impaired fasting glucose and the risk of hypertension in Japanese men between the 1980s and the 1990s. The Osaka Health Survey. Diabetes Care. 1999;22(2):228–32. https://doi.org/10.2337/diacare.22.2.228.
Shi W, Zhou Y, Sun Y, Wang H. Could fasting blood glucose predict hypertension: findings from a low-resource community. J Hypertens. 2020;38(2):369–71. https://doi.org/10.1097/hjh.0000000000002305.
Lee CJ, Lim NK, Kim HC, et al. Impaired fasting glucose and impaired glucose tolerance do not predict hypertension: a community cohort study. Am J Hypertens. 2015;28(4):493–500. https://doi.org/10.1093/ajh/hpu186.
Wang W, Lee ET, Fabsitz RR, et al. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension. 2006;47(3):403–9. https://doi.org/10.1161/01.HYP.0000200710.29498.80.
Hanefeld M, Pistrosch F, Koehler C, Chiasson JL. Conversion of IGT to type 2 diabetes mellitus is associated with incident cases of hypertension: a post-hoc analysis of the STOP-NIDDM trial. J Hypertens. 2012;30(7):1440–3. https://doi.org/10.1097/HJH.0b013e328354663c.
Vaccaro O, Imperatore G, Iovino V, Iovine C, Rivellese AA, Riccardi G. Does impaired glucose tolerance predict hypertension? A prospective analysis. Diabetologia. 1996;39(1):70–6. https://doi.org/10.1007/bf00400415.
Tatsumi Y, Morimoto A, Asayama K, et al. Fasting blood glucose predicts incidence of hypertension independent of HbA1c levels and insulin resistance in middle-aged Japanese: the Saku Study. Am J Hypertens. 2019;32(12):1178–85. https://doi.org/10.1093/ajh/hpz123.
Geva M, Shlomai G, Berkovich A, et al. The association between fasting plasma glucose and glycated hemoglobin in the prediabetes range and future development of hypertension. Cardiovasc Diabetol. 2019;18(1):53. https://doi.org/10.1186/s12933-019-0859-4.
Britton KA, Pradhan AD, Gaziano JM, et al. Hemoglobin A1c, body mass index, and the risk of hypertension in women. Am J Hypertens. 2011;24(3):328–34. https://doi.org/10.1038/ajh.2010.233.
Jung JY, Oh CM, Choi JM, Ryoo JH, Park SK. Long-term risk of hypertension in normoglycemia and prediabetes, and their relation to the change of glycemic state. Am J Hypertens. 2018;31(9):1042–8. https://doi.org/10.1093/ajh/hpy094.
Au Yeung SL, Luo S, Schooling CM. The impact of glycated hemoglobin on risk of hypertension: a Mendelian randomization study using UK Biobank. J Hypertens. 2020;38(1):38–44. https://doi.org/10.1097/HJH.0000000000002210.
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–34. https://doi.org/10.2337/dc09-9033.
Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM. A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care. 2010;33(9):2104–9. https://doi.org/10.2337/dc10-0679.
Bonora E, Tuomilehto J. The pros and cons of diagnosing diabetes with A1C. Diabetes Care. 2011;34(Suppl 2):S184–90. https://doi.org/10.2337/dc11-s216.
Acknowledgements
We sincerely thank the participants of the study.
Funding
This work was supported by a grant from the National Science and Technology Major Project (2011ZX09307-001-08) for the REACTION study, the National Key R&D Program of China (2018YFC1314100). The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Yingkui Si, Anping Wang, Yunshuang Yang, Hongzhou Liu, Shi Gu, Zhaohui Lyu, and Yiming Mu have nothing to disclose.
Compliance with Ethics Guidelines
The study protocol was approved by the Ethics Committee of the PLA General Hospital (#2011-14) and was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments. All participants in the study provided written informed consent. The REACTION trial is registered (ClinicalTrials.gov NCT01206869).
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Si, Y., Wang, A., Yang, Y. et al. Fasting Blood Glucose and 2-h Postprandial Blood Glucose Predict Hypertension: A Report from the REACTION Study. Diabetes Ther 12, 1117–1128 (2021). https://doi.org/10.1007/s13300-021-01019-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01019-9