Abstract
Type 2 diabetes (T2DM) is a polygenic metabolic disorder characterized by hyperglycemia occurring as a result of impaired insulin secretion or insulin resistance. Various environmental and genetic factors interact and increase the risk of T2DM and its complications. Among the various genetic factors associated with T2DM, single nucleotide polymorphism in different candidate genes have been studied intensively and the resulting genetic variants have been found to have either positive or negative association with T2DM thereby increasing or decreasing the risk of T2DM, respectively. In this review, we will focus on Guanine nucleotide-binding protein subunit beta 3 (GNB3), Norepinephrine Transporter (NET), Potassium Channel gene (KCNJ11), Transcription Factor 7-Like 2 (TCF7L2) and Glucocorticoid receptor (GRL) genes and their association with T2DM studied in different ethnic groups. The products of these genes are involved in the biochemical pathway leading to T2DM. Polymorphisms in these genes have been intensively studied in individuals of different ethnic origins. Results show that genetic variants of TCF7L2 and KCNJ11 genes have potential to emerge as a risk biomarker for T2DM whereas results of GNB3, GRL and NET genes have been controversial when studied in individuals of different ethnicities. We have tried to summarize the results generated globally in context to the selected genes which could possibly help researchers working in this field and would eventually help in understanding the mechanistic pathways of T2DM leading early diagnosis and prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a widely recognized major health issues affecting more than 170 million individuals worldwide. Among the different types of diabetes i.e., type 1 diabetes, type 2 diabetes and gestational diabetes, majority of diabetes cases (~90%) are of type 2 diabetes mellitus (T2DM). Increase in incidences of T2DM is becoming a major concern in developing countries and has emerged as an epidemic worldwide. It is predicted that by 2030 India will harbour 79.4 diabetics followed by China (42.3 million) and the United States (30.3 million) (Kaveeshwar and Cornwall 2014). It is characterized by hyperglycemia occurring as a result of impaired insulin secretion, insulin resistance and increased glucose output by liver or a combination of them (American Diabetes Association 2004). Long standing T2DM increases the risk of associated micro and macro vascular complications such as stroke, dyslipidemia, retinopathy, heart disease, stroke, peripheral neuropathy, nephropathy (Rizvi et al. 2014), blindness and amputation (Brownlee 2001). Various factors and their combined effects have been found to contribute to the development of T2DM such as environmental factors, obesity, lifestyle, family history, drugs, etc. Apart from these factors T2DM have a strong genetic component since it’s a polygenic disease with multiple genes interacting with one another along with other factors especially with various environmental factors contributing to disease susceptibility (Jenkins et al. 2013).
Over the past few decades variants in various candidate genes for T2DM such as KCNJ11 (Gloyn et al. 2003), TCF7L2 (Grant et al. 2006), PPAR-G (Altshuler et al. 2000), CAPN10 (Tsuchiya et al. 2006), GSTT1/M1 (Raza et al. 2014), FTO (Raza et al. 2014), PTPNI (Florez et al. 2005), etc. have been extensively studied and investigated through genetic linkage analysis and association studies to find their possible association with T2DM and declare them as susceptible genes. Most of the susceptibility genes were found to perform key regulatory functions in various pathways leading to glucose tolerance thus resulting in disease outcome (Lorenzo et al. 2013).
Identification of susceptibility genes is an important area of diabetes research since it help in finding genetic biomarkers which could help in early identification, treatment, and thus prevention of disease in susceptible individuals. Early identification and subsequent treatment strategies would also prevent the risk of developing the risk of secondary complication associated with T2DM in the susceptible individuals. However, these genetic biomarkers interact with various environmental and lifestyle factors to predispose an individual to T2DM risk. Since these environmental and lifestyle factors change with each ethnic group, a gene which shows association with T2DM in one ethnic group might show weak or no association in a different ethnic group. Thus, it is important to replicate the association studies and identify as well as characterize the gene variants related to T2DM in each ethnic group (Yamada et al. 2006).
