Abstract
Introduction
Diabetes mellitus is a chronic disease with a high prevalence world wide. This disease has also been reported to affect the quality of life (QOL) of the patient and their family due to its chronic nature and multi organ involvement. The aim of this study was to analyze the association between adherence to prescribed diabetes medication and diabetes-specific QOL in patients attending Secondary Health Care Facility in Bandung City, Indonesia.
Methods
A cross-sectional survey was conducted in the Secondary Health Care Facility in Bandung City, Indonesia. Data were collected between February and April 2014 using consecutive sampling. Adherence was assessed using the eight-item Morisky Medication Adherence Scale while diabetes-specific-QOL was assessed using the Diabetes 39 instrument.
Results
The results showed that among the patients, 49.4% exhibited low adherence, 29.7% exhibited medium adherence, and 20.9% exhibited high adherence to diabetes medication. Diabetes-specific QOL proved to be highly affected in the sexual functioning domain. Social-burden domain scores were better than overall QOL scores. There was a significant association between adherence and diabetes-specific QOL (p = 0.009) using The Kruskall-Wallis test of significance. The results of the post hoc Mann–Whitney tests (high vs medium adherence, p = 0.084; medium vs low adherence, p = 0.86; and high vs low adherence, p = 0.001) indicated that higher adherence to prescribed diabetes medication contributed to an improved QOL. Multiple regression analysis showed that the predictors of diabetes-specific QOL were adherence and patient income.
Conclusions
Adherence to prescribed medication showed a positive effect on diabetes-specific QOL in patients. Patients with a high adherence to medication had an improved QOL. This result is important not only in developing intervention programs for patients but also in improving their QOL through sustainable health promotion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a chronic disease with a high prevalence world wide due to changing lifestyles resulting in less physical activity and increased obesity [1, 2]. The prevalence of this disease is predicted to increase by 69% in developing countries between 2010 and 2030 [1]. Treatment regimens for type 2 diabetes mellitus (T2DM) require lifestyle and behavioral changes and may influence daily functioning and well-being in patients. This disease has also been reported to affect the quality of life (QOL) of the patient and their family due to its chronic nature and multi organ involvement. Disease severity has been found to be associated with lower QOL [3]. Meanwhile, the majority of the success of long-term maintenance therapy and metabolic control in patients depends on their adherence to medication and lifestyle changes.
The clinical impact of drug therapies for diabetes has been restricted by low adherence rates [4]. The World Health Organization (WHO) has reported that the adherence rate in patients on long-term therapy for chronic diseases in developed countries is only 50%, and adherence has been reported to be even lower in developing countries [5]. Low adherence to prescribed diabetes medication leads to therapy failure and vital organ damage. Thus, therapy failure has been associated with a decrease in the benefits of therapy, leading to a higher financial burden on the patients and society at large [6].
A previous study comparing adherence between insulin and oral medication groups revealed that fewer patients in the insulin-only group (20%) discontinued their treatment compared with patients taking an oral medication group (31%) [7]. On the other hand, insulin therapy itself has been reported to be associated with decreased QOL in diabetic patients due to the pain associated with insulin administration [8]. Moreover, it is known that approximately 90% of diabetic patients have T2DM [9, 10], whom in its early and middle stage mostly still use oral medication therapy and not insulin injection as may be required in its late stage [11]. Therefore, this study solely focused on adherence to oral medication prescribed to T2DM patients.
A number of instruments are available for measuring QOL in patients with diabetes, including general instruments that are not disease-specific, and also diabetes-specific instruments. General instruments such as the 36-Item Short Form Health Survey and EuroQol five dimensions questionnaire, have been frequently used to assess QOL in patients with different illnesses [12]. On the other hand, diabetes-specific instruments specifically measure the impact of diabetes on patient functioning and well-being, and thus are more sensitive for use in diabetic patients [3]. The Diabetes 39 (D-39) Assessment Questionnaire has been recognized to have reliable psychometric properties and can be applied in a wide variety of patients [13, 14]. Furthermore, the D-39 is one of the various diabetes-specific QOL measures that has proven to be responsive to changes in patient health status [15].
