Abstract
Introduction
A 12-week prospective study was previously performed to assess the effect of add-on therapy with sitagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor, in patients with type 2 diabetes mellitus (T2DM) receiving insulin treatment. Patients were followed until week 48 to investigate the medium-term efficacy and safety of the add-on therapy with sitagliptin.
Methods
In the 70 patients with T2DM, glycemic control, insulin dosage, concomitant medications, body weight, laboratory parameters, and adverse events were evaluated for 48 weeks.
Results
Hemoglobin A1c (HbA1c) improved significantly from 8.03% at week 0 (at initiation of the add-on therapy) to 7.45% at week 48 (P < 0.01). Body weight remained nearly the same. The daily insulin dose was significantly reduced by 2.5 U, from 25.8 to 23.3 U/day (P < 0.001). Stratified analysis of the improvement of HbA1c based on age, duration of diabetes, body mass index, insulin regimen, and oral antidiabetic drugs did not identify any significant differences in relation to these parameters. During the 48-week follow-up period, there were no problematic adverse events, such as severe hypoglycemia, and the add-on therapy with sitagliptin showed good tolerability.
Conclusions
In Japanese patients with T2DM receiving insulin treatment, add-on therapy with sitagliptin was not associated with weight gain and allowed for the reduction of the insulin dosage. Consistent efficacy was noted for 48 weeks without an increasing hypoglycemic effect, and the add-on therapy with sitagliptin was effective irrespective of the insulin regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The usefulness of dipeptidyl peptidase-4 (DPP-4) inhibitors for the treatment of type 2 diabetes mellitus (T2DM) is widely known in Japan. While combination therapy with insulin injections and a DPP-4 inhibitor has been investigated in clinical studies [1, 2], to date only a few reports have discussed the usefulness and safety over a long treatment period [3].
Insulin regimens used in the management of T2DM include long-acting insulin given once daily, premixed insulin given twice or thrice daily, and multiple daily insulin injections (basal-bolus therapy), as well as a variety of regimens combining insulin and oral antidiabetic drugs. In insulin-treated patients with T2DM, the duration of diabetes is longer and hypo-secretion of endogenous insulin is common, but their clinical characteristics are not homogeneous. Therefore, the authors considered that prospective clinical studies should be conducted to identify the patient populations which would benefit from concomitant treatment with insulin and a DPP-4 inhibitor. The authors have previously reported the short-term results of add-on therapy with sitagliptin in patients with T2DM receiving insulin, who were assessed prospectively for 12 weeks [4]. In this study, the medium-term results of the add-on therapy with sitagliptin up to 48 weeks was evaluated by follow-up of the same patient population to monitor glycemic control, insulin dosage, concomitant drugs, body weight, and adverse events. The objective of this study was to investigate whether the combination therapy maintains good glycemic control for 48 weeks with acceptable safety.
Methods
The patients with T2DM recruited for this study were treated at Hyogo College of Medicine and Ikeda Hospital from September 2011 to June 2013, and fulfilled the following eligibility criteria. Inclusion criteria for this study were as follows: (1) age ≥20 years, (2) T2DM treated with insulin therapy [basal insulin with oral antidiabetic drugs (basal insulin therapy), twice daily injection of premixed insulin, or multiple daily insulin injections] for at least 6 months, and (3) hemoglobin A1c (HbA1c) ≥6.9% [National Glycohemoglobin Standardization Program (NGSP) value]. The exclusion criteria were the following: (1) type 1 diabetes, (2) severe complications of diabetes, (3) severe hypoglycemia or recurrent asymptomatic hypoglycemia, (4) severe infection, (5) patients scheduled for surgery or those with severe trauma, (6) pregnant or nursing women and women who could possibly become pregnant, and (7) other patients whom the investigator judged to be inappropriate for the study.
The study protocol was reviewed and approved by the Ethics Committee of Hyogo College of Medicine. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients before inclusion in the study. All subjects were given an explanation of the details of the study and voluntarily gave written informed consent to participation. After completion of the 12-week study, informed consent was again obtained to continue administration of sitagliptin.
Patients who fulfilled the above eligibility criteria continued to receive the add-on therapy with sitagliptin 50 mg given once daily after breakfast for 48 weeks. Throughout the study period, in patient instruction, emphasis was placed on avoiding hypoglycemic episodes based on data obtained by self-monitoring of blood glucose.
The primary endpoint was changes in HbA1c up to 48 weeks. HbA1c, blood glucose, and body weight were measured every 4 weeks. In addition, serum C-peptide reactivity index (CPI) was measured at weeks 0, 12, 24, and 48. Adverse events were monitored throughout the study period.
