Abstract
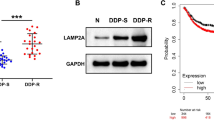
The CD44 isoform containing variant exon v6 (CD44v6) plays an important role in the progression, metastasis, and prognosis of colorectal cancer (CRC). Recently, it was found that CD44v6 is involved in acquired drug resistance. This study aimed to investigate the molecular mechanism of CD44v6 in the resistance of CRC cells to chemotherapy. A stable CD44v6 overexpression model in SW480 cells was established via lentiviral transduction. The chemosensitivity of cells to 5-fluorouracil (5-FU) and oxaliplatin (L-OHP) was determined by cell counting kit (CCK)-8, lactate dehydrogenase (LDH) release, and colony formation assays. Immunohistochemical staining of CD44v6 was performed in human CRC tissues. The key components in cell apoptosis, drug efflux and metabolism, mismatch repair, autophagy, epithelial–mesenchymal transition (EMT), and the PI3K–Akt and MAPK–Ras–Erk1/2 pathways were assessed using flow cytometry, quantitative real-time polymerase chain reaction (PCR), and western blot assays. The CD44v6 overexpression cells showed a higher viability, a lower LDH release rate, and an increased clonogenicity than the control cells under drug treatment. Moreover, overexpression of CD44v6 resulted in enhanced autophagy flux, EMT, and phosphorylation of Akt and Erk in the presence of drugs. Furthermore, high CD44v6 expression in the primary tumor was closely associated with an early recurrence in CRC patients who underwent curative surgery and adjuvant chemotherapy. In conclusion, overexpression of CD44v6 contributes to chemoresistance in SW480 cells under cytotoxic stress via the modulation of autophagy, EMT, and activation of the PI3K–Akt and MAPK–Ras–Erk pathways.








Similar content being viewed by others
References
Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, et al. Colorectal cancer. Lancet. 2010;375(9719):1030–47.
Holohan C, Van Schaeybroeck S, Longley DB, Johnston PG. Cancer drug resistance: an evolving paradigm. Nat Rev Cancer. 2013;13(10):714–26. doi:10.1038/nrc3599.
Longley DB, Johnston PG. Molecular mechanisms of drug resistance. J Pathol. 2005;205(2):275–92. doi:10.1002/path.1706.
De Mattia E, Cecchin E, Toffoli G. Pharmacogenomics of intrinsic and acquired pharmacoresistance in colorectal cancer: toward targeted personalized therapy. Drug Resist Updat. 2015;20:39–70. doi:10.1016/j.drup.2015.05.003.
Perez-Tomas R. Multidrug resistance: retrospect and prospects in anti-cancer drug treatment. Curr Med Chem. 2006;13(16):1859–76. doi:10.2174/092986706777585077.
Glavinas H, Krajcsi P, Cserepes J, Sarkadi B. The role of ABC transporters in drug resistance, metabolism and toxicity. Curr Drug Deliv. 2004;1(1):27–42. doi:10.2174/1567201043480036.
Townsend DM, Tew KD. The role of glutathione-S-transferase in anti-cancer drug resistance. Oncogene. 2003;22(47):7369–75. doi:10.1038/sj.onc.1206940.
Giles GI, Sharma RP. Topoisomerase enzymes as therapeutic targets for cancer chemotherapy. Med Chem. 2005;1(4):383–94.
Kirschner K, Melton DW. Multiple roles of the ERCC1-XPF endonuclease in DNA repair and resistance to anticancer drugs. Anticancer Res. 2010;30(9):3223–32.
Lage H, Dietel M. Involvement of the DNA mismatch repair system in antineoplastic drug resistance. J Cancer Res Clin Oncol. 1999;125(3–4):156–65.
Rodriguez-Nieto S, Zhivotovsky B. Role of alterations in the apoptotic machinery in sensitivity of cancer cells to treatment. Curr Pharm Des. 2006;12(34):4411–25.
Lai K, Killingsworth MC, Lee CS. The significance of autophagy in colorectal cancer pathogenesis and implications for therapy. J Clin Pathol. 2014;67(10):854–8. doi:10.1136/jclinpath-2014-202529.
McCubrey JA, Steelman LS, Kempf CR, Chappell WH, Abrams SL, Stivala F, et al. Therapeutic resistance resulting from mutations in Raf/MEK/ERK and PI3K/PTEN/Akt/mTOR signaling pathways. J Cell Physiol. 2011;226(11):2762–81. doi:10.1002/jcp.22647.
Sui H, Zhu L, Deng WL, Li Q. Epithelial-mesenchymal transition and drug resistance: role, molecular mechanisms, and therapeutic strategies. Oncol Res Treat. 2014;37(10):584–9. doi:10.1159/000367802.
Ponta H, Sherman L, Herrlich PA. CD44: from adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol. 2003;4(1):33–45. doi:10.1038/nrm1004.