Bandung City is the capital city for West Java and the most populated province in Indonesia (54.7% of Indonesian population lives in Java) [16]. Bandung City is also the second most populated city in Indonesia after Surabaya. The data analyzed in this study were obtained from Secondary Health Care Facility, Bandung City, Indonesia which is owned by the Bandung City Government. Therefore, given its geographic characteristics, we expected that Bandung City would be representative of the general Indonesian population, or at least the urban population in Indonesia.
A recent systematic review identified several disease-specific QOL indicators in patients with diabetes [14]. Unfortunately, thus far, studies examining the association between adherence and diabetes specific-QOL in patients have been inadequate. Thus, in this study, we explored the association between adherence to oral diabetes medication and disease-specific-QOL in T2DM patients attending Secondary Health Care Facility in Bandung City, Indonesia.
Methods
Study Design
A cross-sectional survey was conducted from February to April 2014 in Secondary Health Care Facility, Bandung City, Indonesia. Assuming a prevalence rate of 35% [17], a minimum sample size of 91 was required to obtain values with certainty at a 95% confidence level. Thus, data were collected by consecutive sampling who fit the following inclusion criteria: confirmed diagnosis of T2DM for over 3 months, prescribed only with oral diabetes medication, not under insulin injection therapy, more than 18 years old, and attending Secondary Health Care Facility in Bandung City, Indonesia.
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all patients after a full explanation of the objective and procedures of the study. The study protocol was approved by the Health Research Ethics Committee of the Faculty of Medicine, Universitas Padjadjaran No. 93/UN6.C2.1.2/KEPK/PN/2014.
Data Collection
Adherence was assessed using an eight-item Morisky Medication Adherence Scale (MMAS) [18]. The MMAS scale has been used for many chronic diseases including diabetes, as a self-reported measure of adherence to prescribed medication and has been found to have good reliability and predictive validity [19]. All the questions were translated into the Indonesian language and showed good validity (r > 0.3) and internal consistency, with a Cronbach’s alpha of 0.724. Respondents were classified as having low adherence if their score was less than 6, medium adherence if their score was 6 or 7, and high adherence if their score was 8.
Diabetes-specific-QOL was assessed using the D-39. The D-39 instrument was selected due to its applicability for use in the whole T2DM patient population, as it is not specific to demographic, gender, age, educational level, health status, or ethnic groups. This self-administered instrument allows patients to describe how their QOL was affected during the previous month in five dimensions (domains): energy and mobility (15 questions), diabetes control (12 questions), anxiety and worry (4 questions), social impact (5 questions), and sexual behavior (3 questions) [20]. To evaluate a multitude of effects caused by diabetes illness and treatments during the previous month, patients were asked “How much was your QOL affected”. Responses were scored on a seven-point scale that ranged from “not affected at all” (score = 1) to “extremely affected” (score = 7). The domain scores were computed by summing the responses and then applying a linear transformation to a 0–100 scale. Lower scores indicated a better QOL. The instrument was translated and validated in the Indonesian language and demonstrated good internal consistency, with a Cronbach’s alpha of 0.917.
Statistical Analysis
Descriptive statistics were used to investigate the distribution of variables among T2DM patients. Continuous variables were represented using means, standard deviations, medians, and interquartile ranges, whereas categorical variables were represented using counts and percentage. The Kruskall-Wallis test of significance (p < 0.05) was performed to assess the association between adherence and diabetes-specific QOL. A multiple regression analysis (backward selection method) was used to identify independent predictors of diabetes-specific QOL. All statistical analyses were carried out using SPSS software (version 17.0; IBM, Armonk, NY, USA).
Results
Socio-Demographic Characteristics
A sample of 91 patients with T2DM were included in this study. Table 1 shows the socio-demographic and clinical characteristics of these respondents. The average age of the respondents was 61.1 ± 9.6 years, and 71% of respondents were female. Most patients had only graduated from elementary school (42%), were not working/retired (86%), and had an average monthly household income below the regional minimum salary (72%). Most respondents (56%) were diagnosed with diabetes over 5 years prior to participation and 54% of the respondents had no family history of having diabetes.