Candidate and susceptibility genes for T2DM
The candidate gene approach in T2DM research helps in the identification of those genetic variants which are associated with disease outcome. Meta-analysis studies conducted worldwide on various candidate genes help in the determination of susceptibility genes for a particular disease. However, in case of a polygenic disease the results may not be conclusive since gene–gene interactions also play an important role since the contribution of a gene variant is more profound for a disease phenotype when it is the result of gene–gene interactions. A large number of candidate genes have been studied in the last two decades and enormous data is available from various association studies conducted on a global scale. In this review, we will focus on GNB3, NET, KCNJ11, TCF7L2 and GRL genes and their association with T2DM studied in different ethnic groups as shown in Table 1. The products of these genes are involved in the biochemical pathway leading to T2DM. Products of GNB3 gene regulate blood glucose levels through metabolic pathway of insulin signaling, while that of NET gene is involved in sodium–chloride dependent active reuptake of norepinephrine which in turn increases release of glucagon from pancreas thereby increasing blood glucose levels. KCNJ11 gene product was found to regulate insulin secretion; TCF7L2 is involved in survival and functioning of beta cells (Shu et al. 2008) and insulin secretion, while GRL plays role in beta cell function. Polymorphisms in these genes have been intensively studied in individuals of different ethnic origins. Results show that genetic variants of TCF7L2 and KCNJ11 genes have potential to emerge as a risk biomarker for T2DM, whereas results of GNB3, GRL and NET genes have been controversial when studied in individuals of different ethnicities.
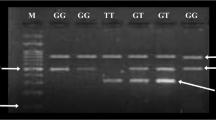
Guanine nucleotide-binding protein subunit beta 3 (GNB3) gene
G proteins also known as heterotrimeric guanine nucleotide-binding proteins are signaling molecules which are involved in regulating blood glucose levels through metabolic pathway of insulin signaling. They are also involved in the stimulation of secondary messengers such as adenylate cyclase, signaling pathways of epinephrine and glucagon receptors in hepatic, muscle and fat-tissue cells which are the pathophysiological signaling pathways leading to T2DM. These heterotrimeric protein molecules are made up of 3 subunits, alpha (α), beta (β) and gamma (γ) (Hurowitz et al. 2000). These G protein-coupled receptors activate a downstream secondary messenger cascade on binding ligand molecules such as hormones, neurotransmitters, chemokines, local mediators, etc. (Chandrasekaran et al. 2012). The GNB3 gene codes for the beta3 subunit of G proteins. Any change in the GNB3 gene due to any mutation or polymorphism may possibly lead to defects in the G protein encoded by the defective gene. These polymorphic changes have been found to be associated with the development of T2DM as well as its associated secondary complications. In this context, the most studied polymorphism of GNB3 gene is the C825T polymorphism. The 825T variant of GNB3 gene occurs when cytosine is replaced with thymine at position 825 in exon 10 in the wild-type gene due to alternative splicing leading to loss of 41 amino acids. The mutant 825T allele was associated with an increased production of Gβ3s (Andersen et al. 2006), resulting in enhanced signal transduction by G proteins. Studies found that the GNB3 C825T variant is a risk factor for hypertension, obesity, metabolic syndrome, atherosclerosis and diabetes (Siffert 2005). Various studies have confirmed the association of GNB3 polymorphism with T2DM in different populations. In Japanese population, multiple logistic regression analysis showed a significant association of the genotypes TT + TC with T2DM (Daimon et al. 2008). However, the results have been shown to be controversial in this population where another study on the same population found no significant association (Hayakawa et al. 2007). A study on Emirati and Canadian population found that 825T variant showed a positive association with T2DM risk (Kiani et al. 2005; Pollex et al. 2006). Numerous studies have showed a strong association of GNB3 polymorphism with the risk of diabetic neuropathy in different ethnic groups (Beige et al. 2000; Blüthner et al. 1999; Zychma et al. 2000). In contrast, some studies have also showed no association of GNB3 polymorphism with T2DM in Hispanic American (Parra et al. 2004), Danish (Andersen et al. 2006), Greek (Maniotis et al. 2014) and South Indian Populations (Chandrasekaran et al. 2012).
