Abstract
Purpose
Peristaltic pumps (PP) are favored in flow bioreactors for their non-contact sterile design. But they produce pulsatile flow, which is consequential for the cultured cells. A novel pulse damper (PD) is reported for pulsatility elimination.
Methods
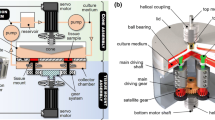
The PD design was implemented to target static pressure pulsatility and flow rate (velocity) pulsatility from a PP. Damping effectiveness was tested in a macro-scale, closed-loop recirculating bioreactor mimicking the aortic arch at flow rates up to (4 L/min). Time-resolved particle image velocimetry was used to characterize the velocity field. Endothelial cells (EC) were grown in the bioreactor, and subjected to continuous flow for 15 min with or without PD.
Results
The PD was found to be nearly 90% effective at reducing pulsatility. The EC exposed to low PP flow without PD exhibited distress signaling in the form of increased ERK1/2 phosphorylation (2.5 folds) when compared to those exposed to the same flow with PD. At high pump flow without PD, the cells detached and did not survive, while they were perfectly healthy with PD.
Conclusions
Flow pulsatility from PP causes EC distress at low flow and cell detachment at high flow. Elevated temporal shear stress gradient combined with elevated shear stress magnitude at high flow are believed to be the cause of cell detachment and death. The proposed PD design was effective at minimizing the hemodynamic stressors in the pump’s output, demonstrably reducing cell distress. Adoption of the proposed PD design in flow bioreactors should improve experimental protocols.











Similar content being viewed by others
Abbreviations
- CCD:
-
Charge coupled device
- EC:
-
Endothelial cells
- ERK:
-
Extra-cellular signal-regulated kinase
- fps:
-
Frames per second
- HUVEC:
-
Human umbilical vein endothelial cells
- ID:
-
Inner diameter
- MAP:
-
Mitogen activated protein
- OD:
-
Outer diameter
- OSI:
-
Oscillatory shear stress
- PD:
-
Pulse damper
- PDMS:
-
Polydimethylsiloxane
- PIV:
-
Particle image velocimetry
- PP:
-
Peristaltic pump
- psig:
-
Pound per square inch, gauge
- RPM:
-
Revolution per minute
- \(f\) :
-
Flow signal (pressure, flow rate, or shear stress)
- \(\varvec{p}\) :
-
Static pressure
- \(\varvec{q}\) :
-
Flow rate
- \(\varvec{u}\left( \varvec{y} \right)\) :
-
Flow velocity distribution near the vessel wall
- \(y\) :
-
Perpendicular distance from the vessel wall
- \(\mu\) :
-
Dynamic viscosity
- \(\varvec{\tau}_{\varvec{w}}\) :
-
Wall shear stress
- \(\varvec{\psi}\) :
-
Damping effectiveness based on signal standard deviation
- \(\phi\) :
-
Damping effectiveness based on signal peak-to-peak
- \({\mathbf{K}}\) :
-
Peak-to-peak of a waveform or signal
- \({\varvec{\upsigma}}\) :
-
Standard deviation of a waveform or signal
- \(\varvec{D}\) :
-
Damped
- \(\varvec{U}\) :
-
Un-damped
References
Alloush, M. M., G. F. Oweis, R. Nasr, and A. Zeidan. An aortic arch flow loop for the study of hemodynamic-induced endothelial cell injury and inflammation. In: 2014 Middle East Conference on Biomedical Engineering (MECBME), (pp. 67–70), 2014.
Alloush M. M., G. F. Oweis, R. Nasr, and A. Zeidan. Flow Measurements in a Matched-Index-of-Refraction Aortic Arch Model for Endothelial Cell Culture. In: ASME 2014 4th Joint US-European Fluids Engineering Division Summer Meeting. American Society of Mechanical Engineers, 2014.
Asmar, E., G. Bejjani, R. Chamoun, J. Hachem, G. Oweis, and M. Liermann. Experimental Study on Active Pneumatic Damping of Pulsatile Flow Delivered From Peristaltic Pump. In: ASME/BATH 2017 Symposium on Fluid Power and Motion Control, pp. V001T01A066.
Bao, X., C. B. Clark, and J. A. Frangos. Temporal gradient in shear-induced signaling pathway: involvement of MAP kinase, c-fos, and connexin43. Am. J. Physiol.-Heart Circ. Physiol. 278(5):H1598–H1605, 2000.
Beller, C. J., et al. Role of aortic root motion in the pathogenesis of aortic dissection. Circulation 109.6:763–769, 2004.
Berger, S. A., L. Talbot, and L. S. Yao. Flow in curved pipes. Annu. Rev. Fluid Mech. 15(1):461–512, 1983.
