Abstract
Introduction
Recent guidelines for the treatment of type 2 diabetes mellitus (T2DM) provide evidence supporting limited use of sulphonylureas (SUs), especially in specific risk patient categories, yet data from national registries still suggest their widespread use. The aim of this study was to investigate characteristics of patients with diabetes treated with SUs and quantify the proportion of patients that met the recommendations for use of SUs by recent guidelines and of those presenting characteristics representing an inappropriate prescription risk (IPR).
Methods
A multicenter, retrospective, cross-sectional, observational study in patients with T2DM receiving treatment with SUs (as monotherapy or in combination with another diabetes therapy) was conducted between 2017 and 2018 in 22 outpatient diabetes clinics across Italy. Exclusion criteria were type 1 diabetes, diabetes mellitus secondary to other conditions, and presence of severe/life-threatening diseases.
Results
A total of 510 patients with T2DM (306 men, 204 women; mean age ± standard deviation 69.8 ± 9.3 years) who were receiving treatment with a SU (as monotherapy or in combination therapy) were assessed in the study. Overall, 70.6% [n = 360; 95% confidence interval (CI) 66.4%, 74.5%] were assessed to have an IPR. Of these, approximately half presented one factor for risk of inappropriate prescription, and 27 and 10.6% presented two and three factors, respectively. In terms of factors contributing to the total burden of risk of inappropriate treatment with SUs, 37.5% (95% CI 33.2%, 41.8%) of all patients were obese; 33.3% (95% CI 29.3%, 37.6%)] were aged ≥ 75 years; 18.6% (95% CI 15.3%, 22.3%) had a history of cardiovascular disease; 14.1% (95% CI 11.2%, 17.4%) had chronic renal insufficiency; 1.8% (95% CI 0.8%, 3.3%) had a history of severe hypoglycemia; 1.8% (95% CI 0.8%; 3.3%) had cognitive impairment; and 2.4% (95% CI 1.2%, 4.1%) had a risky occupation.
Conclusions
The results of this study provide evidence of a high rate of inappropriate SU prescription risk among patients with T2DM, especially among those with overweight/obesity, older age, history of cardiovascular disease, and hypoglycemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
National guidelines recommend limiting the use of sulphonylureas (SUs) in patients with type 2 diabetes mellitus, especially in those with history of heart disease, renal failure, and history of hypoglycemic events. |
The aim of this study was to investigate characteristics of diabetic patients treated with SUs and quantify the proportion of patients that met the recommendations for use of SUs in recent guidelines and of those presenting characteristics representing inappropriate prescription risk (IPR). |
Data from the SUSCIPE study, conducted in 22 outpatient diabetes clinics across Italy, were collected from more than 500 patients with T2D. |
What was learned from this study? |
The results showed that in 70% of cases SUs were prescribed to patients who according to guidelines belong to specific patient groups for whom guidelines recommend caution. |
Approximately half of these patients had one risk factor for whom a prescription might be considered inadequate, and 27 and 10.6% had two and three factors, respectively. |
SUs are still widely prescribed despite the availability of alternative drugs without any intrinsic risk of hypoglycemia or weight gain, with up to half of patients on SUs in our population receiving a new prescription with a SU within the last 2 years of the study. |
Introduction
To date, despite the availability of several molecules and drug classes for the treatment of type 2 diabetes mellitus (T2DM), a large portion of patients still do not achieve optimal glycemic control and are therefore exposed to a higher long-term risk for microvascular damage and systemic complications [1,2,3]. As evidenced by the results of the UK Prospective Diabetes Study (UKPDS), a 1% reduction in glycated hemoglobin (HbA1c) appears be associated with marked reductions in diabetes-related mortality (21%), myocardial infarction (14%), and microvascular complications (37%) [2, 3]. Accordingly, recent guidelines (GLs) developed for the treatment of T2DM in Western countries have been reconsidering therapies and treatment targets, with the aims of shifting HbA1c values downards, from 7 to < 6.5% (53–48 mmol/mol), without placing the patient at risk of severe hypoglycemia or any other side effects [1, 3,4,5,6] and of broadening the scope of the recommendations from HbA1c reduction alone to include changes in lifestyle, weight stabilization/reduction, and prevention of metabolic complications [1, 3, 4].
Current recommendations for antihyperglycemic treatment stress that the choice of therapy must be oriented towards molecules that are weight-neutral [dipeptidyl peptidase-4 (DPP-4) inhibitors] or promote weight loss (metformin, glucagon-like peptide-1 receptor agonists (GLP-1 RAs), and sodium-glucose transport protein 2 (SGLT2) inhibitors], void of an increased risk of hypoglycemia [associated mostly to the use of insulin or sulphonylureas (SUs)/glinides] [1, 3], and without increased comorbidity for cardiovascular (CV) disease or kidney failure. Not least, treatment aspects have also been discussed in terms of relevant economic-related implications, with higher costs being offset by the prevention of hypoglycemic events and reduction in hospital admissions [7].