Coppola D, Hyacinthe M, Fu L, Cantor AB, Karl R, Marcet J, et al. CD44V6 expression in human colorectal carcinoma. Hum Pathol. 1998;29(6):627–35.
Zlobec I, Gunthert U, Tornillo L, Iezzi G, Baumhoer D, Terracciano L, et al. Systematic assessment of the prognostic impact of membranous CD44v6 protein expression in colorectal cancer. Histopathology. 2009;55(5):564–75. doi:10.1111/j.1365-2559.2009.03421.x.
Todaro M, Gaggianesi M, Catalano V, Benfante A, Iovino F, Biffoni M, et al. CD44v6 is a marker of constitutive and reprogrammed cancer stem cells driving colon cancer metastasis. Cell Stem Cell. 2014;14(3):342–56. doi:10.1016/j.stem.2014.01.009.
Reinhold WC, Sunshine M, Liu H, Varma S, Kohn KW, Morris J, et al. Cell miner: a web-based suite of genomic and pharmacologic tools to explore transcript and drug patterns in the NCI-60 cell line set. Cancer Res. 2012;72(14):3499–511. doi:10.1158/0008-5472.CAN-12-1370.
Larionov A, Krause A, Miller W. A standard curve based method for relative real time PCR data processing. BMC Bioinformatics. 2005;6:62. doi:10.1186/1471-2105-6-62.
Klionsky DJ, Abdalla FC, Abeliovich H, Abraham RT, Acevedo-Arozena A, Adeli K, et al. Guidelines for the use and interpretation of assays for monitoring autophagy. Autophagy. 2012;8(4):445–544.
Yanamoto S, Yamada S, Takahashi H, Naruse T, Matsushita Y, Ikeda H, et al. Expression of the cancer stem cell markers CD44v6 and ABCG2 in tongue cancer: effect of neoadjuvant chemotherapy on local recurrence. Int J Oncol. 2014;44(4):1153–62. doi:10.3892/ijo.2014.2289.
Costa S, Terzano P, Bovicelli A, Martoni A, Angelelli B, Santini D, et al. CD44 isoform 6 (CD44v6) is a prognostic indicator of the response to neoadjuvant chemotherapy in cervical carcinoma. Gynecol Oncol. 2001;80(1):67–73. doi:10.1006/gyno.2000.6016.
Bendardaf R, Lamlum H, Ristamaki R, Pyrhonen S. CD44 variant 6 expression predicts response to treatment in advanced colorectal cancer. Oncol Rep. 2004;11(1):41–5.
Niu RF, Zhang J, Huang JY. Expression of CD44v6 before and after chemotherapy in patients with breast cancer and its significance. Ai Zheng. 2002;21(1):71–4.
Recio JA, Merlino G. Hepatocyte growth factor/scatter factor induces feedback up-regulation of CD44v6 in melanoma cells through Egr-1. Cancer Res. 2003;63(7):1576–82.
Gao C, Guo H, Downey L, Marroquin C, Wei J, Kuo PC. Osteopontin-dependent CD44v6 expression and cell adhesion in HepG2 cells. Carcinogenesis. 2003;24(12):1871–8. doi:10.1093/carcin/bgg139.
Li J, Zha XM, Wang R, Li XD, Xu B, Xu YJ, et al. Regulation of CD44 expression by tumor necrosis factor-alpha and its potential role in breast cancer cell migration. Biomed Pharmacother. 2012;66(2):144–50. doi:10.1016/j.biopha.2011.11.021.
Quinones A, Dobberstein KU, Rainov NG. The egr-1 gene is induced by DNA-damaging agents and non-genotoxic drugs in both normal and neoplastic human cells. Life Sci. 2003;72(26):2975–92.
Damm S, Koefinger P, Stefan M, Wels C, Mehes G, Richtig E, et al. HGF-promoted motility in primary human melanocytes depends on CD44v6 regulated via NF-kappa B, Egr-1, and C/EBP-beta. J Invest Dermatol. 2010;130(7):1893–903. doi:10.1038/jid.2010.45.
Hebbard L, Steffen A, Zawadzki V, Fieber C, Howells N, Moll J, et al. CD44 expression and regulation during mammary gland development and function. J Cell Sci. 2000;113(Pt 14):2619–30.
Ni J, Cozzi PJ, Hao JL, Beretov J, Chang L, Duan W, et al. CD44 variant 6 is associated with prostate cancer metastasis and chemo-/radioresistance. Prostate. 2014;74(6):602–17. doi:10.1002/pros.22775.
Miletti-Gonzalez KE, Chen S, Muthukumaran N, Saglimbeni GN, Wu X, Yang J, et al. The CD44 receptor interacts with P-glycoprotein to promote cell migration and invasion in cancer. Cancer Res. 2005;65(15):6660–7. doi:10.1158/0008-5472.CAN-04-3478.
