Abstract
Purpose
The Berlin Heart EXCOR (BH) is the only FDA-approved, extracorporeal pulsatile ventricular assist device (VAD) for infants and children with heart failure. Clinicians control four settings on the device—systolic and diastolic drive pressures, device pump rate, and systolic time as a percentage of the pump cycle. However, interactions between BH pneumatics and the native circulation remain poorly understood. Thus, establishing appropriate device size and settings can be challenging on a patient-to-patient basis.
Methods
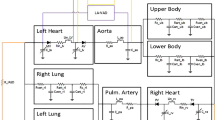
In this study we develop a novel lumped parameter network based on simplified device mechanics. We perform parametric studies to characterize device behavior, study interactions between the left ventricle (LV) and BH across different device settings, and develop patient-specific simulations. We then simulate the impact of changing device parameters for each of three patients.
Results
Increasing systolic pressure and systolic time increased device output. We identified previously unobserved cycle-to-cycle variations in LV–BH interactions that may impact patient health. Patient-specific simulations demonstrated the model’s ability to replicate BH performance, captured trends in LV behavior after device implantation, and emphasized the importance of device rate and volume in optimizing BH efficiency.
Conclusion
We present a novel, mechanistic model that can be readily adjusted to study a wide range of device settings and clinical scenarios. Physiologic interactions between the BH and the native LV produced large variability in cardiac loading. Our findings showed that operating the BH at a device rate greater than the patient’s native heart decreases variability in physiological interactions between the BH and LV, increasing cardiac offloading while maintaining cardiac output. Device rates that are close to the resting heart rate may result in unfavorable cardiac loading conditions. Our work demonstrates the utility of our model to investigate BH performance for patient-specific physiologies.










Similar content being viewed by others
References
Adachi, I., and R. D. Jaquiss. Mechanical circulatory support in children. Current Cardiol. Rev. 12:132–140, 2016.
Almond, C., D. Morales, E. Blackstone, M. Turrentine, M. Imamura, M. Massioctte, L. Jordan, E. Devaney, C. Ravishankar, K. Kanter, W. Holman, R. Kroslowitz, C. Tjossem, L. Thuita, G. Cohen, H. Buchholz, J. St Louis, K. Nguyen, R. Niebler, B. Reemtsen, P. den Wear-, O. Reinhartz, K. Guleserian, M. Mitchell, M. Bleiweis, C. Canter, and T. Humpl. Berlin Heart EXCOR pediatric ventricular assist device for bridge to heart transplantation in US children. Circulation. 127:1702–1711, 2013.
Ascher, U. M., and L. R. Petzold. Computer Methods for Ordinary Differential Equations and Differential-Algebraic Equations. SIAM, 1998.
Avrahami, I., M. Rosenfeld, S. Raz, and S. Einav. Numerical model of flow in a sac-type ventricular assist device. Artif. Organs. 30:529–538, 2006.
BH GmbH. EXCOR Pediatric VAD: Ventricular Assist Device with Stationary Driving Unit Ikus Rev 21, Instructions for Use 1000721x09 Revision 8. GmbH BH, 2015.
Blume, E. D., D. C. Naftel, H. J. Bastardi, B. W. Duncan, J. K. Kirklin, and S. A. Webber. Outcomes of children bridged to heart ttransplantation with ventricular assist devices. Circulation. 113:2313–2319, 2006.
Caimi, A., F. Sturla, B. Good, M. Vidotto, R. DePonti, F. Piatti, K. B. Manning, and A. Redaelli. Toward the virtual benchmarking of pneumatic ventricular assist devices: application of a novel fluid-structure interaction-based strategy to the Penn state 12 cc device. J. Biomech. Eng. 139:081008, 2017.
Center BCH Hospital BC. Z-Score Calculator. Center BCH Hospital BC, 2020.
Chan, C. H. H., S. Diab, K. Moody, O. H. Frazier, L. C. Sampaio, C. D. J. Fraser, and J. Teruya. Adachi in vitro hemocompatibility evaluation of ventricular assist devices in pediatric flow conditions: a benchmark study. Artif. Organs. 42:1028–1034, 2018.
Cheng, W., B. Li, J. Kajstura, P. Li, M. Wolin, E. Sonnenblick, T. Hintze, G. Olivetti, and P. Anversa. Stretch-induced programmed myocyte cell death. J. Clin. Investig. 96:2247–2259, 1995.
Committee AHAS Subcommittee SS. Heart disease and stroke statistics–2006 update. Circulation. 113:85–151, 2006.
Dandel, M., and R. Hetzer. Recovery of failing hearts by mechanical unloading: pathophysiologic insights and clinical relevance. Am. Heart J. 206:30–50, 2018.