Statistical Analysis
Changes in HbA1c during sitagliptin treatment were analyzed by one-way analysis of variance. Changes in each parameter at week 48 compared to those measured at the initiation of sitagliptin treatment (baseline) were evaluated by paired t test or Mann–Whitney U test. Comparisons between groups were done with Mann–Whitney U test, Kruskal–Wallis test, or Steel–Dwass test as appropriate. For stratified analysis based on the insulin regimen, demographic data were compared by Bartlett’s test, Kruskal–Wallis test, or Chi-square test. All analyses were carried out using SAS software version 8.02 (SAS Institute Inc., Cary, NC, USA) and statistical significance was accepted at P < 0.05. Data are expressed as the mean ± standard deviation. NGSP equivalent values were calculated for HbA1c (%) values determined according to the Japan Diabetes Society (JDS) method (HbA1c [NGSP] = 1.02 × HbA1c [JDS] + 0.25%), based on the reported relationship between HbA1c (NGSP) values and HbA1c (JDS; %) values measured by the standard Japanese method.
Results
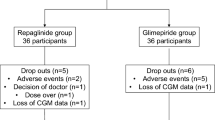
After exclusion of 1 patient who discontinued treatment after completing week 12, 70 patients were included in this study. Another patient was transferred to a different hospital during the study, therefore 69 patients completed the 48-week observation period.
Overall Results
Patient Characteristics
Table 1 shows the baseline characteristic of 70 patients enroled in the study. The mean daily insulin dose was 25.7 ± 14.8 U/day. While most patients were receiving concomitant oral antidiabetic drugs such as sulfonylureas (60.0%), α-glucosidase inhibitors (38.6%), and metformin (32.9%), 12 patients (17.1%) were on insulin monotherapy.
Changes in HbA1c
Changes in HbA1c were the primary endpoint of this study. HbA1c decreased significantly from 8.03 ± 1.07% at week 0 (at the time of initiation of the add-on therapy) to 7.51 ± 0.91% after 12 weeks (P < 0.01), 7.59 ± 1.09% after 24 weeks (P < 0.05), and 7.45 ± 1.03% after 48 weeks (P < 0.01; Fig. 1).
Changes in Other Parameters
Table 2 shows changes in other parameters after 48 weeks. Body weight remained nearly the same at 66.7 kg throughout the 48 weeks, showing no significant change. There was a significant improvement in CPI after 48 weeks. The insulin dosage also significantly decreased. After 48 weeks, insulin therapy was discontinued in 2 patients (2.9%) and the insulin dose was reduced in 35 patients (50.0%), with the mean reduction being 6.6 ± 5.3 U/day. The insulin dose was increased in 10 patients (14.3%), with a mean increase of 4.5 ± 2.3 U/day, while there was no change in insulin dosage in the remaining patients.
With regard to oral antidiabetic drugs, 42 patients were concomitantly using sulfonylureas. These drugs were discontinued in two patients (4.8%), the daily dose was decreased in 10 patients (23.8%) and increased in three patients (7.1%), and the sulfonylurea dosage was not changed in other patients.
Severe Hypoglycemia and Adverse Events
None of the patients experienced severe hypoglycemia that required assistance by a third party or treatment including intravenous infusion. In addition, none of the patients discontinued the administration of sitagliptin due to an adverse event.
Stratified Analysis by Patient Characteristics
Evaluation of Patients Responding to the Add-On Therapy
To identify patients for whom the add-on therapy with sitagliptin showed high efficacy, correlations between the hypoglycemic effect (change in HbA1c from week 0 to week 48) and various baseline characteristics were evaluated; a high baseline HbA1c was identified as a factor that was significantly associated with the decrease in HbA1c (r = −0.29249, P = 0.00180; Table 3).
Influence of Specific Factors
The influences of specific baseline factors (age, BMI, CPI, and oral hypoglycemic agents) on changes in HbA1c after 48 weeks were investigated by stratifying patients as shown in Fig. 2 For all factors, the stratified groups showed a significant decrease in HbA1c, but no significant difference was found between the groups (Fig. 2).
Changes in HbA1c from week 0 to week 48 in each subgroup stratified by a age, b BMI, c CPI, and d OHAs. α-GI alpha glucosidase inhibitor, BG biguanide, BMI body mass index, CPI C-peptide reactivity index, HbA1c hemoglobin A1c, OHA oral hypoglycemic agent, NS not significant, SD standard deviation, SU sulfonylurea
Stratified Analysis by Insulin Regimen
Profile of the Three Insulin Regimen Groups
The insulin regimen was twice daily injection of premixed insulin in 45 patients (64.3%, twice daily group), multiple daily injections of insulin in 14 patients (20.0%, multiple injections group), and basal insulin therapy in 11 patients (15.7%, basal insulin group). Table 4 shows the baseline characteristics of each group.
