Abstract
Purpose
Very high-risk, ductal-dependent or complex two-ventricle patients with associated comorbidities often require pulmonary blood flow restriction as bridge to a more definitive procedure, but current surgical options may not be well-tolerated. An evolving alternative utilizes a fenestrated Micro Vascular Plug (MVP) as a transcatheter, internal pulmonary artery band. In this study, we report a case series and an in-vitro evaluation of the MVP to elicit understanding of the challenges faced with device implantation.
Methods
Following single-center, retrospective review of eight patients who underwent device placement, an in-vitro flow study was conducted on MVP devices to assess impact of device and fenestration sizing on pulmonary blood flow. A mathematical model was developed to relate migration risk to vessel size. Results of the engineering analysis were compared to the clinical series for validation.
Results
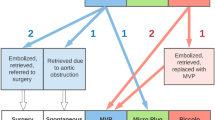
At median follow-up of 8 months (range 1–15), survival was 63% (5/8), and 6 (75%) patients underwent subsequent target surgical intervention with relatively low mortality (1/6). Occluder-related challenges included migration (63%) and peri-device flow, which were evaluated in-vitro. The device demonstrated durability over normal and supraphysiologic conditions with minimal change in fenestration size. Smaller vessel size significantly increased pressure gradient due to reduced peri-device flow and smaller effective fenestration size.
Conclusion
Device oversizing, with appropriate adjustment to fenestration size, may reduce migration risk and provide a clinically appropriate balance between resulting pressure gradient and Qp:Qs. Our results can guide the interventionalist in appropriately selecting the device and fenestrations based on patient-specific anatomy and desired post-implantation flow characteristics.






Similar content being viewed by others
Abbreviations
- CO:
-
Cardiac output
- HLHS:
-
Hypoplastic left heart syndrome
- LPA:
-
Left pulmonary artery
- LV:
-
Left ventricle
- MPA:
-
Main pulmonary artery
- MVP:
-
Micro Vascular PlugTM
- PA:
-
Pulmonary artery
- PAB:
-
Pulmonary artery banding
- PBF:
-
Pulmonary blood flow
- PDA:
-
Patent ductus arteriosus
- PFR:
-
Pulmonary flow restrictor
- PTFE:
-
Polytetrafluoroethylene
- Qp:Qs:
-
Pulmonary-systemic flow ratio
- SV:
-
Single ventricle
References
Akintuerk, H., et al. Stenting of the arterial duct and banding of the pulmonary arteries: basis for combined Norwood stage I and II repair in hypoplastic left heart. Circulation. 105(9):1099–1103, 2002. https://doi.org/10.1161/hc0902.104709.
Baba, K., et al. Hybrid versus norwood strategies for single-ventricle palliation. Circulation. 126(11):1, 2012. https://doi.org/10.1161/CIRCULATIONAHA.111.084616.
Berry, J. M., R. Gurumurthy, H. Elisabeth, H. Do, and J. L. Bass. Echocardiographic imaging of the Medtronic Micro Vascular Plug TM during off label placement in the premature infant with patent ductus arteriosus. Echocardiography. 3:944–947, 2019. https://doi.org/10.1111/echo.14335.
Ceneri, N. M., et al. Hybrid strategy in neonates with ductal-dependent systemic circulation and multiple risk factors. J. Thorac. Cardiovasc. Surg. 2022. https://doi.org/10.1016/j.jtcvs.2021.11.103.
Chetan, D., et al. Surgical palliation strategy does not affect interstage ventricular dysfunction or atrioventricular valve regurgitation in children with hypoplastic left heart syndrome and variants. Circulation. 128(1):205–212, 2013. https://doi.org/10.1161/CIRCULATIONAHA.112.000380.
Dibardino, D. J., K. Kleeman, and E. L. Bove. A method of transcutaneously adjustable pulmonary artery banding for staged left ventricular retraining. J. Thorac. Cardiovasc. Surg. 144(3):553–556, 2012. https://doi.org/10.1016/j.jtcvs.2011.09.077.
Galantowicz, M., et al. Hybrid approach for hypoplastic left heart syndrome: intermediate results after the learning curve. Ann. Thorac. Surg. 85(6):2063–2071, 2008. https://doi.org/10.1016/j.athoracsur.2008.02.009.
Guyon, P., et al. Institutional trend in device selection for transcatheter PDA Closure in premature infants. Pediatr. Cardiol. 43:1716–1722, 2022.
Haddad, R. N., D. Bonnet, and S. M. Milani. Embolization of vascular abnormalities in children with congenital heart diseases using medtronic micro vascular plugs. Heart Vessels. 37(7):1271–1282, 2022. https://doi.org/10.1007/s00380-021-02007-6.
Karamlou, T., et al. Stage 1 hybrid palliation for hypoplastic left heart syndrome-assessment of contemporary patterns of use: an analysis of the society of thoracic surgeons congenital heart surgery database. J. Thorac. Cardiovasc. Surg. 149(1):195-202.e1, 2015. https://doi.org/10.1016/j.jtcvs.2014.08.020.
Khan, A. H., et al. Utility of the Medtronic microvascular plugTM as a transcatheter implantable and explantable pulmonary artery flow restrictor in a swine model. Catheter. Cardiovasc. Interv. 93(7):1320–1328, 2019. https://doi.org/10.1002/ccd.28162.
Kurtz, J. D., B. Alsoufi, S. J. Wilkens, and E. Kim. Modified microvascular plug as a flow restrictor in hypoplastic left heart syndrome with dysplastic tricuspid and pulmonary valves. Pediatr. Cardiol. 42(7):1653–1657, 2021. https://doi.org/10.1007/s00246-021-02701-2.