In 2016 these principles were embraced by the national GLs of Italy [3], which also underlined the lack of evidence for the superiority of one agent over another (except for metformin in overweight patients with diabetes). Although the GLs did not endorse the use of any one specific agent, they did provide guidance on major (hypoglycemia, kidney disease, heart disease, risky occupation) and minor (age, obesity) factors that should caution against the use of a specific agent [1, 3, 8]. Specific warnings included the use of SUs in the elderly and in patients with renal failure and/or a history of hypoglycemic events, based on the glucose-independent manner with which these drugs stimulate insulin secretion.
Since then, such concerns have been addressed further with contrasting results from a number of studies on the possible contribution of SUs to CV disease [8,9,10]. Although very recent studies [11, 12] seem to provide ultimate evidence of the neutrality of SUs in promoting CV disease, this is not so for patients who have already had a CV event and who should be directed to newer generation molecules, such as SGLT2 inhibitors or GLP-1 RAs, that have been shown to even reduce CV risk [4]. Nonetheless, 2016 data from national registries [13, 14] indicate that approximately 36.3% of all oral antihyperglycemic agents prescribed in Italy are secretagogues, specifically SUs/SU + metformin (27.4%) and glinides (8.9%).
Taking these data into consideration, we have investigated the socio-demographic and clinical characteristics of patients with diabetes treated with SUs. In addition, we have assessed whether—and if so, in what proportion—these patients met the recommendations in recent Italian and international GLs for the use of SUs in clinical practice and quantified the inappropriate prescription risk (IPR).
Methods
Study Design and Population
This study was a multicenter, retrospective/cross-sectional, observational study involving 22 outpatient diabetes clinics across Italy that were chosen to provide a heterogeneous representation of large- and medium-sized referral centers (on average, with 1 diabetologist and 2 nurses per 1000 patients) located in the northern, central, and southern regions of Italy.
Patient enrollment took place between June 2017 and July 2018, and all consecutive patients receiving SU treatment who presented for their prescheduled periodic check-up appointment (index visit) during that period were eligible. No additional appointments were scheduled for this study, and no pharmacological or behavioral interventions were implemented for the purpose of this study. During the index visit, relevant information was collected as required by the protocol, either on paper or on an electronic case report form, in accordance with each participating center’s procedures.
Criteria for inclusion in the study were: diagnosis of T2DM [as defined by the American Diabetes Association (ADA) criteria]; on-going treatment with SUs, either as monotherapy or in combination therapy; availability of complete socio-demographic and clinical data relevant to the purpose of the study; and signed patient-informed consent form. Exclusion criteria were: type 1 diabetes mellitus; non-pharmacologically treated diabetes; T2DM treated only with medications other than SUs; diabetes mellitus secondary to other conditions; and other severe life-threatening diseases.
Among the main data collected were socio-demographic variables and main clinical and diabetes-related laboratory parameters [family history of diabetes, concomitant diseases and treatments, history of CV disease, history of hypoglycemia events, body mass index (BMI), blood pressure, HbA1c, kidney function, type of SU, and initiation date of SU therapy].
Study Objectives
The primary objective of the study was to quantify the percentage of patients inappropriately treated with SUs, based on the 2016 Associazione Medici Diabetologi–Società Italiana di Diabetologia (AMD–SID) GLs [3]. Specifically, inappropriate treatment was defined as patients meeting one or more of the following seven characteristics/risk factors: age ≥ 75 years; history of heart failure, unstable angina, coronary heart disease, stroke, or myocardial infarction; chronic renal insufficiency (moderate to severe or requiring dialysis); history of severe hypoglycemia (conventionally defined as an episode that requires assistance from another person); obesity (set as BMI ≥ 30 kg/m2, in accordance with the AMD–SID and World Health Organization definitions); cognitive impairment; and risky occupation (bus/taxi/train driver, working at height).
The secondary objective was to quantify the percentage of patient subgroups by specific comorbidity, age, or one of the seven characteristics mentioned above, and the use of glibenclamide, gliclazide, or repaglinide + SU among patients aged ≥ 75 years. In addition, and with an exploratory purpose only, a further aim was to examine the association between selected individual characteristics and drug use and IPR.