Norepinephrine transporter (NET) gene
The norepinephrine transporter (NET), also known as solute carrier family 6 member 2 (SLC6A2) (Pacholczyk et al. 1991). It is a 617 amino acid multipass monoamine symporter protein encoded by SLC6A2 gene present on chromosome 16 (Gelernter et al. 1993). It is involved in sodium–chloride dependent active reuptake of norepinephrine, a potent neurotransmitter, at neuronal junctions into the presynaptic nerve terminals. It helps in maintaining norepinephrine homeostasis in our body by regulating its metabolism and turnover rates. A potential decrease in norepinephrine uptake sites due to dysfunctional transporter had been observed in various cardiovascular diseases, such as hypertension, cardiomyopathy as well as in diabetes mellitus (Hahn and Blakely 2002). This could possibly occur as a result of various mutations and polymorphisms where a single nucleotide changes in the gene neither encoding nor epinephrine transporter may result in a non functional protein. A lot of studies have been conducted globally to find a potential relationship between single nucleotide polymorphism in NET gene and various diseases such as psychiatric disorders (Tellioglu and Robertson 2001), hyperactivity disorder (Kim et al. 2006), ADHD (Shannon et al. 2000; Neubauer and Christensen 1976) orthostatic intolerance (Tellioglu and Robertson 2001; Shannon et al. 2000) etc. Neubauer in 1976 first reported that norepinephrine concentration reduces considerably in the cardiovascular system of the diabetic patients but till date an insignificant amount of data is present to provide a potential evidence of the association of NET gene polymorphism with T2DM. The first ever study in this field was first carried out in 2006 on the G1287 single nucleotide polymorphism present in exon 9 of NET gene and T2DM in Caucasians where no significant association was found between this gene polymorphism and the risk of the development of T2DM and diabetic nephropathy (Ksiazek et al. 2006). However, it was observed that the AA genotype might contribute to the development of hypertension in these diabetic subjects. The frequency of AA genotype is reported to be higher in diabetic patients suffering from hypertension when compared with normotensive diabetic patients (19 vs. 10%, respectively, p < 0.05, OR = 2.21 with 95% CI 1.36–3.59) (Ksiazek et al. 2006). To the best of my knowledge this is the only study conducted so far between NET gene polymorphism and T2DM which calls for further association studies and testing of coding region variants of this gene and their functional assessment.
Potassium channel (KCNJ11) gene
The Potassium Channel gene also known as the Potassium inwardly rectifying channel, subfamily J, member 11 potassium channel gene and abbreviated as KCNJ11 belongs to potassium channel gene family. It is located at 11p15.1 on human chromosome and don’t have any intronic sequences (Haghvirdizadeh et al. 2015). This gene encodes a 390 amino acid protein which is an inward-rectifier potassium ion channel called Kir6.2. The Kir6.2 protein along with another protein SUR1 encoded by the ABCC8 gene located next to the KCNJ11 gene forms the KATP channel which modulates insulin production and secretion through glucose metabolism (McTaggart et al. 2010) and is the target of sulphonylurea drugs used for treating diabetes. Genetic polymorphism in KCNJ11 gene has been shown to be associated with an increased risk of T2DM. The KCNJ11 gene variant (Glu23Lys or E23K) where glutamic acid is replaced with lysine at 23rd position in the translated protein had been found to be a potential biomarker for T2DM (Qiu et al. 2014). This variant replaces the amino acid glutamic acid with the amino acid lysine at position 23 in the protein sequence, written as Glu23Lys or E23K. The lysine carrier having the variant gene were found to have reduced insulin secretion but were less likely to develop T2DM (Florez et al. 2007). A case control and a meta-analysis on Tunisian and Arab population case-also revealed significant association between KCNJ11 E23K variant and T2DM (Lasram et al. 2014). Recent study on Iranian subjects demonstrated that the carriers homozygous for KK genotype of KCNJ11 gene were susceptible to T2DM (p value = 0.049) and the frequency of K allele was higher in T2DM patients than control subjects (Rastegari et al. 2015). Another study on arab population showed significant association of the KCNJ11 E23K polymorphism with type 2 diabetes (Alsmadi et al. 2008a). A meta-analysis which included 48 published studies found a higher disease risk among Caucasians and East Asians carrying the lysine variant but no significant association was found with Indian and other ethnic populations (Qiu et al. 2014). Studies on Russian and Mauritanian populations also found an association between E23K variant and T2DM (Nikitin et al. 2015; Abdelhamid et al. 2014). However, apart from above mentioned studies a contrasting finding was observed in Iranian population where KCNJ11 E23K polymorphism is not associated with genetic susceptibility to T2DM but it was inferred that it might play a role in the progression of T2DM in obese subjects (Keshavarz et al. 2014). Similarly no significant association was observed in Moroccan population (Benrahma et al. 2014). Also, it was shown that patients carrying the lysine variant were more prone to secondary failure to sulphonylurea, T2DM treatment drug leading to higher fasting plasma glucose and glycosylated hemoglobin concentrations (Sesti et al. 2006).