Lin, M. T., et al. Alternative approach for selected severe pulmonary hypertension of congenital heart defect without initial correction - Palliative surgical treatment. Int. J. Cardiol. 151(3):313–317, 2011. https://doi.org/10.1016/j.ijcard.2010.05.067.
Makhija, N., S. Aggarwal, S. Talwar, S. Ladha, D. Das, and U. Kiran. Management of iatrogenic pulmonary artery injury during pulmonary artery banding. Ann. Card. Anaesth. 20(3):379–380, 2017. https://doi.org/10.4103/aca.ACA_47_17.
Mollet, A., B. Stos, D. Bonnet, D. Sidi, and Y. Boudjemline. Development of a device for transcatheter pulmonary artery banding: evaluation in animals. Eur. Heart J. 27(24):3065–3072, 2006. https://doi.org/10.1093/eurheartj/ehl354.
Nageotte, S., S. Shahanavaz, P. Eghtesady, and D. Balzer. Total transcatheter stage 1: a word of caution. Pediatr. Cardiol. 42(6):1410–1415, 2021. https://doi.org/10.1007/s00246-021-02626-w.
Nakahata, Y., et al. Re-expandable covered stent: preliminary animal study. Kitasato Med. 2:165–169, 2011.
Park, S. C., et al. A percutaneously adjustable device for banding of the pulmonary trunk. Int. J. Cardiol. 9(4):477–484, 1985. https://doi.org/10.1016/0167-5273(85)90243-8.
Pinho, P., U. O. Von Oppell, J. Brink, and J. Hewitson. Pulmonary artery banding; adequacy and long-term outcome. Eur. J. Cardio-thoracic Surg. 11(1):105–111, 1997. https://doi.org/10.1016/S1010-7940(96)01049-4.
Rychik, J., J. J. Rome, M. H. Collins, W. M. Decampli, and T. L. Spray. The hypoplastic left heart syndrome with intact atrial septum: atrial morphology, pulmonary vascular histopathology and outcome. J. Am. Coll. Cardiol. 34(2):554–560, 1999. https://doi.org/10.1016/S0735-1097(99)00225-9.
Scheurer, M. A., et al. Abstract 16450: left ventricular coronary-cameral fistulae in the mitral stenosis-aortic atresia variant of hypoplastic left heart syndrome are associated with poor outcomes. Circulation. 122(21):A16450–A16450, 2010. https://doi.org/10.1161/circ.122.suppl_21.A16450.
Schranz, D., et al. Fifteen-year single center experience with the ‘giessen hybrid’ approach for hypoplastic left heart and variants: current strategies and outcomes. Pediatr. Cardiol. 36(2):365–373, 2015. https://doi.org/10.1007/s00246-014-1015-2.
Solis, E., C. F. Heck, J. B. Seward, and M. P. Kaye. Percutaneously adjustable pulmonary artery band. Ann. Thorac. Surg. 41(1):65–69, 1986. https://doi.org/10.1016/S0003-4975(10)64498-0.
Stoica, S. C., et al. The retrograde aortic arch in the hybrid approach to hypoplastic left heart syndrome. Ann. Thorac. Surg. 88(6):1939–1947, 2009. https://doi.org/10.1016/j.athoracsur.2009.06.115.
Tanem, J., N. Rudd, J. Rauscher, A. Scott, M. A. Frommelt, and G. D. Hill. Survival after norwood procedure in high-risk patients. Ann. Thorac. Surg. 109(3):828–833, 2020. https://doi.org/10.1016/j.athoracsur.2019.07.070.
Vad, S., A. Eskinazi, T. Corbett, T. McGloughlin, and J. P. V. Geest. “Determination of coefficient of friction for self-expanding stent-grafts. J. Biomech. Eng. 132(12):1–10, 2010. https://doi.org/10.1115/1.4002798.
Vida, V. L., et al. Hypoplastic left heart syndrome with intact or highly restrictive atrial septum : surgical experience from a single center. Ann. Thoracic Surgery 2007. https://doi.org/10.1016/j.athoracsur.2007.04.017.
Walsh, K. P., P. Oslizlok, M. B. Brian, and D. Kenny. Use of the Medtronic Microvascular Plug 7Q for transcatheter closure of large patent ductus arteriosus in infants weighing. Catheter. Cardiovasc. Interv. 1:1545–1550, 2022. https://doi.org/10.1002/ccd.30105.
Wang-giuffre, E. W., and J. P. Breinholt. Novel use of the medtronic micro vascular plug for PDA closure in preterm infants. Catheter. Cardiovasc. Interv. 1065(6):1059–1065, 2017. https://doi.org/10.1002/ccd.26855.
Yoshimura, N., et al. Pulmonary artery banding still has an important role in the treatment of congenital heart disease [2] (multiple letters). Ann. Thorac. Surg. 79(4):1463–1464, 2005. https://doi.org/10.1016/j.athoracsur.2003.12.113.
Acknowledgements
None.
Funding
This work was supported by internal funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.B. Kizilski, D.P. Recco, F. Sperotto, N. Lang, P.E. Hammer, C.W. Baird, N. Maschietto, D.M. Hoganson declare that they have no conflicts of interest.
Informed Consent
This study was approved by the Boston Children’s Hospital Institutional Review Board (IRB-P000044617) with waiver of consent.
Meeting Presentations
None.
Additional information
Associate Editor Patrick Segers, PhD oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kizilski, S.B., Recco, D.P., Sperotto, F. et al. Transcatheter Pulmonary Artery Banding in High-Risk Neonates: In-Vitro Study Provoked by Initial Clinical Experience. Cardiovasc Eng Tech 14, 640–654 (2023). https://doi.org/10.1007/s13239-023-00674-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-023-00674-2