Statistical Methods
Regarding the primary objective, the IPR of SUs was calculated as the percentage ratio between the number of patients meeting one or more of the seven characteristics/risk factors outlined in the 2016 AMD–SID GLs and the number of eligible patients (all treated with SUs). For the secondary objective, we calculated the percentages of patients contributing to the total burden of inappropriate treatment with SUs for each specific factor together with their Clopper–Pearson 95% confidence interval (CI). In addition, the percentages of patients treated with the SUs glibenclamide or gliclazide or with repaglinide (a meglitinide) + SU and aged ≥ 75 years were calculated.
An exploratory analysis was conducted by comparing groups of patients with inappropriate versus appropriate treatment with SUs according to selected characteristics using Pearson’s chi-squared test or Fisher’s exact test (for categorical variables) and the Mann–Whitney test for HbA1c. For all statistical tests, a p value < 0.05 was accepted as indicating statistical significance. Secondly, the evaluation of the candidate predictors of IPR was examined using multiple logistic regression analysis to compute the odds ratios (OR) and related 95% CIs [15]. Models with different sets of independent variables were estimated on patients for whom data on all relevant variables were available.
Analysis of the primary objective was also repeated by eliminating BMI from the risk factors in the IPR definition.
Compliance with Ethics Guidelines
The present study was approved (no. 80/2017/U) by the Ethics Committee "Comitato Etico interaziendale AOU San Luigi Gonzaga di Orbassano AA.SS.LL. TO3–TO4–TO5" (Turin, Italy). Given the retrospective design of the study, no medical, pharmacological, or behavioral interventions were involved. All research was conducted in agreement with the principles laid out in the original Declaration of Helsinki and its later amendments, and data were handled in agreement with patient-informed consent.
Results
The study included a total of 510 adult patients with T2DM [306 men/204 women; 97.8% Caucasian; mean age (± standard deviation) 69.8 ± 9.3 years], all of whom were receiving treatment with a SU, either as monotherapy or in combination with another diabetes medication (Table 1). The mean BMI was 29.1 ± 5.2 kg/m2, with the majority of patients (81.0%) being either overweight or obese (43.5 and 37.5%, respectively). Mean HbA1c was 7.6 ± 1.3% (60 ± 14.2 mmol/mol), and approximately one-half of the patients enrolled had a family history of diabetes. One-third of all patients (95% CI 29.3%, 37.6%) were aged ≥ 75 years, 18.6% (95% CI 15.3%, 22.3%) had a history of CV disease, 14.1% (95% CI 11.2%, 17.4%) had chronic renal insufficiency, 1.8% (95% CI 0.8%, 3.3%) had a history of severe hypoglycaemia events, 1.8% (95% CI 0.8%, 3.3%) had cognitive impairment, and 2.4% (95% CI 1.2%, 4.1%) had a risky occupation.
Rate of IPR
Based on the seven main criteria from the 2016 AMD–SID GLs [3] used to identify the inappropriate use of SUs, of the 510 adult patients included in the study, 360 (70.6%; 95% CI 66.4%, 74.5%) were classified as presenting with an IPR. Of these 360 patients, 60.3% presented with only one risk factor.
Analysis of the IPR (Table 2) revealed that the most common risk factors were obesity (47.5% of patients with IPR), age > 75 years (32.3%), and CV comorbidity (10.6%). Of the 360 patients with an IRP, more than one-half had ≥ 2 concomitant risk factors, with 27% presenting with two risk factors, of which the most common were the combinations obesity + age (26.8% of the latter patient group), age + CV morbidity (20.6%), obesity + CV comorbidity (14.4%), and age + renal disease (14.4%); 10.6, 1.9, and 0.3% of patients presented with three, four, and five concomitant risk factors, respectively.
The computation of the IPR after BMI was removed from the analysis of risk factors (this parameter is a possible source of bias) confirmed that one-half of all SU prescriptions were inappropriate, yielding a 50.4% IPR (95% CI 46.0%, 54.8%) (Supplementary material Table 1 Appendix).
The association between selected features and IPR (Supplementary material Table 2 Appendix) was statistically significant for the following variables: use of antihypertensive agents (p < 0.001), use of anticoagulant agents (p = 0.010), use of antithrombotic agents (p = 0.002), use of other agents for the CV system (p = 0.019), and use of at least one agent among antihypertensive, lipid-lowering, and antithrombotic agents (p = 0.004). The association of use of lipid-lowering agents and IPR was not statistically significant (p = 0.153).
Multiple regression logistic models used to assess the predictors of IPR (Supplementary material Table 3 Appendix) showed that the propensity of IPR was about twofold higher for patients receiving antihypertensive drugs (OR 1.88; 95% CI 1.18, 3.00) and for those taking at least one agent among the antihypertensive, lipid-lowering, and antithrombotic agents (OR 1.98; 95% CI 1.10, 3.56). Conversely, the analysis did not show a statistically significant difference between appropriately and inappropriately treated patients in terms of use of lipid-lowering agents (OR 1.16; 95% CI 0.78, 1.75).