Transcription factor 7-like 2 (TCF7L2) gene
Transcription factor 7-like 2 (TCF7L2) is a 215.9 kb gene located at 10q25 on human chromosome (Duval et al. 2000). TCF7L2 is a major component of Wnt signaling pathway, which is involved in various cellular growth and developmental processes. TCF7L2 regulates various pathways such as adipogenesis, development of pancreatic islet cells, survival and functioning of beta cells (Shu et al. 2008). It also plays a major role in insulin secretion by regulating various proteins involved in postprandial insulin secretion such as proglucagon and glucagon-like peptides GLP-1 and GLP-2 at transcriptional level (da Silva Xavier et al. 2009; Doria et al. 2008). TCF7L2 variants are regarded as the strongest genetic risk factors for T2DM, since it increase the disease risk 1.5-fold in heterozygotes and 2.4-fold in homozygotes, contributing to a 21% population risk (Grant et al. 2006). However, the TCF7L2 disease risk variants were found to vary among different populations (Guinan 2012). The most studied polymorphisms in TCF7L2 gene are rs7903146 of the intron 3 (IVS3C > T), rs7901695 of the intron 3 (IVS3T > C), rs12255372 of the intron 4 (IVS4G > T) and rs11196205 of the intron 4 (IVS4G > C). Polymorphism in TCF7L2 gene disrupts body glucose homeostasis by impairing insulin secretion, glucose turnover and glucose tolerance pathways by directly affecting pancreatic beta cells (Lyssenko et al. 2007; Schafer et al. 2007). In another study genetic polymorphism in TCF7L2 gene (rs7903146) was shown to predispose an individual to the risk of developing T2DM where the presence of TT genotype results in elevated plasma glucose, serum proinsulin and plasma gastric inhibitory polypeptide levels (Gjesing et al. 2011). TCF7L2 variants have been found to have a positive association with T2DM in French (Cauchi et al. 2006), African-American (Sale et al. 2007), Finnish (Scott et al. 2006), U. K. (Groves et al. 2006), Japanese (Miyake et al. 2008), Indian (Chandak et al. 2007) and Chinese (Chang et al. 2007) populations. Three TCF7L2 polymorphisms rs7903146, rs7901695 and rs12255372 were found to be associated with T2DM in Italian population and a strong correlation was found between rs7903146 and cardiovascular autonomic neuropathy in the study subjects (Cincia et al. 2012). In Kurdish population of Iran the T-allele of rs12255372, rs7903146, and rs290487 polymorphisms of TCF7L2 were found to be a risk allele for T2DM (Shokouhi et al. 2014). A large meta-analysis demonstrated significant association between IVS3C > T as well as IVS4G > T TCF7L2 gene polymorphisms and T2DM where among IVS3C > T polymorphism, TC heterozygotes and TT homozygous variants increased risk of T2MD by 1.4-fold and 2.0-fold, respectively, as compared to wild-type CC homozygotes whereas in case of IVS4G > T polymorphism, TG heterozygotes and TT homozygous variants increased risk of T2MD by 1.4-fold and 1.9-fold, respectively, as compared to wild-type GG homozygotes (Tong et al. 2009). In contrast, no significant association was found between TCF7L2 variants and T2DM among East Asians and conflicting results have appeared, in various studies on Chinese population (Chang et al. 2007; Ng et al. 2007). In Arabs, weak or no association was observed in two polymorphisms of TCF7L2 gene (rs12255372, rs7903146) with T2DM (Alsmadi et al. 2008b).