Fleeter, C. M., G. Geraci, D. E. Schiavazzi, A. M. Kahn, and A. L. Marsden. Multilevel and multifidelity uncertainty quantification for cardiovascular hemodynamics. Comput. Methods Appl. Mech. Eng. 365:113030, 2020.
Hetzer, R., F. Kaufmann, and E. M. D. Walter. Paediatric mechanical circulatory support with Berlin Heart EXCOR: development and outcome of a 23-year experience. Eur. J. Cardio-Thorac. Surg. 50:203–210, 2016.
Irving, C. A., D. S. Crossland, S. Haynes, M. Griselli, A. Hasan, and R. Kirk. Evolving experience with explantation from the Berlin Heart EXCOR ventricular assist device support in children. J. Heart Lung Transpl. 33:211–213, 2013.
Konig, C., and M. Mokhtarzadeh-Dehghan. Investigation of unsteady flow in a model of a ventricular assist device by numerical modelling and comparison with experiment. Med. Eng. Phys. 21:53–64, 1999.
Kung, E., G. Pennati, F. Migliavacca, T. Y. Hsia, R. Figliola, A. Marsden, A. Giardini, and M. Investigators. A simulation protocol for exercise physiology in Fontan patients using a closed loop lumped-parameter model. J. Biomech. Eng. 136:8, 2014.
Long, C., A. Marsden, and Y. Bazilevs. Fluid–structure interaction simulation of pulsatile ven tricular assist devices. Comput. Mech. J. 52:971–981, 2013.
Mackling, T., T. Shah, V. Dimas, K. Guleserian, M. Sharma, J. Forbess, M. Ardura, J. Gross-Toalson, Y. Lee, J. Journeycake, and B. Aliessa. Management of single-ventricle patients with berlin heart EXCOR ventricular assist devices: single-center experience. Aritif. Organs. 36:555–559, 2012.
Mancini, D. M., A. Beniaminovitz, H. Levin, K. Catanesse, M. Flannery, M. DiTullio, S. Savin, M. E. Cardisco, E. Rose, and M. Oz. Low incidence of myocardial recovery after left ventricular assist device implantation in patients with chronic heart failure. Circulation. 98:2383–2389, 1998.
Marsden, A. L. Simulation based planning of surgical interventions in pediatric cardiology. Phys. Fluids. 25:101303, 2013.
Marsden, A. L., Y. Bazilevs, C. C. Long, and M. Behr. Recent advances in computational method- ology for simulation of mechanical circulatory assist devices. Wiley Interdiscip. Rev. 6:169–188, 2014.
Miera, O., K. R. Schmitt, E. Delmo-Walter, S. Ovroutski, R. Hetzer, and F. Berger. Pump size of Berlin Heart EXCOR pediatric device influences clinical outcome in children. J. Heart Lung Transpl. 33:816–821, 2014.
Migliavacca, F., G. Pennati, G. Dubini, R. Fumero, R. Pietrabissa, G. Urcelay, E. Bove, T. Hsia, and M. de Leval. Modeling of the Norwood circulation: effects of shunt size, vascular resistances, and heart rate. Am. J. Physiol. Heart Circ. Physiol. 280:H2076–H2086, 2001.
Minnath, M. A., G. Unnikrishnan, and E. Purushothaman. Transport studies of thermoplastic polyurethane/natural rubber (TPU/NR) blends. J. Membr. Sci. 379:361–369, 2011.
Morena, G. E., A. Charroqui, M. L. Pilan, R. H. Magliola, M. P. Krynski, M. Althabe, L. M. Landry, G. Sciuccati, A. Villa, and H. Vogelfang. Clinical experience with Berlin Heart Excor in pediatric patients in Argentina: 1373 days of cardiac support. Pediatr. Cardiol. 32:652–658, 2011.
Mynard, J., M. Davidson, D. Penny, and J. Smolich. A simple, versatile valve model for use in lumped parameter and one-dimensional cardiovascular models. Int. J. Numer. Methods Biomed. Eng. 28:626–641, 2012.
Nandi, D., and J. W. Rossano. Epidemiology and cost of heart failure in children. Cardiol. Young. 25:1460–1468, 2015.
Obidowski, D., P. Reorowicz, D. Witkowski, K. Sobczak, and K. Jozwik. Methods for determination of stagnation in pneumatic ventricular assist devices. Int. J. Artif. Organs. 41:653–663, 2018.
Odell, W. G. Accuracy of the left ventricular cavity volume and ejection fraction for conventional estimation methods and 3D surface fitting. J. Am. Heart Assoc. 8:e009124, 2010.
