Abstract
Introduction
In carcinoma of cervix, if overall treatment time (OTT) is prolonged beyond 6 weeks, then the total dose required to achieve a given probability of tumor control is to be increased by 0.6 Gy for each day of prolongation, to control the accelerative repopulation of the cells, i.e., 1 % loss of tumor control, and to avoid increased treatment delays and drop outs due to the prolonged gap between EBRT and intracavitary brachytherapy (ICBT).
Objectives
To evaluate local disease control and early complications of concomitant HDR-ICBT with EBRT and thereby decrease the OTT in I B–III B stage carcinoma cervix.
Methods
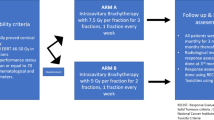
Fifty patients of carcinoma cervix (FIGO-I B/III B) were randomly divided into two groups: the study group treated with concomitant EBRT and HDR-ICBT (EBRT = 50–50.4 Gy/25–28 Fr, HDR 7 Gy in 3 Fr during the 3rd, 4th, and 5th weeks), EBRT and weekly cisplatin were not given on the day of HDR-ICBT; and the control group treated with EBRT followed by HDR-ICBT and weekly cisplatin. Acute reactions and local disease response were compared after treatment and at 6-month follow-up.
Results
Medians of OTTs were 42 and 63 days in the study and the control groups, respectively. Dysuria and diarrhoea incidences were more in the study but manageable. At the completion of the treatment, there were 92 and 80 % complete responses; 4 and 4 % partial responses; and 4 and 16 % stable diseases in the study group and the control group, respectively. DFSs (disease free survivals) at 6-month follow-up were, respectively, 96 and 84 %, and most of the stable diseases were observed in stage III B.
Conclusions
Response was better in the study group but statistically insignificant, acute reactions were manageable, and there was decrease in drop outs due to completion of treatment at a stretch, but larger number of patients and longer follow-up are required to arrive at concrete conclusions.









Similar content being viewed by others
References
Fowler JF. How worthwhile are short schedules in radiotherapy? A series of exploratory calculations. Radiother. Oncol. 1990;18(2):165–181. http://www.ncbi.nlm.nih.gov/pubmed/2367691.
Schmidt-Ullrich RK, Contessa JN, Dent P, et al. Molecular mechanisms of radiation-induced accelerated repopulation. Radiat. Oncol. Invest. 1999;7:321–330. http://www.ncbi.nlm.nih.gov/pubmed/10644055.
Fyles A, Keane TJ, Barton M, et al. The effect of treatment duration in the local control of cervix cancer. Radiother. Oncol. 1992;25:273–279. http://www.ncbi.nlm.nih.gov/pubmed/1480773.
Lanciano RM, Pajak TF, Martz K, et al. The influence of treatment time on outcome for squamous cell cancer of the uterine cervix treated with radiation: a patterns-of-care study. Int. J. Radiat. Oncol. Biol. Phys. 1993;25:391–397. http://www.ncbi.nlm.nih.gov/pubmed/8436516.
Girinsky T, Rey A, Roche B, et al. Overall treatment time in advanced cervical carcinomas: a critical parameter in treatment outcome. Int. J. Radiat. Oncol. Biol. Phys. 1993;27:1051–1056. http://www.ncbi.nlm.nih.gov/pubmed/8262826.
Perez CA, Grigsby PW, Castro-Vita H, et al. Carcinoma of the uterine cervix. Impact of prolongation of overall treatment time and timing of brachytherapy on outcome of radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 1995;32:1275–1288. http://www.ncbi.nlm.nih.gov/pubmed/7635767.
Delaloye JF, Coucke PA, Pampallona S, et al. Radiation therapy duration influences overall survival in patients with cervical carcinoma. Int. J. Gynecol. Obstet. 1997; 57(3): 295–303. http://www.ncbi.nlm.nih.gov/pubmed/9215493.
Mayer A, Nemeskéri C, Petneházi C, et al. Primary radiotherapy of stage IIA/B-IIIB cervical carcinoma. A comparison of continuous versus sequential regimens. Strahlenther. Onkol. 2004 Apr;180(4):209–215. http://www.ncbi.nlm.nih.gov/pubmed/15057431.
Petereit DG, Sarkaria JN, Chappell R, et al. The adverse effect of treatment prolongation in cervical carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 1995;32(5):1301–1307. http://www.ncbi.nlm.nih.gov/pubmed/7635769.
Patidar AK, Kumar HS, Walke RV, et al. Evaluation of the response of concurrent high dose rate intracavitary brachytherapy with external beam radiotherapy in management of early stage carcinoma cervix. J. Obstet. Gynecol. India. 2012;62(5):562–565
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pandu Ranga Kumari, M., Nagarjun Reddy, B., Sanjeeva Kumari, C. et al. Comparison Between Concurrent EBRT and ICA with Conventional EBRT Followed by ICA in Cervical Cancer. J Obstet Gynecol India 66, 263–273 (2016). https://doi.org/10.1007/s13224-014-0661-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-014-0661-x