Glucocorticoid receptor (GRL) gene
The glucocorticoid receptor gene (GRL) also known as NR3C1 (nuclear receptor subfamily 3, group C, member 1) gene, is located on chromosome number 5 at 5q31 position in humans. (Marti et al. 2006) It encodes a 777-amino acid (Glucocorticoid receptor α) or a 742-amino acid (Glucocorticoid receptor β) polypeptide which acts as a receptor for cortisol and glucocorticoids and regulates gene expression of various genes involved in cell development, metabolism and immune responses. The 363S allele of the N363S variant present in exon 2 of GRL gene was found to be associated with the risk of weight gain/obesity but no evidence was found for an association of this variant with parameters related to hyperglycaemia in French Caucasians with T2DM (Roussel et al. 2003). In another study on Swedish men, significant increase in fasting glucose and insulin were found over the 5-year follow-up among individuals homozygotes for the BclI allele of GRL gene whereas no significant associations were found with Tth111I or A/G polymorphism of GRL gene with T2DM (Rosmond and Holm 2008). Similar results were reported in Italian subjects with Addison’s disease where patients carrying GG genotype of BclI polymorphism showed higher glucose levels or glucose intolerance as compared to individuals carrying wild-type CC and heterozygous CG genotype (Giordano et al. 2012). Another study on British Caucasian obese women showed that Bc1I polymorphism was significantly associated with higher fasting insulin and index of insulin resistance (HOMA) (weaver et al. 1992). In a different study on Italian patients with Cushing’s syndrome the A3669G polymorphism of GRL gene was seen to have a protective role where it was found to decrease the risk of developing T2DM (Trementino et al. 2012). In a cross-sectional cohort study on N363S (rs6195), BclI (rs41423247), ER22/23EK (rs6189/6190), 9b A/G (rs6198) and ThtIIII (rs10052957) polymorphisms in KCNJ11 gene, none of the polymorphisms studied was found to be associated with insulin sensitivity, however, N363S and ER22/23EK polymorphisms of the GRL gene were found to be negatively associated with β-cell function in women, but not in men (van Raalte et al. 2012).
Conclusion
The incidence of diabetes occurrence is increasing at a fast pace globally and present data demonstrate that its prevalence is also increasing among children and adolescents who are below 30 years of age. This calls for an urgent development of techniques and methods to combat this growing epidemic and to identify high-risk individuals at an early stage that could thus be prevented from T2DM by taking suitable preventive measures. Apart from environmental factors such as diet, ethnicity, family history, lifestyle, etc., genetic factors also have a profound effect on the occurrence of T2DM and they interact with the environmental factors in predisposing an individual to T2DM. Thus, a susceptible gene in one population might not show the same phenotypic effect in other population. Various genetic linkage and associations studies have identified several candidate genes for T2DM and ongoing studies on in this field are focusing on identifying novel gene variants which are having a potential role in the pathophysiology of T2DM. This review had summarized the results from various global studies on the association of GNB3, NET, KCNJ11, TCF7L2 and GRL genes with T2DM which could possibly help researchers working in this field and would eventually help in understanding the mechanistic pathways of T2DM. Results show that genetic variants of TCF7L2 and KCNJ11 genes have potential to emerge as a risk biomarker for T2DM whereas polymorphisms in GNB3, GRL and NET genes may confer smaller or modifier effects since the results have been controversial and will require further larger studies to fully elucidate their role in T2DM. Thus, we could say that a proper understanding of genetic background of T2DM will help in understanding the biochemical and molecular mechanisms, developing potential biomarkers which could identify at-risk patients in early stages and designing new therapeutics which will thus help in diagnostics, treatment and eventually prevention of this disease.