SU Types, Doses, and Length of Treatment
The most commonly used SU among the 510 patients was gliclazide (71.4%), followed by glimepiride (20.6%) (Table 3). Among the patients aged > 75 years (33.3% of total patients enrolled), gliclazide was used by 68.2%, glibenclamide (with or without metformin) by 11.8%, and SU + repaglinide by 4.1%.
Data obtained in the IPR (n = 360) population stratified by length of treatment since prescription (Table 4) showed that one-half of inappropriate treatments were started within the 2-year period preceding the index visit, while the other half referred to older prescriptions (31.1% of SUs prescribed during the previous 3–9 years; 10.8% during the previous 10–14 years, and 8.3% over 15 years previously). Among the patients appropriately treated (150 non-IRP patients), slightly more than one-half had had treatments started within the last 2 years.
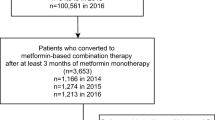
Gliclazide was the most commonly SU prescribed in all time frames considered (0–2 years, 3–9 years, 10–14 years, ≥ 15 years) (Fig. 1), followed by glimepiride, either alone or in combination with metformin. Compared to when the overall time frame was considered, the analysis of length of treatment showed that the use of gliclazide increased in the most recent 2-year period from the index visit, whereas the use of glimepiride increased in the 3- to 9-year time frames; Also, the prescription rate showed a 50% reduction in the most recent 2 years.
The mean daily dose of insulin used in 69 patients was 16.8 ± 11.6 U. The median daily doses of the SUs were 60.0 (mean ± SD, 57.7 ± 36.4) for gliclazide, 2.0 (mean ± SD, 4.9 ± 16.8) for glimepiride and 5.0 (mean ± SD, 8.6 ± 5.8) for glibenclamide.
Discussion
The aim of the study reported here was to provide a snapshot of current utilization of SUs in Italy, focusing on the rate of inappropriate prescription, as defined by the presence of at least one of seven main patient characteristics/risk factors mentioned in current guidelines. Overall, the patient sample represented a typical patient population with T2DM, with most patients presenting high HbA1c values, overweight or obesity, and several comorbidities.
With specific reference to the primary objective of our study, 70.6% of the patients had at least one IPR (n = 360), of whom 50% presented one risk factor for IPR and the remaining 50% presented ≥ 2 risk factors. Weight, age, and CV comorbidities were the most frequently documented patient risk factors. Many patients presented several risk factors concomitantly, which worsened the cumulative individual risk of an inappropriate prescription.
Overall, our analyses confirmed the potentially inappropriate use of SUs, with 50% of all SU prescriptions occurring within the 2 years immediately preceding the index visit. It is noteworthy, however, that during the study period (June 2017 to July 2018) the use of SUs was already being discouraged, in part in accordance with the 2016 AMD–SID GLs for specific patient risk categories, such as those considered in this study, and in part due the availability of alternative drugs with a very low risk of hypoglycemia and weight gain, such as DPP-4 inhibitors, GLP-1 RAs and, more recently, SGLT2 inhibitors. In addition, the 2018 AMD-SID GLs no longer recommend SUs as second-line treatment (scientific evidence grade I A), limiting their use only to special cases as third-line treatment and not in combination with insulin [4], while specifically recommending against the use of glibenclamide, which is associated to a greater risk of hypoglycemia [3, 4].
BMI and Overweight/Obesity
We had expected weight to be an important discriminating factor in the choice of anti-diabetes treatment as it significantly influences glycemic control and macrovascular complications. It is also well known that overweight and obese patients are more likely to be affected by T2DM, with the odds ratio increasing from the lowest BMI category to the highest [1, 4, 16,17,18,19].
In our study we set the cutoff for obesity at BMI > 30 kg/m2 (rather than 25 kg/m2 as indicated by some GLs), as the cutoff reflects real-world clinical practice [3, 20].
Although we can only speculate on the reasons justifying the use of SUs in obese patients, treatment with SUs is associated with weight gain, which is known to enhance chronic low-grade subclinical inflammation and insulin resistance, contributing to the long-term development of macro- and microvascular damage [17, 21].