Borsa, J. J., E. K. Hoffer, R. Karmy-Jones, A. B. Fontaine, R. D. Bloch, J. K. Yoon, C. R. So, M. H. Meissner, and S. Demirer. Angiographic description of blunt traumatic injuries to the thoracic aorta with specific relevance to endograft repair. J. Endovasc. Ther. 9(Suppl 2):II-84–II-91, 2002.
Carrisoza-Gaytan, R., Y. Liu, D. Flores, C. Else, H. G. Lee, G. Rhodes, R. M. Sandoval, T. R. Kleyman, F. Y. Lee, B. Molitoris, L. M. Satlin, and R. Rohatgi. Effects of biomechanical forces on signaling in the cortical collecting duct (CCD). Am. J. Physiol. Renal. Physiol. 307(2):F195–F204, 2014.
Cavalcante, J. L., J. A. C. Lima, A. Redheuil, and M. H. Al-Mallah. Aortic stiffness: current understanding and future directions. J. Am. Coll. Cardiol. 57(14):1511–1522, 2011.
Chiu, J. J., and S. Chien. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol. Rev. 91(1):327–387, 2011.
Davis, R. J. The mitogen-activated protein kinase signal transduction pathway. J. Biol. Chem. 268:14553–14556, 1993.
Dekker, R. J., J. V. van Thienen, J. Rohlena, S. C. de Jager, Y. W. Elderkamp, J. Seppen, and A. J. Horrevoets. Endothelial KLF2 links local arterial shear stress levels to the expression of vascular tone-regulating genes. Am. J. Pathol. 167(2):609–618, 2005.
Deng, R., Y. Cheng, and C. H. Wang. Experiments and simulation on a pulse dampener system for stabilizing liquid flow. Chem. Eng. J. 210:136–142, 2012.
DePaola, N., M. A. Gimbrone, P. F. Davies, and C. F. Dewey. Vascular endothelium responds to fluid shear stress gradients. Arterioscler. Thromb. Vasc. Biol. 12(11):1254–1257, 1992.
Dougherty, F. C., F. M. Donovan, Jr, and M. I. Townsley. Harmonic analysis of perfusion pumps. J. Biomech. Eng. 125(6):814–822, 2003.
Dudash, L. A., F. Kligman, S. M. Sarett, K. Kottke-Marchant, and R. E. Marchant. Endothelial cell attachment and shear response on biomimetic polymer-coated vascular grafts. J. Biomed. Mater. Res. Part A 100(8):2204–2210, 2012.
Estrada, R., G. A. Giridharan, M. D. Nguyen, T. J. Roussel, M. Shakeri, V. Parichehreh, and P. Sethu. Endothelial cell culture model for replication of physiological profiles of pressure, flow, stretch, and shear stress in vitro. Anal. Chem. 83(8):3170–3177, 2011.
Ha, C. H., S. Kim, J. Chung, S. H. An, and K. Kwon. Extracorporeal shock wave stimulates expression of the angiogenic genes via mechanosensory complex in endothelial cells: mimetic effect of fluid shear stress in endothelial cells. Int. J. Cardiol. 168(4):4168–4177, 2013.
Hahn, M. S., M. K. McHale, E. Wang, R. H. Schmedlen, and J. L. West. Physiologic pulsatile flow bioreactor conditioning of poly (ethylene glycol)-based tissue engineered vascular grafts. Ann. Biomed. Eng. 35(2):190–200, 2007.
Han, D., and M. G. Mungal. Simultaneous measurements of velocity and CH distributions. Part 1: jet flames in co-flow. Combust Flame 132:565–590, 2003.
Herricks, T., K. B. Seydel, G. Turner, M. Molyneux, R. Heyderman, T. Taylor, and P. K. Rathod. A microfluidic system to study cytoadhesion of Plasmodium falciparum infected erythrocytes to primary brain microvascularendothelial cells. Lab Chip 11(17):2994–3000, 2011.
Hoenicka, M., L. Wiedemann, T. Puehler, S. Hirt, D. E. Birnbaum, and C. Schmid. Effects of shear forces and pressure on blood vessel function and metabolism in a perfusion bioreactor. Ann. Biomed. Eng. 38(12):3706–3723, 2010.
Hsiai, T. K., S. K. Cho, H. M. Honda, S. Hama, M. Navab, L. L. Demer, and C. M. Ho. Endothelial cell dynamics under pulsating flows: significance of high versus low shear stress slew rates (∂ τ/∂ t). Ann. Biomed. Eng. 30(5):646–656, 2002.
Ishibazawa, A., T. Nagaoka, T. Takahashi, K. Yamamoto, A. Kamiya, J. Ando, and A. Yoshida. Effects of shear stress on the gene expressions of endothelial nitric oxide synthase, endothelin-1, and thrombomodulin in human retinal microvascular endothelial cells. Invest. Ophthalmol. Vis. Sci. 52(11):8496–8504, 2011.