References
Abdelhamid I, Lasram K, Meiloud G, Ben Halim N, Kefi R, Samb A et al (2014) E23K variant in KCNJ11 gene is associated with susceptibility to type 2 diabetes in the Mauritanian population. Prim Care Diabet 8(2):171–175. doi:10.1016/j.pcd.2013.10.006
Alsmadi O, Al-Rubeaan K, Mohamed G, Alkayal F, Al-Saud H, Al-Saud NA et al (2008a) Weak or no association of TCF7L2 variants with type 2 diabetes risk in an Arab population. BMC Med Genet 9:72
Alsmadi O, Al-Rubeaan K, Wakil SM, Imtiaz F, Mohamed G, Al-Saud H et al (2008b) Genetic study of Saudi diabetes (GSSD): significant association of the KCNJ11 E23K polymorphism with type 2 diabetes. Diabet Metab Res Rev 24(2):137–140
Altshuler D, Hirschhorn JN, Klannemark M, Lindgrea CM, Vohl MC, Nemesh J et al (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80
American Diabetes Association (2004) Diagnosis and classification of diabetes mellitus. Diabet Care 1:S5–S10
Amoli MM, Amiri P, Tavakkoly-Bazzaz J, Charmchi E, Hafeziyeh J et al (2010) Replication of TCF7L2 rs7903146 association with type 2 diabetes in an Iranian population. Genet Mol Biol 33:449–451. doi:10.1590/s1415-47572010005000056
Andersen G, Overgaard J, Albrechtsen A, Glümer C, Borch-Johnsen K, Jørgensen T et al (2006) Studies of the association of the GNB3 825C> T polymorphism with components of the metabolic syndrome in white Danes. Diabetologia 49(1):75–82
Beige J, Ringel J, Distler A et al (2000) G-protein β3-subunit C825T genotype and nephropathy in diabetes mellitus. Nephrol Dial Transplant 15:1384–1387
Benrahma H, Charoute H, Lasram K, Boulouiz R, Atig RK, Fakiri M et al (2014) Association Analysis of IGF2BP2, KCNJ11, and CDKAL1 Polymorphisms with Type 2 Diabetes Mellitus in a Moroccan Population: A Case–Control Study and Meta-analysis. Biochem Genet 52(9–10):430–442. doi:10.1007/s10528-014-9658-5
Blüthner M, Schmidt S, Siffert W et al (1999) Increased frequency of G-protein β3-subunit 825 T allele in dialyzed patients with type 2 diabetes. Kidney Int 55:1247–1250
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Cauchi S, Meyre D, Dina C, Choquet H, Samson C, Gallina S et al (2006) Transcription factor TCF7L2 genetic study in the French population: expression in human beta-cells and adipose tissue and strong association with type 2 diabetes. Diabetes 55(10):2903–2908
Cauchi S, El Achhab Y, Choquet H, Dina C, Krempler F, Weitgasser R et al (2007) TCF7L2 is reproducibly associated with type 2 diabetes in various ethnic groups: a global meta-analysis. J Mol Med (Berl) 85(7):777–782
Chandak GR, Janipalli CS, Bhaskar S, Kulkarni SR, Mohankrishna P et al (2007) Common variants in the TCF7L2 gene are strongly associated with type 2 diabetes mellitus in the Indian population. Diabetologia 50:63–67. doi:10.1007/s00125-006-0502-2
Chandrasekaran S, Sivani S, Sudarsanam S (2012) Evaluation of single nucleotide polymorphism C825T in the GNB3 gene with the development of type 2 diabetes of the South Indian population. Int J Pharma Sci Res 3(1):249–325
Chang YC, Chang TJ, Jiang YD et al (2007) Association study of the genetic polymorphisms of the transcription factor 7-like 2 (TCF7L2) gene and type 2 diabetes in the Chinese population. Diabetes 56(10):2631–2637
Chavali S, Mahajan A, Tabassum R et al (2011) Association of variants in genes involved in pancreatic β-cell development and function with type 2 diabetes in North Indians. J Hum Genet 56(10):695–700
