Abstract
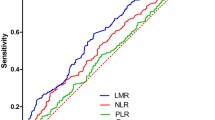
Prognostic value of peripheral monocyte, as a member of inflammatory cells, was widely being investigated. The aim of this study was to evaluate the prognostic value of preoperative peripheral blood monocyte count for hepatocellular carcinoma (HCC) patients who underwent liver transplantation (LT) and the relationship between monocyte count and tumor-related characteristics. We retrospectively analyzed the clinical data of 101 HCC patients after LT. Preoperative monocyte count and demographic, clinical, and pathologic data were analyzed. The optimal cutoff value of monocyte count was 456/mm3, with the sensitivity and specificity of 69.4 and 61.5 %, respectively. Elevated preoperative peripheral blood monocyte count was significantly associated with large tumor size. The 1-, 3-, and 5-year disease-free survival (DFS) (80.9, 70.1, and 53.3 % vs 55.1, 38.7, and 38.7 %, P = 0.007) and overall survival (OS) rates (95.7, 76.6, and 64.8 % vs 72.2, 44.1, and 36.1 %, P = 0.002) of HCC patients in the peripheral blood monocyte count ≤456/mm3 group were higher than those in the peripheral blood monocyte count >456/mm3 group. In conclusion, elevated preoperative peripheral blood monocyte count was significantly associated with advanced tumor stage and it can be considered as a prognostic factor for HCC patients after LT.


Similar content being viewed by others
References
Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2:533–43.
Zhang TT, Zhao XQ, Liu Z, Mao ZY, Bai L. Factors affecting the recurrence and survival of hepatocellular carcinoma after hepatectomy: a retrospective study of 601 Chinese patients. Clin Transl Oncol. 2015.
Zhou YM, Zhang XF, Li B, Sui CJ, Yang JM. Postoperative complications affect early recurrence of hepatocellular carcinoma after curative resection. BMC Cancer. 2015;15:689.
Zhou D, Zhang Y, Xu L, Zhou Z, Huang J, Chen M. A monocyte/granulocyte to lymphocyte ratio predicts survival in patients with hepatocellular carcinoma. Sci Rep. 2015;5:15263.
Lin ZX, Ruan DY, Li Y, Wu DH, Ma XK, Chen J, et al. Lymphocyte-to-monocyte ratio predicts survival of patients with hepatocellular carcinoma after curative resection. World J Gastroenterol. 2015;21(38):10898–906.
Shen SL, Fu SJ, Huang XQ, Chen B, Kuang M, Li SQ, et al. Elevated preoperative peripheral blood monocyte count predicts poor prognosis for hepatocellular carcinoma after curative resection. BMC Cancer. 2014;14:744.
Lee SD, Kim SH, Kim YK, Lee SA, Park SJ. Prognostic significance of preoperative peripheral blood monocyte ratio in patients with hepatocellular carcinoma. World J Surg. 2014;38:2377–85.
Pinato DJ, Stebbing J, Ishizuka M, Khan SA, Wasan HS, North BV, et al. A novel and validated prognostic index in hepatocellular carcinoma: the inflammation based index (IBI). J Hepatol. 2012;57:1013–20.
Huang J, Xu L, Luo Y, He F, Zhang Y, Chen M. The inflammation-based scores to predict prognosis of patients with hepatocellular carcinoma after hepatectomy. Med Oncol. 2014;31:883.
Parisi I, Tsochatzis E, Wijewantha H, Rodríguez-Perálvarez M, De Luca L, Manousou P, et al. Inflammation-based scores do not predict post-transplant recurrence of hepatocellular carcinoma in patients within Milan criteria. Liver Transpl. 2014;20:1327–35.
Sasaki A, Iwashita Y, Shibata K, Matsumoto T, Ohta M, Kitano S. Prognostic value of preoperative peripheral blood monocyte count in patients with hepatocellular carcinoma. Surgery. 2006;139:755–64.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:633–9.
Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33:1394–403.
Zheng SS, Xu W, Wu J, Chen J, Wang WL, Zhang M, et al. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 2008;85:1726–32.
Han M, Guo ZY, Zhao Q, Wang XP, Yuan XP, Jiao XY, et al. Liver transplantation using organs from deceased organ donors: a single organ transplant center experience. Hepatobiliary Pancreat Dis Int. 2014;13:409–15.
Chai EZ, Siveen KS, Shanmugam MK, Arfuso F, Sethi G. Analysis of the intricate relationship between chronic inflammation and cancer. Biochem J. 2015;468:1–15.
Kidane D, Chae WJ, Czochor J, Eckert KA, Glazer PM, Bothwell AL, et al. Interplay between DNA repair and inflammation, and the link to cancer. Crit Rev Biochem Mol Biol. 2014;49:116–39.
Atsumi T, Singh R, Sabharwal L, Bando H, Meng J, Arima Y, et al. Inflammation amplifier, a new paradigm in cancer biology. Cancer Res. 2014;74:8–14.
Hung RJ, Ulrich CM, Goode EL, Brhane Y, Muir K, Chan AT, et al. Cross cancer genomic investigation of inflammation pathway for five common cancers: lung, ovary, prostate, breast, and colorectal cancer. J Natl Cancer Inst. 2015. doi:10.1093/jnci/djv246.
Bishayee A. The role of inflammation and liver cancer. Adv Exp Med Biol. 2014;816:401–35.
Nakagawa H, Maeda S. Inflammation- and stress-related signaling pathways in hepatocarcinogenesis. World J Gastroenterol. 2012;18:4071–81.
Posner LJ, Miligkos T, Gilles JA, Carnes DL, Taddeo DR, Graves DT. Monocyte chemoattractant protein-1 induces monocyte recruitment that is associated with an increase in numbers of osteoblasts. Bone. 1997;21:321–7.
Craig MJ, Loberg RD. CCL2 (monocyte chemoattractant protein-1) in cancer bone metastases. Cancer Metastasis Rev. 2006;25:611–9.
Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11:762–74.
Wu Y, Kuang DM, Pan WD, Wan YL, Lao XM, Wang D, et al. Monocyte/macrophage-elicited natural killer cell dysfunction in hepatocellular carcinoma is mediated by CD48/2B4 interactions. Hepatology. 2013;57:1107–16.
Ji J, Eggert T, Budhu A, Forgues M, Takai A, Dang H, et al. Hepatic stellate cell and monocyte interaction contributes to poor prognosis in hepatocellular carcinoma. Hepatology. 2015;62:481–95.
Acknowledgments
This study was supported by the National High Technology Research and Development Program of China (863 Program) (2012AA021007 and 2012AA021008), the Key Clinical Project from the Ministry of Health (2010159), the National Natural Science Foundation of China (81373156 and 81471583), the Special Fund for Science Research by Ministry of Health (201302009), and the Guangdong Provincial Key Laboratory Construction Projection on Organ Donation and Transplant Immunology (2013A061401007). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authors’ contributions
QQR, SJF, LWW, and XSH were the main authors of the manuscript. They were involved in the conception, design, and coordination of the study as well as in data analysis, interpretation of results, and drafting the manuscript. LWW and XSH were in charge of all experimental procedures. QZ, ZYG, FJ, and MGC participated in the experimental procedures and revised critically the content of the manuscript. All authors contributed to the interpretation of data and critically revised the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None
Additional information
Qing-Qi Ren and Shun-Jun Fu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ren, QQ., Fu, SJ., Zhao, Q. et al. Prognostic value of preoperative peripheral monocyte count in patients with hepatocellular carcinoma after liver transplantation. Tumor Biol. 37, 8973–8978 (2016). https://doi.org/10.1007/s13277-015-4758-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4758-3