Adherence to Prescribed Diabetes Medication
Self-reported adherence rates to prescribed diabetes medication as measured by the MMAS, indicated that 49.4% of patients had low adherence, 29.7% of patients had medium adherence, and 20.9% of patients had high adherence.
Diabetes-Specific QOL in T2DM Patients
Figure 1 shows the mean scores for diabetes-specific QOL. Social burden scores (27.5) were lower than overall QOL scores (39.1), while sexual functioning scores (52.8) were higher than overall QOL scores (39.1). Significant differences between the mean scores for energy and mobility (45.4), diabetes control (36.7), and anxiety and worry (29.8) were identified.
Association Between Adherence and Diabetes-Specific-QOL in Patients
There was a significant association between adherence and diabetes specific-QOL, as indicated by the Kruskall-Wallis test of significance (p < 0.05) (Table 2). Furthermore, these results were analyzed using post hoc Mann–Whitney tests. There was a significant difference between patients with high and low adherence in diabetes-specific QOL (p = 0.001).
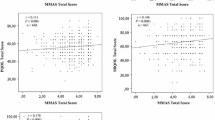
Overall mean diabetes-specific QOL scores were then plotted by level of adherence (low, medium, and high adherence) (Fig. 2). These results indicated that higher adherence to medication contributed to improve diabetes-specific QOL and vice versa. A lower overall mean of diabetes-specific QOL score indicated a better QOL.
Multiple regression analysis was used to analyze the predictors of diabetes-specific QOL. Adherence and income were found to be significant predictors of diabetes-specific QOL in patients (Table 3).
Discussion
Poor adherence to medication and a lack of understanding of medication instructions are major barriers to the treatment of T2DM. Poor adherence to medication and life-style recommendations may significantly contribute to the economic burden of this disease. The rate of high adherence identified in Bandung City was 20.9%. This result was lower than that reported in another study conducted in the United States of America (79%) [21]. This adherence rate was possibly associated with the poor quality of pharmaceutical care provided to patients. Pharmacists should provide important information including what to do if a dose is missed or an adverse effect is caused by the prescribed medication. As reported in our previous study, the average dispensing time in community pharmacy in Bandung City, Indonesia, was 62 s (varying widely from 3 to 435 s), which is above the recommended 60 s [22]. Therefore, pharmacists should allocate more time for patient consultation. In addition, another study revealed that pharmaceutical care intervention for diabetes treatment in Indonesia contributed to improvements of 17.01%; 6.73%; and 6.31% in 2 h postprandial glucose, HDL and triglyceride parameters, respectively, relative to treatment without the provision of pharmaceutical care [23].
The primary objective of diabetes management is to improve patient QOL. This study established the association between adherence and diabetes-specific QOL (and vice versa). The D-39 diabetes specific-QOL instrument has been suggested for use in research and clinical practice [14]. Furthermore, this instrument not only reflects the QOL in diabetes patients but also allows patients to frame responses based on their own personal conceptualization of QOL. These properties result in an instrument that is focused on the patients, which is important in any patient-assessed QOL measure.
A number of previous studies have attempted to analyze the association between adherence and various diabetes specific-QOL measures. However, within these studies, associations have proven to be weak [24]. Only a few domains have been analyzed [25], or only type 1 diabetes was assessed [26]. Furthermore, previous studies have focused on singular aspects of QOL (e.g., distress [24]), and neglected other key components of QOL, such as physical and social functioning [13].
This study overcame the limitations of previous studies and the results of this study enhance the current body of evidence regarding the positive association between adherence and diabetes-specific-QOL in patients. The results of the Kruskall-Wallis test showed that adherence to prescribed medication was significantly associated with diabetes-specific-QOL and vice versa (p = 0.009) in participating patients. Furthermore, the multiple linear regression model results suggested that adherence was significantly associated with diabetes specific-QOL. These results suggest that increased occurence of high adherence to diabetes-prescribed medicine was associated with better QOL and vice versa. This result also indicated the beneficial effects of the use of anti-diabetic pharmacological therapies by patients, which may have been associated with decreased pain and other diabetes-related complications.