Changes in HbA1c by Insulin Regimens
HbA1c decreased significantly after 48 weeks in all three groups; there was no significant difference between the three insulin regimens (Fig. 3).
Changes in Other Parameters by Insulin Regimens
Table 5 shows changes in other parameters by three insulin regimens. For all parameters (body weight, CPI, and insulin dosage), there was no significant difference between the three insulin regimens in terms of changes in parameters from baseline to week 48.
Discussion
In this study that investigated the effects of the combination therapy of sitagliptin and insulin in 70 Japanese patients with T2DM, there were four main findings: (1) The insulin dosage was reduced significantly after 48 weeks without weight gain; (2) HbA1c was decreased by 0.58% after 48 weeks compared with the baseline value; (3) There were no problematic adverse events, including severe hypoglycemia; and (4) CPI was significantly higher after 48 weeks, indicating that endogenous insulin secretion was improved. These results suggested that the combination of insulin and sitagliptin is effective for the treatment of T2DM over the medium term (48 weeks) and shows good tolerability.
When the target HbA1c level cannot be achieved by insulin therapy for a certain period, the general approach is to consider changing the insulin preparation, dosage, or regimen. While a higher insulin dosage and changing the regimen may temporarily improve glycemic control, it is likely to cause an increased risk of hypoglycemia and weight gain. This can lead to a vicious cycle of deteriorating glycemic control and further insulin dose escalation, as demonstrated in some large-scale clinical studies including the United Kingdom Prospective Diabetes Study (UKPDS) [5]. To address these issues, concomitant treatment with insulin and oral antidiabetic drugs has been employed. Consequently, improvement of glycemic control, a decrease in the risk of hypoglycemia, and a reduction of the insulin dosage as a result of this concomitant treatment have been confirmed by clinical research [6]. The efficacy and safety of sitagliptin were demonstrated by a placebo-controlled double-blind study performed in Japan [2]. In the authors’ previous 12-week prospective clinical study to determine the effects of combined treatment with sitagliptin and various insulin regimens, it was found that good glycemic control was achieved without problematic adverse events, confirming the tolerability and usefulness of add-on therapy with sitagliptin [4]. The authors considered that safety and efficacy should be investigated for a longer period than 12 weeks, since T2DM requires a long-term treatment. Therefore, the patients from our previous study were followed up to week 48 in this study. The authors found that HbA1c was still significantly lower than the baseline level after 48 weeks, while there was no change in body weight compared to the baseline level. Also, no serious adverse event was observed during the 48-week observation period; thus, the results of the present study confirmed those of the previous short-term study.
Some previous studies have evaluated the effects of add-on therapy of sitagliptin in insulin-treated patients. In a randomized controlled study that compared an ongoing insulin therapy group (twice daily or more) with a sitagliptin add-on group (50 mg or 100 mg/day) in 50 Japanese patients with T2DM, a significant reduction in HbA1c and reduced insulin dosage was observed after 24 weeks in the sitagliptin add-on group [7]. There is also an observational study that investigated the effects of combination therapy of sitagliptin and insulin in Japanese patients with T2DM receiving different insulin regimens [8]. The present study is different from those studies in the following aspects. The present study demonstrated a longer-term (48 weeks) and stable glycemic control by the add-on therapy with sitagliptin. By comparing patient groups who were matched with HbA1c and other factors, the effects of the add-on therapy with sitagliptin by different insulin regimens over a longer period of time were determined. Stable efficacy across patients with different background factors such as concomitant drugs, BMI, and CPI was confirmed.
To date, the influence of sitagliptin on the insulin dosage had not been fully evaluated in Japanese patients because sitagliptin is administered in combination with a fixed dose of insulin (mainly twice daily premixed insulin). This study showed that the insulin dosage was significantly reduced after 48 weeks of the add-on therapy with sitagliptin. Among the 42 patients also receiving treatment with sulfonylureas, the sulfonylurea dosage was increased in only three patients, while it was decreased in 10 patients and sulfonylureas were discontinued in two patients. Moreover, CPI was significantly higher than baseline after 48 weeks of the add-on therapy with sitagliptin, indicating that endogenous insulin secretion was maintained and even improved. Therefore, the stable hypoglycemic effect obtained by concomitant use of sitagliptin attenuated glucotoxicity and maintained pancreatic β-cell function, leading to lower insulin dosages and dose reduction of sulfonylurea therapy. Since concomitant use of sitagliptin was not associated with an increase in the insulin dosage over the medium term (48 weeks), this combination may be beneficial for glycemic control.