Jin, S., J. Oshinski, and D. P. Giddens. Effects of wall motion and compliance on flow patterns in the ascending aorta. J. Biomech. Eng. 125(3):347–354, 2003.
Kang, H., Y. Fan, and X. Deng. Vascular smooth muscle cell glycocalyx modulates shear-induced proliferation, migration, and NO production responses. Am. J. Physiol.-Heart. Circ. Physiol. 300(1):H76–H83, 2010.
Keynton, R. S., M. M. Evancho, R. L. Sims, N. V. Rodway, A. Gobin, and S. E. Rittgers. Intimal hyperplasia and wall shear in arterial bypass graft distal anastomoses: an in vivo model study. J. Biomech. Eng. 123(5):464–473, 2001.
Kinney, M. A., C. Y. Sargent, and T. C. McDevitt. The multiparametric effects of hydrodynamic environments on stem cell culture. Tissue Eng. Part B 17(4):249–262, 2011.
Kopsachilis, N., K. T. Tsaousis, I. T. Tsinopoulos, and U. Welge-Luessen. Air toxicity for primary human-cultured corneal endothelial cells: an in vitro model. Cornea 32(4):e31–e35, 2013.
Lantz, J., J. Renner, and M. Karlsson. Wall shear stress in a subject specific human aorta—influence of fluid-structure interaction. Int. J. Appl. Mech. 3(04):759–778, 2011.
Lee, H. Y., and O. Byung-Hee. Aging and arterial stiffness. Circ. J. 74(11):2257–2262, 2010.
Lee, E. J., and L. E. Niklason. A novel flow bioreactor for in vitro microvascularization. Tissue Eng. Part C 16(5):1191–1200, 2010.
Li, M., Y. Tan, K. R. Stenmark, and W. Tan. High pulsatility flow induces acute endothelial inflammation through overpolarizing cells to activate NF-κB. Cardiovasc. Eng. Technol. 4(1):26–38, 2013.
Liermann, M. Active pneumatic pulsation damper for peristaltic pump flow loops. In: BATH/ASME 2016 Symposium on Fluid Power and Motion Control, p. V001T01A005.
Liu, X., P. Fang, Y. Fan, X. Deng, D. Li, and S. Li. A numerical study on the flow of blood and the transport of LDL in the human aorta: the physiological significance of the helical flow in the aortic arch. Am. J. Physiol.-Heart Circ. Physiol. 297(1):H163–H170, 2009.
London, G. M., and A. P. Guerin. Influence of arterial pulse and reflected waves on blood pressure and cardiac function. Am. Heart J. 138(3):S220–S224, 1999.
Lu, L., M. Mende, X. Yang, H. F. Körber, H. J. Schnittler, S. Weinert, J. Heubach, C. Werner, and U. Ravens. Design and validation of a bioreactor for simulating the cardiac niche: a system incorporating cyclic stretch, electrical stimulation, and constant perfusion. Tissue Eng. Part A 19(3–4):403–414, 2012.
Mahler, G. J., C. M. Frendl, Q. Cao, and J. T. Butcher. Effects of shear stress pattern and magnitude on mesenchymal transformation and invasion of aortic valve endothelial cells. Biotechnol. Bioeng. 111(11):2326–2337, 2014.
Mebratu, Y., and Y. Tesfaigzi. How ERK1/2 activation controls cell proliferation and cell death: is subcellular localization the answer? Cell cycle 8(8):1168–1175, 2009.
Nordgaard, H., A. Swillens, D. Nordhaug, I. Kirkeby-Garstad, D. Van Loo, N. Vitale, P. Segers, R. Haaverstad, and L. Lovstakken. Impact of competitive flow on wall shear stress in coronary surgery: computational fluid dynamics of a LIMA–LAD model. Cardiovasc. Res. 88(3):512–519, 2010.
Peattie, R. A., E. Golden, R. S. Nomoto, C. M. Margossian, F. Q. Pancheri, E. S. Edgar, M. D. Iafrati, and A. L. Dorfmann. A technique for comparing wall pressure distributions in steady flow through rigid versus flexible patient-based abdominal aortic aneurysm phantoms. Exp. Tech. 40(4):1187–1201, 2016.
Pedroso, P. D., B. L. Hershey, W. Holman, R. Venugopalan, and A. S. Anayiotos. The hemodynamic effects of compliance, bulging, and curvature in a saphenous vein coronary artery bypass graft model. Technol. Health Care 11(6):443–455, 2002.
Reymond, P., P. Crosetto, S. Deparis, A. Quarteroni, and N. Stergiopulos. Physiological simulation of blood flow in the aorta: comparison of hemodynamic indices as predicted by 3-D FSI, 3-D rigid wall and 1-D models. Med. Eng. Phys. 35(6):784–791, 2013.