Age
Of all patients receiving SUs in the present study, 33% were older than 75 years; of these, 11.8% were treated with glibenclamide (with or without metformin), 68.2% were treated with gliclazide, and 4.1% were treated with a SU + repaglinide. These percentages are in agreement with data from an Italian national registry, Osservatorio ARNO, which also documents a high SU prescription rate among the elderly [14]. This high use of SUs is not recommended in current GL recommendations which, in contrast, discourage the use of SUs in elderly patients due to the increased risk of severe hypoglycemic events among aging patients who are already facing a physiological decrease in renal, hepatic, and beta-cell function [3, 4]. In particular, it is important to note that glibenclamide has a prolonged plasma half-life and that it lasts even longer in individuals suffering from renal impairment, which is frequently observed in elderly patients. Thus, the related high risk of hypoglycemia should always be considered when prescribing a new antihyperglycemic agent in older patients.
Hypoglycemia
With particular reference to hypoglycemia, the glycemic threshold that triggers symptoms of hypoglycemia is less functional in elderly individuals than in younger patients; consequently, the occurrence of a glycemic event may more easily lead to arrhythmias, angina, and falls in elderly patients. In particular, severe hypoglycemic episodes have been shown to be associated to a twofold increase in the incidence of dementia, as shown by recent systematic reviews and a meta-analysis of the impact of pharmacologic therapy for diabetes on dementia [22].
It has also been estimated that the risk of severe fatal events in the elderly doubles in patients receiving anti-diabetic treatment, either alone or with concomitant medications, as it increases the risk of hypoglycemia [3, 4]. Moreover, higher hypoglycemic risk has been well documented for some SUs, such as long-acting glibenclamide, which is also not recommended in recent GLs [3, 4]. Despite this, over 11% of our patients who were more than 75 years old were receiving treatment with glibenclamide.
Cardiovascular Risk
The CV risk factor for inappropriate prescription was found in 18.6% of the total patient population. In recent years the safety of SUs versus CV risk has been widely debated, and current GLs recommend the use of the new drug classes of SGLT-2 inhibitors and GLP-1 RAs, which have demonstrated a protective effect on CV mortality and events in individuals with history of heart disease [4, 23,24,25,26,27].
As demonstrated by current AMD–SID GLs, evidence for at least limiting the use of SUs appears to be sufficiently robust [1, 4, 28], yet still leaving room for debate on CV risk [AMD-SID2018]: data from the UKPDS trial showed a similar CV mortality among SU users and controls, and an even lower mortality for long-term SU users; the data also showed no significant difference between SU and insulin with respect to CV mortality. However, SUs are associated with a higher mortality than metformin [2]. The TOSCA.IT study compared SUs with pioglitazone and found no significant difference in the incidence of CV events, while a post-hoc analysis showed an inferior incidence of events for pioglitazone [7]. In contrast, several meta-analyses have reported conflicting results, with an increased all-cause mortality among patients on SUs, even if no statistically significant differences were found when data from more restrictive studies were analyzed [4].
In a population-based cohort study, 25,699 patients starting on metformin, either with SUs added to metformin or who were switched to SUs, were compared with patients remaining on metformin monotherapy. The authors reported that SUs as second-line drugs were associated with an increased risk of myocardial infarction, all-cause mortality, and severe hypoglycemia [29]. Such results are in disagreement with those of a previous 2013 Cochrane review that compared monotherapy with SUs versus placebo, no intervention, or other anti-diabetic interventions, and evaluated 72 randomized controlled trials with 22,589 participants. Results in a random-effects model showed no statistically significant effects of SUs regarding all-cause mortality or cardiovascular mortality [30].
Finally, results of trials with second-generation SUs did not show an increased CV risk with use of these agents. In fact, in the ADVANCE trial, in which participants in the intensive glycemic control group used a gliclazide-based regimen, CV outcomes were similar in the conventional and intensive arms [8]. Moreover, the recently concluded CAROLINA study, which is the first CV outcomes trial to compare two active drugs (linagliptin vs. glimepiride), appears to provide final evidence of the neutral CV profile of glimepiride [11].
Similarly, recent ADA standards of medical care [1, 31] consider second-generation SUs to be neutral on CV events (both atherosclerotic CV disease and heart failure), suggesting their use (as second-line treatment after metformin) in patients without established atherosclerotic CV disease or chronic kidney disease when cost is a major issue. However, this is not the case of Italy, where the National Health System reimburses the new classes of drugs, albeit with some prescription limitations. The ADA 2019 addendum to the 2018 GLs, however, does specifically recommend either GLP-1 RAs or SGLT2 inhibitors for patients with atherosclerotic CV disease or at high risk for heart failure, or SGLT2 inhibitors for patients with existing heart failure [1, 32].
Taking into account the number of patients in our population presenting the CV risk factor concomitantly with an age ≥ 75 years as well as additional risk factors, the study by Li et al. is worth mentioning. These authors specifically evaluated the use of SUs among the elderly and confirmed the association between CV disease and SUs in older individuals, with a positive correlation for coronary heart disease and duration of treatment, albeit with differing effect sizes depending on tissue-specific receptor binding of each SU [32].