Orr, Y., A. Jeewa, M. C. McGarry, and I. Adachi. Upsizing of a Berlin Heart EXCOR pediatric left ventricular assist device to achieve adequate flow requirement. J. Heart Lung Transpl. 32:845–846, 2013.
Pekkan, K., D. Frakes, D. De Zelicourt, C. W. Lucas, W. J. Parks, and A. P. Yoganathan. Coupling pediatric ventricle assist devices to the fontan circulation: simulations with a lumped-parameter model. Am. Soc. Artif. Internal Organs. 51:618–628, 2005.
Pratap, J. N., and S. Wilmshurst. Anesthetic management of children with in situ Berlin Heart EXCOR. Pediatr. Anesth. 20:812–820, 2010.
Roszelle, B. N., B. T. Cooper, T. C. Long, S. Deutsch, and K. B. Manning. The 12 cc penn state pulsatile pediatric assist device: flow field observations at a reducated beat rate with application to weaning. Am. Soc. Artif. Organs. 54:325–331, 2008.
Roudaut, R., K. Serri, and S. Lafitte. Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations. Heart. 93:137–142, 2007.
Schiavazzi, D. E., A. Baretta, G. Pennati, T. Y. Hsia, and A. L. Marsden. Patient-specific parameter estimation in single-ventricle lumped circulation models under uncertainty. Int. J. Numer. Methods Biomed. Eng. 33:e02799, 2016.
Schmidt, T. M. Computational Evaluation of Ventricular Assist Device Implementation in the Single Ventricle Circulation. All Theses, 2016.
Schubert, K., T. Schaller, E. Stojenthin, C. Stephan, H. H. Sievers, and M. Scharfschwerdt. A novel trileaflet mechanical heart valve: first in vitro results. Interactive Cardiovasc. Thorac. Surg. 28:689–694, 2019.
Shi, Y., P. Lawford, and R. Hose. Review of zero-D and 1-D models of blood flow in the cardiovascular system. BioMed. Eng. OnLine. 10:1–38, 2011.
Shimizue, S., T. Kawada, Y. Hayam, A. Kamiya, T. Shishido, and M. Sugimachi. Lumped parameter model for hemodynamic simulation of congenital heart diseases. J. Physiol. Sci. 68:103–111, 2018.
Sievert, A., C. Wiesener, A. Arndt, W. Drewelow, and O. Simanski. Control of An Extracorporeal Heart Assist Device. IEEE International Conference on Control Applications. 15:63–68, 2012.
Sousa, D., T. Cordeiro, T. Melo, N. J. da Rocha, I. Cestari, and A. Lima. Modeling, characterization and test of a pediatric ventricular assist device. J. Phys. 1044:e12047, 2018.
Timoshenko, S., and S. Woinowsky-Krieger. Theory of Plates and Shells. New York: McGraw-Hill Book Company, 1959.
Uriel, N., G. Sayer, S. Annamalai, N. K. Kapur, and D. Burkhoff. Mechanical unloading in heart failure. J. Am. Coll. Cardiol. 72:569–580, 2018.
Wermelt, J. Z., O. Honjo, A. Kilic, G. van Arsdell, C. Gruenwald, and T. Humpl. Use of a Pulsatile Ventricular Assist Device (Berlin Heart EXCOR) and an Interventional Lung Assist Device (Novalung) in an animal model. Am. Soc. Artif. Internal Organs. 54:498–503, 2008.
Zimmerman, H., D. Covington, S. Richard, C. Inaht, B. Barber, and J. Copeland. Recovery of dilated cardiomyopathies in infants and children using left ventricular assist devices. Am. Soc. Artif. Internal Organs. 65:364–368, 2010.
Acknowledgments
We gratefully acknowledge the clinical expertise of Dr. Chris Almond, Dr. Katsuhide Maeda, Jenna Murray, NP, and Don Sheff, CCP and the assistance of our clinical research coordinator, Matthew Irvin. We also thank Stanford Undergraduate Advising and Research for their financial support.
Funding
This study was funded by Stanford Undergraduate Advising and Research Major Grant.
Data Availability
Not applicable.
Code Availability
Not applicable.
Conflict of interest
V. Yuan, A. Verma, N.K. Schiavone, and A.L. Marsden declare they have no conflicts of interest. D.N. Rosenthal is a co-leader at the Advanced Cardiac Therapies Improving Outcomes Network (ACTION Network), which receives funding from Berlin Heart EXCOR.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Igor Efimov oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yuan, V., Verma, A., Schiavone, N.K. et al. A Mechanistic Lumped Parameter Model of the Berlin Heart EXCOR to Analyze Device Performance and Physiologic Interactions. Cardiovasc Eng Tech 13, 603–623 (2022). https://doi.org/10.1007/s13239-021-00603-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00603-1