Riquelme, M. A., S. Burra, R. Kar, P. D. Lampe, and J. X. Jiang. MAPK Activated by Prostaglandin E2 Phosphorylates Connexin 43 and Closes Osteocytic Hemichannels in Response to Continuous Flow Shear Stress. J Biol Chem; jbc.M115.683417, 2015.
Seger, R., and E. G. Krebs. The MAPK signaling cascade. FASEB J. 9:726–735, 1995.
Siddharthan, V., Y. V. Kim, S. Liu, and K. S. Kim. Human astrocytes/astrocyte-conditioned medium and shear stress enhance the barrier properties of human brain microvascular endothelial cells. Brain Res. 1147:39–50, 2007.
Stevens, M. C., F. M. Callaghan, P. Forrest, P. G. Bannon, and S. M. Grieve. Flow mixing during peripheral veno-arterial extra corporeal membrane oxygenation—a simulation study. J. Biomech. 55:64–70, 2017.
Tsai, T. T., M. S. Schlicht, K. Khanafer, J. L. Bull, D. T. Valassis, D. M. Williams, R. Berguer, and K. A. Eagle. Tear size and location impacts false lumen pressure in an ex vivo model of chronic type B aortic dissection. J. Vasc. Surg. 47(4):844–851, 2008.
Viggers, R. F., A. R. Wechezak, and L. R. Sauvage. An apparatus to study the response of cultured endothelium to shear stress. J. Biomech. Eng. 108(4):332–337, 1986.
Voigt, E. E., C. F. Buchanan, M. N. Rylander, and P. P. Vlachos. Wall shear stress measurements in an arterial flow bioreactor. Cardiovasc. Eng. Technol. 3(1):101–111, 2012.
Voyvodic, P. L., D. Min, and A. B. Baker. A multichannel dampened flow system for studies on shear stress-mediated mechanotransduction. Lab Chip 12(18):3322–3330, 2012.
White, C. R., H. Y. Stevens, M. Haidekker, and J. A. Frangos. Temporal gradients in shear, but not spatial gradients, stimulate ERK1/2 activation in human endothelial cells. Am. J. Physiol.-Heart Circ. Physiol. 289(6):H2350–H2355, 2005.
Wootton, D. M., and D. N. Ku. Fluid mechanics of vascular systems, diseases, and thrombosis. Annu. Rev. Biomed. Eng. 1(1):299–329, 1999.
Yamawaki, H., S. Pan, R. T. Lee, and B. C. Berk. Fluid shear stress inhibits vascular inflammation by decreasing thioredoxin-interacting protein in endothelial cells. J. Clin. Investig. 115(3):733–738, 2005.
Zeidan, A., S. Javadov, and M. Karmazyn. Essential role of Rho/ROCK-dependent processes and actin dynamics in mediating leptin-induced hypertrophy in rat neonatal ventricular myocytes. Cardiovasc. Res. 72(1):101–111, 2006.
Zhang, B., C. Peticone, S. K. Murthy, and M. Radisic. A standalone perfusion platform for drug testing and target validation in micro-vessel networks. Biomicrofluidics 7(4):044125, 2013.
Zhu, C., J. H. Seo, and R. Mittal. Computational modelling and analysis of haemodynamics in a simple model of aortic stenosis. J. Fluid Mech. 851:23–49, 2018.
Zou, Y., Y. Hu, B. Metzler, and Q. Xu. Signal transduction in arteriosclerosis: mechanical stress activated MAP kinases in vascular smooth muscle cells. Int. J. Mol. Med. 1:827–834, 1998.
Acknowledgments
Casting molds for the arched bioreactor model were produced via CNC machining by J. Nassif and J. Zoullikian. GFO thanks Prof. SL Ceccio from U. Michigan for hosting his sabbatical which made the production of this manuscript possible.
Funding
This work was supported by the American University of Beirut through the Faculty of Engineering and Architecture (Dar-Shair Grant), and the Faculty of Medicine (F. Jabre Grant).
Conflict of interest
M.M. Alloush declares that he has no conflict of interest. M. Liermann declares that he has no conflict of interest. A Zedan declares that he has no conflict of interest. G.F. Oweis declares that he has no conflict of interest.
Ethical Approval
No human studies were carried out by the authors for this article. No animal studies were carried out by the authors for this article. The HUVEC culture used in this study was obtained commercially.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jonathan Butcher and Ajit P. Yoganathan oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alloush, M.M., Liermann, M., Zedan, A. et al. A Novel Pulse Damper for Endothelial Cell Flow Bioreactors. Cardiovasc Eng Tech 10, 95–111 (2019). https://doi.org/10.1007/s13239-018-00394-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-018-00394-y