Liu CM, Chang CH, Yu CH, Hsu CC, Huang LL. Hyaluronan substratum induces multidrug resistance in human mesenchymal stem cells via CD44 signaling. Cell Tissue Res. 2009;336(3):465–75. doi:10.1007/s00441-009-0780-3.
Misra S, Ghatak S, Toole BP. Regulation of MDR1 expression and drug resistance by a positive feedback loop involving hyaluronan, phosphoinositide 3-kinase, and ErbB2. J Biol Chem. 2005;280(21):20310–5. doi:10.1074/jbc.M500737200.
Xu ZY, Tang JN, Xie HX, Du YA, Huang L, Yu PF, et al. 5-Fluorouracil chemotherapy of gastric cancer generates residual cells with properties of cancer stem cells. Int J Biol Sci. 2015;11(3):284–94. doi:10.7150/ijbs.10248.
Mathew R, Karantza-Wadsworth V, White E. Role of autophagy in cancer. Nat Rev Cancer. 2007;7(12):961–7. doi:10.1038/nrc2254.
Li J, Hou N, Faried A, Tsutsumi S, Takeuchi T, Kuwano H. Inhibition of autophagy by 3-MA enhances the effect of 5-FU-induced apoptosis in colon cancer cells. Ann Surg Oncol. 2009;16(3):761–71. doi:10.1245/s10434-008-0260-0.
Sasaki K, Tsuno NH, Sunami E, Kawai K, Hongo K, Hiyoshi M, et al. Resistance of colon cancer to 5-fluorouracil may be overcome by combination with chloroquine, an in vivo study. Anticancer Drugs. 2012;23(7):675–82. doi:10.1097/CAD.0b013e328353f8c7.
Sasaki K, Tsuno NH, Sunami E, Tsurita G, Kawai K, Okaji Y, et al. Chloroquine potentiates the anti-cancer effect of 5-fluorouracil on colon cancer cells. BMC Cancer. 2010;10:370. doi:10.1186/1471-2407-10-370.
Park JM, Huang S, Wu TT, Foster NR, Sinicrope FA. Prognostic impact of Beclin 1, p62/sequestosome 1 and LC3 protein expression in colon carcinomas from patients receiving 5-fluorouracil as adjuvant chemotherapy. Cancer Biol Ther. 2013;14(2):100–7. doi:10.4161/cbt.22954.
Zaanan A, Park JM, Tougeron D, Huang S, Wu TT, Foster NR, et al. Association of beclin 1 expression with response to neoadjuvant chemoradiation therapy in patients with locally advanced rectal carcinoma. Int J Cancer. 2015;137(6):1498–502. doi:10.1002/ijc.29496.
Ogier-Denis E, Pattingre S, El Benna J, Codogno P. Erk1/2-dependent phosphorylation of Galpha-interacting protein stimulates its GTPase accelerating activity and autophagy in human colon cancer cells. J Biol Chem. 2000;275(50):39090–5. doi:10.1074/jbc.M006198200.
Levine B, Sinha S, Kroemer G. Bcl-2 family members—dual regulators of apoptosis and autophagy. Autophagy. 2008;4(5):600–6.
Graziani A, Gramaglia D, Cantley LC, Comoglio PM. The tyrosine-phosphorylated hepatocyte growth factor/scatter factor receptor associates with phosphatidylinositol 3-kinase. J Biol Chem. 1991;266(33):22087–90.
Orian-Rousseau V, Chen L, Sleeman JP, Herrlich P, Ponta H. CD44 is required for two consecutive steps in HGF/c-Met signaling. Genes Dev. 2002;16(23):3074–86. doi:10.1101/gad.242602.
Klingbeil P, Marhaba R, Jung T, Kirmse R, Ludwig T, Zoller M. CD44 variant isoforms promote metastasis formation by a tumor cell-matrix cross-talk that supports adhesion and apoptosis resistance. Mol Cancer Res. 2009;7(2):168–79. doi:10.1158/1541-7786.MCR-08-0207.
Jung T, Gross W, Zoller M. CD44v6 coordinates tumor matrix-triggered motility and apoptosis resistance. J Biol Chem. 2011;286(18):15862–74. doi:10.1074/jbc.M110.208421.
Acknowledgments
This work was supported by the Science Foundation from the Health Bureau of Wenzhou City of Zhejiang, China (Y20140713) and by the Incubation Program from The First Affiliated Hospital of Wenzhou Medical University (FHY2014013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Lin Lv and Hai-Guang Liu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lv, L., Liu, HG., Dong, SY. et al. Upregulation of CD44v6 contributes to acquired chemoresistance via the modulation of autophagy in colon cancer SW480 cells. Tumor Biol. 37, 8811–8824 (2016). https://doi.org/10.1007/s13277-015-4755-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4755-6