Renal Impairment
In addition to CV disease, microangiopathic complications, such as reduced glomerular filtration rate (GFR) and microalbuminuria, represent additional sources of concern [3, 33, 34]. In the present study, approximately 13–14% of patients presented mild to moderate renal impairment, often in combination with another risk factor (age or weight). Reduced estimated GRF causes a prolonged presence and increased levels of the drugs and may therefore increase the risk of hypoglycemia.
SUs Amid Newer Generation Antihyperglycemic Treatment Options
Taken together the results from our study suggest the need to look deeper into the motivations underlying SU prescribing, particularly at a time when a number of alternative anti-diabetic treatments are available with equivalent effectiveness. With specific reference to the persistent usage of SUs in Italy, one explanation is likely related to the Italian Drug Regulatory Agency (Agenzia Italiana del Farmaco -AIFA) rules, which govern the use of innovative anti-diabetic drugs. These require diabetologists to first establish a personal therapeutic plan in which they prescribe either a GLP-1 RA, DPP-4 inhibitor, or SGLT2 inhibitor and then keep within that plan without the possibility to add other drugs for combination therapy, with the aim to stay within a certain cost range [35]. Other reasons for persistent usage could also be factors such as therapeutic inertia, incomplete consideration by the physicians of the risk factors described above, and the unwillingness of the patients to change drug or to accept more complex drug regimens.
It should be noted that the main SU prescribed in Italy is gliclazide, which is known to have a more favorable CV profile and a lower hypoglycemic risk than other SUs due to its pharmacodynamic and pharmacokinetic characteristics [36, 37]. Furthermore, the median drug dosage is in the low range.
One alarming development is the concomitant prescription of a SU with repaglinide. While SUs may be considered for use in combination with all classes of oral anti-diabetic drugs, they should not be administered with glinides.
In contrast with indications from the European GLs, several authors still support the use of SUs [38, 39], either focusing on the aspect of dosage that would appear to provide equal efficacy of other anti-diabetic agents with less adverse effects [36, 37] or on the modified or slow-release SUs (such as gliclazide) that are associated with a lower risk of hypoglycemia (especially compared to glimepiride or glipizide) [9, 38]. The debate on SUs has recently focused on the strength of scientific evidence of GLs versus consensus statements [40]. The affordability of SUs and disease-management costs aspects also remain relevant topics [1, 41,42,43].
Limits of the Study
Findings from our study provide evidence for a persistent high rate of inappropriate prescription of SUs in the last 2 years, in agreement with data from main national registries.
There are a number of limitations to our study. First, the sample size of our population was relatively small to draw definitive conclusions. Nevertheless, our study represents a “real-world” reflection of the activity of some outpatient clinics in a specific setting (Italy) in which the National Health Service provides drugs at no expense to diabetic patients, but where the prescription of innovative drugs is only possible under defined and restrictive rules. Second, the study does not include qualitative information on clinical decision-making that may have warranted appropriate SU use in these patients (possible contraindications to other glucose-lowering agents, patient preference, etc.). This might be an interesting aspect for future study.
Conclusions
Findings from this present study provide evidence for a high risk of inappropriate prescription of SUs among T2DM patients with established CV disease, older age, renal impairment, as well as high BMI indicative of obesity. These results underline the need for both general practitioners and specialists to carefully monitor patients for the presence of these factors and to withdraw or avoid prescribing this class of drug when one or more of these factors are present.
Larger and more prolonged observations are required to provide a better understanding of the evolution of anti-diabetic treatments in the era of innovative medications with proven effects on weight reduction, with a virtually absent risk of hypoglycemia, a minimal burden (or potential benefit) on diabetic renal disease, and proven beneficial effects on major CV outcomes.
References
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–701.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;1998(352):837–53.
Associazione Medici Diabetologi–Società Italiana di Diabetologia (AMD-SID). Standard italiani per la cura del diabete mellito 2016 [Italian standards for treatment of diabetes mellitus" 2016]. www.standarditaliani.it. Accessed May 2019.
International Diabetes Foundation (IDF). IDF clinical practice recommendations for managing type 2 diabetes in primary care. https://www.idf.org/our-activities/care-prevention/type-2-diabetes.html. Accessed 20 Oct 2019.
Associazione Medici Diabetologi–Società Italiana di Diabetologia (AMD-SID). Standard italiani per la cura del diabete mellito 2016 [Italian standards for treatment of diabetes mellitus" 2018]. www.standarditaliani.it. Accessed 2 May 2019.
AACE/ACE comprehensive 2019 type 2 diabetes management algorithm. https://www.aace.com/disease-state-resources/diabetes/clinical-practice-guidelines-treatment-algorithms/comprehensive. Accessed 20 Oct 2019.