Cincia C, Fusco DD, Cacciotti L, Morganti R, D’Amato C, Novelli G et al (2012) TCF7L2 gene polymorphisms and type 2 diabetes: association with diabetic retinopathy and cardiovascular autonomic neuropathy. Acta Diabetol 50(5):789–799. doi:10.1007/s00592-012-0418-x
da Silva Xavier G, Loder MK, McDonald A, Tarasov AI, Carzaniga R, Kronenberger K (2009) TCF7L2 regulates late events in insulin secretion from pancreatic islet beta-cells. Diabetes 58(4):894–905
Daimon M, Sato H, Sasaki S, Toriyama S, Emi M, Muramatsu M et al (2008) Salt consumption-dependent association of the GNB3 gene polymorphism with type 2 DM. Biochem Biophys Res Commun 374(3):576–580. doi:10.1016/j.bbrc.2008.07.065
Damcott CM, Pollin TI, Reinhard LJ, Ott SH, Shen H et al (2006) Polymorphisms in the transcription factor 7-like 2 (TCF7L2) gene are associated with type 2 diabetes in the Amish: replication and evidence for a role in both insulin secretion and insulin resistance. Diabetes 55:2654–2659. doi:10.2337/db06-0338
Doria A, Patti ME, Kahn CR (2008) The emerging genetic architecture of type 2 diabetes. Cell Metab 8(3):186–200
Duval A, Busson-Leconiat M, Berger R, Hamelin R (2000) Assignment of the TCF-4 gene (TCF7L2) to human chromosome band 10q25.3. Cytogenet Cell Genet 88:264–265. doi:10.1159/000015534
Florez JC, Agapakis CM, Burtt NP, Sun M, Almgren P, Rastam L et al (2005) Association testing of the protein tyrosine phosphatase 1B gene (PTPN1) with type 2 diabetes in 7,883 people. Diabetes 54:1884–1891
Florez JC, Jablonski KA, Kahn SE, Franks PW, Dabelea D, Hamman RF et al (2007) Type 2 diabetes–associated missense polymorphisms KCNJ11 E23K and ABCC8 A1369S influence progression to diabetes and response to interventions in the diabetes prevention program. Diabetes 56(2):531–536. doi:10.2337/db06-0966
Gelernter J, Kruger S, Pakstis AJ, Pacholczyk T, Sparkes RS, Kidd KK et al (1993) Assignment of the norepinephrine transporter protein (NET1) locus to chromosome 16. Genomics 18:690–692
Giordano R, Marzotti S, Berardelli R, Karamouzis I, Brozzetti A, D’Angelo V et al (2012) BClI polymorphism of the glucocorticoid receptor gene is associated with increased obesity, impaired glucose metabolism and dyslipidaemia in patients with Addison’s disease. Clin Endocrinol (Oxf) 77(6):863–870. doi:10.1111/j.1365-2265.2012.04439.x
Gjesing AP, Kjems LL, Vestmar MA, Grarup N, Linneberg A, Deacon CF (2011) Carriers of the TCF7L2 rs7903146 TT genotype have elevated levels of plasma glucose, serum proinsulin and plasma gastric inhibitory polypeptide (GIP) during a meal test. Diabetologia 54(1):103–110
Gloyn AL, Weedon MN, Owen KR, Turner MJ, Knight BA, Hitman G et al (2003) Large scale association studies of variants in genes encoding the pancreatic beta-cell K-ATP channel subunits Kir6.2 (KCNJ11) and SUR1 (ABCC8) confirm that the KCNJ11 E23K variant is associated with type 2 diabetes. Diabetes 52:568–572
Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J et al (2006) Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 38:320–323
Groves CJ, Zeggini E, Minton J et al (2006) Association analysis of 6,736 U.K. subjects provides replication and confirms TCF7L2 as a type 2 diabetes susceptibility gene with a substantial effect on individual risk. Diabetes 55(9):2640–2644
Guinan KJ (2012) Worldwide distribution of type II diabetes-associated TCF7L2 SNPs: evidence for stratification in Europe. Biochem Genet 50(3–4):159–179. doi:10.1007/s10528-011-9456-2
Haghvirdizadeh P, Mohamed Z, Abdullah NA, Haghvirdizadeh P, Haerian MS, Haerian BS (2015) KCNJ11: genetic polymorphisms and risk of diabetes mellitus. J Diabet Res 908152:9