The stratified analysis of the improvement of HbA1c in relation to age, duration of diabetes, BMI, CPI, insulin regimen, and oral antidiabetic drugs did not identify any of these parameters as being influential on HbA1c. In the authors’ previous 12-week investigation, improvement of HbA1c was largest in patients treated with basal insulin and sitagliptin (basal insulin group). In this study, a decrease in HbA1c was observed after 48 weeks even in the multiple injections group, and there was no significant difference in the changes in HbA1c among the three insulin regimens. As far as we know, there have been no other reports on the comparison of the HbA1c-lowering effect of the add-on therapy among three insulin regimens for the period over 24 weeks.
Moreover, there has been no report on the differences in the inhibitory effect on the increase of postprandial blood glucose. Takahara et al. [9] investigated the influence of sitagliptin combined with basal insulin on the diurnal variation of blood glucose by self-monitoring of blood glucose. They reported that both HbA1c and the M value (an index of diurnal variation of blood glucose) were significantly improved, and that diurnal variation of blood glucose was improved along with inhibition of postprandial hyperglycemia. The possibility was suggested that adding sitagliptin to twice daily premixed insulin could improve postprandial blood glucose [10]. In the twice daily group and basal insulin group in the current study, postprandial hyperglycemia had not been satisfactorily controlled prior to combined therapy, but it was improved by add-on sitagliptin; also, HbA1c decreased during the relatively short period of 12 weeks. However, the authors consider that further improvement of HbA1c over time is not likely in these patients, and other treatment will be needed. With regard to the influence of CPI on HbA1c, the authors found that HbA1c was improved without weight gain after 48 weeks of the add-on treatment, even in patients with baseline CPI <0.8 who may have insulin hypo-secretion.
In this study, there was an improvement in CPI in the twice daily insulin group, but no change was observed in the multiple injections group and the basal insulin group. The authors consider the following possible reasons: almost all patients in the multiple injections group had required basal insulin therapy at baseline. Thus, endogenous insulin secretion capacity may have been exhausted in those patients, which caused no improvement in endogenous insulin after the addition of sitagliptin. In addition, a difference in the number of patients included in each group (14 patients in the multiple injections group vs. 44 patients in the twice daily group) may have contributed. As shown in Table 5, the change in CPI was largest in the basal insulin group, followed by the multiple injections group. Nevertheless, a significant increase in CPI was observed only in the twice daily group. This may be because of the small number of patients in the multiple injections group, causing insufficient power to detect a significant difference.
Dipeptidyl peptidase-4 inhibitors have both a glucose-dependent insulinotropic effect and a glucagonostatic effect, which contribute equally to the glucose-lowering action of these drugs [11]. Sitagliptin has been reported to reduce blood glucose in patients with type 1 diabetes treated with insulin [12], and a glucagonostatic effect of glucagon-like peptide-1 receptor agonists was also reported in patients with type 1 diabetes [13]. In patients with impaired endogenous insulin secretion, it is probable that the glucagonostatic effect could be more important than the improvement of endogenous insulin secretion soon after initiation of sitagliptin treatment, while a blood glucose-lowering effect similar to that in patients with CPI ≥0.8 was seen after 48 weeks owing to improvement of insulin secretion over time as a result of the suppression of glucotoxicity.
It should be noted that the glucose-lowering efficacy of DPP-4 inhibitors may be greater in Asian populations including Japanese [14], thus, the results of the present study may be different in Western populations. In terms of the effects of sitagliptin in Caucasians, a large-scale randomized, double-blind, placebo-controlled, 24-week clinical trial in which treatment with sitagliptin 100 mg/day or placebo was administered concurrently with insulin glargine titration has been conducted [15]. The present study is similar to this study in that, the add-on therapy with sitagliptin led to a decrease in HbA1c, decreased insulin dosage and reduced hypoglycemia incidence. However, unlike the present study, the insulin therapy was limited to insulin glargine. The authors believe that the present study is beneficial as it determined the add-on effects of sitagliptin given over a longer time with different types of insulin regimens.
Conclusions
In conclusion, add-on therapy with sitagliptin maintained stable glycemic control for 48 weeks without weight gain or problematic adverse events in patients with poor baseline glycemic control despite various insulin regimens. The authors’ finding that endogenous insulin secretion was increased after 48 weeks compared with that measured at the initiation of the add-on therapy suggests that long-term treatment may be beneficial. However, a randomized controlled trial is necessary to confirm these results.