Wang C, Neil D, Home P. Vision an overview of prospects for diabetes—management and prevention in the next decade. Diabetes Res Clin PR. 2020. https://doi.org/10.1016/j.diabres.2018.06.007.
Packer M. Are physicians neglecting the risk of heart failure in diabetic patients who are receiving sulfonylureas? Lessons from the TOSCA.IT trial. Eur J Heart Fail. 2018;20:49–55.
Heller S, ADVANCE Collaborative Group. A summary of the ADVANCE. Diabetes Care. 2009;32(Suppl 2):S357–S361361.
Alzaid A. Sulfonylureas in the treatment of type 2 diabetes mellitus: a fresh look and new insights. Diabetes Ther. 2020;11(Suppl 1):1–3.
Vaccaro O, Masulli M, Bonora E, et al. The TOSCAIT trial: a study designed to evaluate the effect of pioglitazone versus sulfonylureas on cardiovascular disease in type 2 diabetes. Diabetes Care. 2012;35(12):e82–e92.
Rosenstock J, Kahn SE, Johansen OE, et al. Effect of Linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: the CAROLINA randomized clinical trial. JAMA. 2019;322(12):1155–66. https://doi.org/10.1001/jama.2019.13772.
Osservatorio ARNO Diabete. II profilo assistenziale della popolazione con diabete. Rapporti Arno 2017 [Diabetes Healthcare Management]. http://www.siditalia.it/clinica/linee-guida-societari?limit=10&start=10 [document in Italian]. Accessed 13 July 2020.
Osservatorio ARNO Diabete. II profilo assistenziale della popolazione con diabete. Rapporti Arno 2019 [Diabetes Healthcare Management]. http://www.siditalia.it/clinica/linee-guida-societari [document in Italian]. Accessed 13 July 2020.
Hosmer DW, Lemeshow S. Applied logistic regression. New York: Wiley; 1989.
Ganz M, Sintfel L, Li Q, et al. The association of body mass index with the risk of type 2 diabetes: a case–control study nested in an electronic health records system in the United States. Diabetol Metab Syndr. 2014;6:50.
Argawal NK, Kant S. Targeting inflammation in diabetes: newer therapeutic options. World J Diabetes. 2014;5(5):697–710.
Dennis J, Shields BM, Henley WE, et al. Disease progression and treatment response in data-driven subgroups of type 2 diabetes compared with models based on simple clinical features: an analysis using clinical trial data. Lancet Diabetes Endocrinol. 2019;7(6):442–51.
Qian D, Zhang T, Tan X, et al. Comparison of antidiabetic drugs added to sulfonylurea monotherapy in patients with type 2 diabetes mellitus: a network meta-analysis. PLoS ONE. 2018;13(8):e0202563.
Berrington de Gonzalez B, Hartge P, Cerhan JR, et al. Body-mass index and mortality prospective analysis of 1.46 million white adults. N Engl J Med. 2010;362:2311.
Kothari V, Galdo A, Mathews S. Hypoglycemic agents and potential anti-inflammatory activity. J Inflam Res. 2016;9:27–38.
McMillan JM, Mele BS, Hogan DB, et al. Impact of pharmacological treatment of diabetes mellitus on dementia risk: systematic review and meta-analysis. BMJ Open Diabetes Res Care. 2018;6:e000563. https://doi.org/10.1136/bmjdrc-2018-000563.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–288.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:2099.
Marso SP, Daniela GH, Brown-Frandensen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;2016(376):891–2.
Holman R, Bethel A, Mentz R. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377:1228–399. https://doi.org/10.1056/NEJMoa1612917.
Shimoda M, Kaku K. Controversy about the relationship between sulfonylurea use and cardiovascular events and mortality. J Diabetes Investig. 2016;7(5):674–6.
Dourso A, D’Aniello S, Yun YuO, et al. Sulfonylureas as second line drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: population-based cohort study. BMJ. 2018;362:k2693.
Hemmingsen B, Schroll JB, Lund SS, et al. Sulphonylurea monotherapy for patients with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;(4):CD009008. https://doi.org/10.1002/14651858.CD009008.pub2.
American Diabetes Association. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes. Diabetes Care. 2019;42(Suppl 1):S90–S102.
Li Y, Hu Y, Ley SH, et al. Sulfonoylurea use and incident cardiovascular disease among patients with type 2 diabetes: prospective cohort study among women. Diabetes Care. 2014;37:3106–13.
Avogaro A, Giorda C, Magini M. Incidence of coronary heart disease in type 2 diabetic men and women: impact of microvascular complications, treatment, and geographic location. Diabetes Care. 2007;30(5):1241–7.