The results of this study are in accordance with those of Farias et al. [9], suggesting that QOL in patients with DM may influence treatment adherence, satisfactorily improve clinical outcomes and reduce morbidity and mortality rates and disease progression. However, the relationship between QOL and treatment adherence remains contradictory. Some studies [27, 28] have shown that the highest QOL level in patients with DM was associated with better treatment adherence; however, other research has not identified this association [29].
Based on our previous study, the predictors of low adherence in Indonesia were complementary and alternative medicine usage [adjusted odds ratio (ORadj) 6.16; 2.44–15.52], gender (ORadj 2.57; 1.05–6.31), and age (ORadj 4.25; 1.53–11.31) [30]. In patients, adherence to medication may be associated with relieved symptoms in the short term and managed disease in the longer term, thus resulting in better social functioning and improved QOL. In contrast, a previous study by Martinez [31] showed that there was no association between medication adherence and QOL measured by the World Health Organization Quality of Life questionnaire (WHOQOL-100) in T2DM patients. That study recommended that it was necessary to investigate psychological predictors of therapy adherence behavior in T2DM patients. These different findings may be a result of differences in the instruments used, patients socio-demographics and healthcare settings.
The results of the multiple regression analysis also revealed that patient income was significantly associated with diabetes-specific QOL. As estimated, it was found that patients with lower incomes had a significantly lower QOL. This result is in agreement with prior studies by Glasgow et al. [32] and Ferrans et al. [33]. The decreased QOL in this population showed the need to reform the treatment of low-income diabetes patients.
Of all the diabetes-specific-QOL domain scores, the social burden (27.5%) was lower than the overall QOL score which indicated better QOL. In the instrument used, lower score is associated with better QOL. In contrast, a previous study showed a substantial effect (50% or more) of social functioning on QOL in patients [34]. A probable explanation for this difference is the presence of full support from the patient’s family or social support from the work environment. Social support could encourage improved psychological conditions and better adherence to prescribed diabetes medication. Better family and social support has been found to be predictive of higher adherence and better QOL [35]. Further, all the patients in this study were T2DM patients who had experienced a lower level of impact on their social life than that previously reported in type 1 diabetes patients, in whom more social control problems have been reported [36]. Thus, it is possible that patients did not worry that diabetes might limit their social relationships or friendships.
On the other hand, sexual functioning scores were higher than overall QOL scores which indicated poor QOL. In the instrument used, higher score is associated with poor QOL. This result is in accordance with a previous study that reported the sexual dysfunctions associated with diabetes have been known to decrease QOL in both males and females [37]. Sexual dysfunction has been frequently identified in diabetes mellitus patients. The prevalence of erectile dysfunction among diabetic men has been estimated to be 35–90% [38]. The topic of sexual activity is very sensitive to Indonesians and not pleasant to talk about to the public. A study of the help-seeking patterns (on the issues of sexual behavior and dysfunction) in urban populations in China, Taiwan, South Korea, Japan, Thailand, Singapore, Malaysia, Indonesia and the Philippines showed that although sexual dysfunction was frequent, socio-cultural factors seemed to prevent suffering individuals from seeking treatment [39]. A self-reported instrument is, however, still the best way to investigate complicated information. Low adherence to medications could have limited the effects of medication on pain management and sexual functioning. There were slight differences between the mean scores in the energy and mobility, diabetes control, and anxiety and worry domains. However, these domains were proven to not have an effect on diabetes patients in this study.
In this study, we restricted to only T2DM patients who used oral medication to prevent any confounding associated with insulin use that might affect adherence. We also stratified predictors into categories to minimize confounding and facilitate interpretation of the data. However, this study still had several limitations. First, the sample size of 91 patients may have limited the power of the analyses, thus, the generalizability of this study may also be limited. Subsequent studies should not only use larger and more diverse samples to ensure sufficient power and generalizability but also should use a case control study design with groups defined according adherence to therapy. In addition, other information that may influence adherence should also be assessed, such as the use of other medications and the frequency of dosage, costs, and side effects of medication. Second, our data relied on the respondents’ self-reported data regarding their medication adherence and may have been subject to recall bias. This possibility, however, should have been minimized as the MMAS has been a validated and is a self-reported instrument most widely used to assess adherence.