References
Vilsbøll T, Rosenstock J, Yki-Järvinen H, et al. Efficacy and safety of sitagliptin when added to insulin therapy in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12:167–77.
Kadowaki T, Tajima N, Odawara M, et al. Efficacy and safety of sitagliptin add-on therapy in Japanese patients with type 2 diabetes on insulin monotherapy. Diabetol Int. 2013;4:160–72.
Hong ES, Khang AR, Yoon JW, et al. Comparison between sitagliptin as add-on therapy to insulin and insulin dose-increase therapy in uncontrolled Korean type 2 diabetes: CSI study. Diabetes Obes Metab. 2012;14:795–802.
Katsuno T, Ikeda H, Ida K, Miyagawa J, Namba M. Add-on therapy with the DPP-4 inhibitor sitagliptin improves glycemic control in insulin-treated Japanese patients with type 2 diabetes mellitus. Endocr J. 2013;60:733–42.
UKPDS group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854–65.
Korytkowski M. When oral agents fail: practical barriers to starting insulin. Int J Obes Relat Metab Disord. 2002;26(Suppl. 3):S18–24.
Sato S, Saisho Y, Itoh H, et al. Efficacy and safety of sitagliptin added to insulin in Japanese patients with type 2 diabetes: the EDIT randomized trial. PLoS One. 2015;10:e0121988.
Takai M, Ishikawa M, Maeda H, et al. Safety and efficacy of adding sitagliptin to insulin in patients with type 2 diabetes: the ASSIST-K study. Diabetes Res Clin Pract. 2014;103:e30–3.
Takahara M, Shiraiwa T, Kaneto H, Katakami N, Matsuoka TA, Shimomura I. Efficacy of sitagliptin on blood glucose fluctuation in Japanese type 2 diabetic patients with basal-supported oral therapy. Endocr J. 2012;59:1131–6.
Mori Y, Taniguchi Y, Miyazaki S, Yokoyama J, Utsunomiya K. Effects of add-on treatment with sitagliptin on narrowing the range of glucose fluctuations in Japanese type 2 diabetes patients receiving insulin therapy. Diabetes Technol Ther. 2013;15:237–40.
Hare KJ, Vilsbøll T, Asmar M, Deacon CF, Knop FK, Holst JJ. The glucagonostatic and insulinotropic effects of glucagon-like peptide 1 contribute equally to its glucose-lowering action. Diabetes. 2010;59:1765–70.
Ellis SL, Moser EG, Snell-Bergeon JK, Rodionova AS, Hazenfield RM, Garg SK. Effect of sitagliptin on glucose control in adult patients with type 1 diabetes: a pilot, double-blind, randomized, crossover trial. Diabet Med. 2011;28:1176–81.
Kielgast U, Krarup T, Holst JJ, Madsbad S. Four weeks of treatment with liraglutide reduces insulin dose without loss of glycemic control in type 1 diabetic patients with and without residual beta-cell function. Diabetes Care. 2011;34:1463–8.
Kim YG, Hahn S, Oh TJ, et al. Difference in the glucose-lowering efficacy of dipeptidyl peptidase-4 inhibitors between Asians and non-Asians: a systematic review and meta-analysis. Diabetologia. 2013;56:696–708.
Mathieu C, Shankar RR, Lorber D, et al. A randomized clinical trial to evaluate the efficacy and safety of co-administration of sitagliptin with intensively titrated insulin glargine. Diabetes Ther. 2015;6:127–42.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. The article processing charges for this publication were funded by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval of the version to be published.
Disclosures
Tomoyuki Katsuno, Hiroki Ikeda, and Mitsuyoshi Namba declare no conflict of interest.
Compliance with Ethics Guidelines
The study protocol was reviewed and approved by the Ethics Committee of Hyogo College of Medicine. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients. All subjects were given an explanation of the details of the study and voluntarily gave written informed consent to participation. Informed consent was again obtained to continue administration of sitagliptin after week 12 of the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to www.medengine.com/Redeem/61C4F0606CCAA2A7.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Katsuno, T., Ikeda, H. & Namba, M. Medium-Term Effect of Add-On Therapy with the DPP-4 Inhibitor, Sitagliptin, in Insulin-Treated Japanese Patients with Type 2 Diabetes Mellitus. Diabetes Ther 7, 309–320 (2016). https://doi.org/10.1007/s13300-016-0170-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-016-0170-2