Xie J, Ikram MK, Cotch MF, et al. Association of diabetic macular edema and proliferative diabetic retinopathy with cardiovascular disease: a systematic review and meta-analysis. JAMA Ophthalmol. 2017;135(6):586–93. https://doi.org/10.1001/jamaophthalmol.2017.0988.
Agenzia Italiana del Farmaco (AIFA). Algoritmo per la terapia del diabete. [Therapeutic algorithm for diabetes]. https://www.sifoweb.it/images/pdf/ALGORITMO_AIFA_DIABETE.pdf. Accessed 20 Oct 2019.
Sarkar A, Tiwari A, Bashin P, Mitra M. Pharmacological and pharmaceutical profile of gliclazide: a review. J Appl Pharm Sci. 2011;01(09):11–9.
Chan SP, Colagiuri S. Systematic review and meta-analysis of the efficacy and hypoglycemic safety of gliclazide versus other insulinotropic agents. Diabetes Res Clin Pract. 2015;110(1):75–81.
Cordiner R, Pearson E. Reflections on the sulphonylurea story: A drug class at risk of extinction or a drug class worth reviving? Diabetes Obes Metab. 2019;21:761–71.
Khunti K, Chatterjee S, Gerstein H, et al. Do sulphonylureas still have a place in clinical practice? Lancet Diabetes Endocrinol. 2018;6(109):821–32.
Amod A. The place of sulfonylureas in guidelines: why are there differences? Diabetes Ther. 2020;11(Suppl 1):S5–S14. https://doi.org/10.1007/s13300-020-00811-3.
Mkele G. Where do sulphonylureas fit in the type 2 diabetes guidelines? S Afr Fam Pract. 2014;56(4):6–8.
Xu Y, Yang Z, Lin H, et al. Long-term patterns of antidiabetic medication use in patients with type 2 diabetes. Med Sci Monit. 2018;24:8707–15.
Kalra S, Behendeka S, Sahay R, et al. Consensus recommendations on sulfonylurea and sulfonylurea combinations in the management of type 2 diabetes mellitus International Task Force. Indian J Endocrinol Metab. 2018;22(1):132–57.
Acknowledgements
Due to the retrospective/observational characteristics of the study there was no patient, nor public involvement, aside from Patient's informed consent. Results of the study will be disseminated after their publication to physicians working in the general practice.
Funding
The present study was unconditionally supported by MSD Italy, who provided the financial coverage for study data collection and elaboration, medical writing activity, and Rapid Service fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
CBG (corresponding author) contributed to the study design, drafting of protocol, study report, data collection, interpretation of the results, and development and final editing of the manuscript. SDC, ACB, FC contributed to data collection, interpretation of the results, and development and final editing of the final manuscript. CG contributed to the study design, drafting of protocol, and data collection and approved the final manuscript. SC contributed to the study design and drafting of protocol and approved the final manuscript. BG contributed to data collection and interpretation of the results and approved the final manuscript.
Medical writing, editorial, and other assistance
The authors are grateful to all the participating centers, to Manuella Walker for her support in drafting and editing the text, Ecol Studio Spa–Divisione Yghea for its support in carrying out the study, and Carlotta Galeone for statistical consultancy.
Disclosures
Antonio Carlo Bossi has received speaker fees from Takeda and Boerhinger Ingelheim, and grants from Lilly Italy, Novo Nordisk, Sanofi Italia, Bayer, MSD, and Pikdar. Catia Guerzoni, Barbara Gilio, and Stefania Cercone are employees of MSD. Carlo Bruno Giorda, Emanuela Orsi, Salvatore De Cosmo, and Franco Cavalot have nothing to disclose.
Compliance with Ethics Guidelines
The present study was approved (no. 80/2017/U) by the Ethics Committee "Comitato Etico interaziendale AOU San Luigi Gonzaga di Orbassano AA.SS.LL. TO3–TO4–TO5" (Turin, Italy). Given the retrospective design of the study, no medical, pharmacological, or behavioral interventions were involved. All research was conducted in agreement with the principles laid out in the original Declaration of Helsinki and its later amendments, and data were handled in agreement with patient-informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due [Data are proprietary of MSD] but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12515418
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Giorda, C.B., Orsi, E., De Cosmo, S. et al. Prescription of Sulphonylureas among Patients with Type 2 Diabetes Mellitus in Italy: Results from the Retrospective, Observational Multicentre Cross-Sectional SUSCIPE (Sulphonyl_UreaS_Correct_Internal_Prescription_Evaluation) Study. Diabetes Ther 11, 2105–2119 (2020). https://doi.org/10.1007/s13300-020-00871-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-020-00871-5