Conclusions
Adherence to prescribed medication was positively associated with diabetes-specific-QOL in patients. Patients with high adherence also had a better QOL. This result is useful not only in developing intervention programs for patients but also in improving their QOL through sustainable health promotion.
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14.
Abebe SM, Berhane Y, Worku A. Barriers to diabetes medication adherence in North West Ethiopia. SpringerPlus. 2014;3(1):195.
Huang I, Hwang CC, Wu MY, Lin W, Leite W, Wu AW. Diabetes-specific or generic measures for health-related quality of life? evidence from psychometric validation of the D-39 and SF-36. Value Health. 2008;11(3):450–61.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
World Health Organization. Adherence to long term therapies: evidence for action. 2003. pp. 7–9.
Wroth TH, Pathman DE. Primary medication adherence in a rural population: the role of the patient-physician relationship and satisfaction with care. J Am Board Fam Med. 2006;19(5):478–86.
Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–24.
Shim YT, Lee J, Toh MP, Tang WE, Ko Y. Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in singapore. Diabet Med. 2012;29(8):241–8.
Farias MS, Agra CC, Araújo LK, Correia DS, Cavalcante JC. Treatment adherence and life quality of diabetic patients assisted in the primary care division. Rev Soc Bras Clín Med. 2014;12(2):102–7.
Gimenes HT, Zanetti ML, Haas VJ. Factors related to patient adherence to antidiabetic drug therapy. Rev Latino Am Enfermagem. 2009;17(1):46–51.
Qaseem A, Humphrey LL, Sweet DE, Starkey M, Shekelle P. Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2012;156(3):218–31.
Anderson RM, Fitzgerald JT, Wisdom K, Davis WK, Hiss RG. A comparison of global versus disease-specific quality-of-life measures in patients with NIDDM. Diabetes Care. 1997;20(3):299–305.
Watkins K, Connel CM. Measurement of health related QOL in diabetes mellitus. Pharmacoeconomics. 2004;22:1109–26.
El Achhab Y, Nejjari C, Chikri M, Lyoussi B. Disease-specific health-related quality of life instruments among adults diabetic: a systematic review. Diabetes Res Clin Pract. 2008;80(2):171–84.
Lee LJ, Fahrbach JL, Nelson LM, McLeod LD, Martin SA, Sun P, Weinstock RS. Effects of insulin initiation on patient-reported outcomes in patients with type 2 diabetes: results from the DURABLE trial. Diabetes Res Clin Pract. 2010;89(2):157–66.
Tempo Magazine Online. 54.7% people lived in java. 2014. https://m.tempo.co/read/news/2014/02/07/092552083/sebanyak-54-7-persen-penduduk-terpusat-di-jawa. Accessed 8 Sept 2016.
Bangun AV. Faktor-faktor yang Berkontribusi terhadap Kepatuhan Pasien DM Tipe 2 dalam Konteks Asuhan Keperawatan di Poliklinik Endokrin RS Hasan Sadikin Bandung. Jakarta: Universitas Indonesia; 2009.
Morisky DE, Ang A, Krousel-Wood MA, Ward H. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Pharm. 2008;10:348–54.
Krapek K, King K, Warren SS, George KG, Caputo DA, Mihelich K, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38:1357–62.
Zulian LR, Santos MA, Veras VS, Rodrigues FFL, Arrelias CCA, Zanetti ML. Quality of life in patients with diabetes using the Diabetes 39 (D-39) instrument. Rev Gaúcha Enferm. 2013;34(3):138–46.
Boccuzzi SJ, Wogen J, Fox J, Sung JCY, Shah AB, Kim J. Utilization of oral hypoglycemic agents in a drug-insured US population. Diabetes Care. 2001;24:1411–5.
Abdulah R, Barliana M, Pradipta IS, Halimah E, Diantini A, Lestari K. Assessment of patient care indicators at community pharmacies in Bandung City, Indonesia. Southeast Asian J Trop Med Public Health. 2014;45(5):1196–201.
Insani WN, Lestari K, Abdulah R, Ghassani SK. Effect of Pharmaceutical Information Care on Clinical Outcomes of Patients with Type 2 Diabetes Mellitus. Indonesian J Clin Pharm. 2013;2(4):127–35.
Carey MP, Jorgensen RS, Weinstock RS, Sprafkin RP, Lantinga LJ, Carnrike CL, Baker MT, Meisler AW. Reliability and validity of the appraisal of diabetes scale. J Behav Med. 1991;14(1):43–51.
Hammond GS, Aoki TT. Measurement of Health Status in diabetic patients: diabetes impact measurement scales. Diabetes Care. 1992;15(4):469–77.
Bott U, Mühlhause I, Overmann H, Berger M. Validation of a diabetesspecific quality-of-life scale for patients with type 1 diabetes. Diabetes Care. 1998;21(5):757–69.
Hassan K, Loar R, Anderson BJ, Heptulla RA. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr. 2006;149(4):526–31.
Puri K, Sapra S, Jain V. Emotional, behavioral and cognitive profile, and quality of life of indian children and adolescents with type 1 diabetes. Indian J Endocrinol Metab. 2013;17(6):1078–83.
O’Neil KJ, Jonnalagadda SS, Hopkins BL, Kicklighter JR. Quality of life and diabetes knowledge of young persons with type 1 diabetes: influence of treatment modalities and demographics. J Am Diet Assoc. 2005;105(1):85–91.
Alfian SD, Sukandar H, Arisanti N, Abdulah R. Complementary and alternative medicine use decreases adherence to prescribed medication in diabetes patients. Ann Trop Med Public Health. 2016;9(3):174–9.
Martinez YV, Prado-Aguilar CA, Rascon-Pacheco RA, Valdivia-Martinez JJ. Quality of life associated with treatment adherence in patients with type 2 diabetes: a cross sectional study. BMC Health Serv Res. 2008;8:164.
Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care. 1997;20(4):562–7.
Ferrans CE, Powers MJ. Psychometric assessment of the Quality of Life Index. Res Nurs Health. 1992;15(1):29–38.
Goldney RD, Philips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life. Diabetes Care. 2004;27:1066–70.
Pereira MG, Berg-Cross L, Almeida P, Machado JC. Impact of Family Environment and Support on Adherence, Metabolic Control, and Quality of Life in Adolescents with Diabetes. Int J Behav Med. 2008;15:187–93.
Fitzgerald JT, Gruppen LD, Anderson RM, Funnell MM, Jacober SJ, Grunberger GE, Aman LC. The influence of treatment modality and ethnicity on attitudes in Type 2 diabetes. Diabetes Care. 2000;23:313–8.
De Berardis G. Erectile dysfunction and quality of life in type 2 diabetic patients: a serious problem too often overlooked. Diabetes Care. 2002;25(2):284–91.
Malavige LS, Levy JC. Erectile dysfunction in diabetes mellitus. J Sex Med. 2009;6(5):1232–47.
Hisasue S, Kumamoto Y, Sato Y, Masumori N, Horita H, Kato R, et al. Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: a Japanese female cohort study. Urology. 2005;65:143–8.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All authors named meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
SD. Alfian, H. Sukandar, K. Lestari and R. Abdulah have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in this study. Informed consent was obtained from all patients after a full explanation of the purpose and procedures used for the study. The study protocol was approved by the health research ethics committee of the Faculty of Medicine, Universitas Padjadjaran No. 93/UN6.C2.1.2/KEPK/PN/2014.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/8FE6F0602ACF776E.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Alfian, S.D., Sukandar, H., Lestari, K. et al. Medication Adherence Contributes to an Improved Quality of Life in Type 2 Diabetes Mellitus Patients: A Cross-Sectional Study. Diabetes Ther 7, 755–764 (2016). https://doi.org/10.1007/s13300-016-0203-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-016-0203-x