Hahn MK, Blakely RD (2002) Monoamine transporter gene structure and polymorphisms in relation to psychiatric and other complex disorders. Pharmacogenom J 2:217–235
Hayakawa T, Takamura T, Abe T et al (2007) Association of the C825T polymorphism of the G-protein beta3 subunit gene with hypertension, obesity, hyperlipidemia, insulin resistance, diabetes, diabetic complications and diabetic therapies among Japanese. Metabolism 56(1):44–48
Hayashi T, Iwamoto Y, Kaku K, Hirose H, Maeda S (2007) Replication study for the association of TCF7L2 with susceptibility to type 2 diabetes in a Japanese population. Diabetologia 50:980–984. doi:10.1007/s00125-007-0618-z
Hurowitz EH, Melnyk JM, Chen YJ, Kouros-Mehr H, Simon MI, Shizuya H et al (2000) Genomic characterization of the human heterotrimeric G protein alpha, beta, and gamma subunit genes. DNA Res 7(2):111–120
Jenkins AB, Batterham M, Samocha-Bonet D, Tonks K, Greenfield JR, Campbell LV (2013) Segregation of a latent high adiposity phenotype in families with a history of type 2 diabetes mellitus implicates rare obesity-susceptibility genetic variants with large effects in diabetes-related obesity. PLoS One 8:e70435
Jyothi KU, Jayaraj M, Subburaj KS, Prasad KJ, Kumuda I, Lakshmi V (2013) Association of TCF7L2 Gene Polymorphisms with T2DM in the Population of Hyderabad, India. PLoS One 8(4):e60212
Kaveeshwar SA, Cornwall J (2014) The current state of diabetes mellitus in India. Aust Med J 7(1):45–48
Keshavarz P, Habibipour R, Ghasemi M, Kazemnezhad E, Alizadeh M, Omami MH (2014) Lack of genetic susceptibility of KCNJ11 E23 K polymorphism with risk of type 2 diabetes in an Iranian population. Endocr Res 39(3):120–125. doi:10.3109/07435800.2013.860607
Kiani JG, Saeed M, Parvez SH, Frossard PM (2005) Association of G-protein beta-3 subunit gene (GNB3) T825 allele with Type II diabetes. Neuroendocrinol Lett 26(2):87–88
Kim CH, Hahn MK, Joung Y, Anderson SL, Steele AH, Mazei-Robinson MS et al (2006) A polymorphism in the norepinephrine transporter gene alters promoter activity and is associated with attention-deficit hyperactivity disorder. Proc Natl Acad Sci USA 103(50):19164–19169
Koo BK, Cho YM, Park BL et al (2007) Polymorphisms of KCNJ11 (Kir6.2 gene) are associated with type 2 diabetes and hypertension in the Korean population. Diabet Med 24(2):178–186
Ksiazek P, Buraczynska K, Buraczynska M (2006) Norepinephrine transporter gene (NET) polymorphism in patients with type 2 diabetes. Kidney Blood Press Res 29:338–343. doi:10.1159/000097356
Lasram K, Ben Halim N, Hsouna S, Kefi R, Arfa I, Ghazouani W et al (2014) Evidence for Association of the E23K Variant of KCNJ11 Gene with Type 2 Diabetes in Tunisian Population: Population-Based Study and Meta-Analysis. Biomed Res Int 2014:265–274. doi:10.1155/2014/265274
Liu Z, Zhang YW, Feng QP et al (2006) Association analysis of 30 type 2 diabetes candidate genes in Chinese Han population. Acta Acad Med Sin 28(2):124–128
Lorenzo C, Greco A, Fiorentino TV, Mannino GC, Hribal ML (2013) Variants of insulin-signaling inhibitor genes in type 2 diabetes and related metabolic abnormalities. Int J Genom 376454:1–13. doi:10.1155/2013/376454
Lyssenko V, Lupi R, Marchetti P et al (2007) Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 117(8):2155–2163
Maniotis C, Chantziara K, Kokkoris P, Papadogiannis D, Andreou C, Tsioufis C et al (2014) The AGT and the GNB3 polymorphisms and insulin resistance in prehypertension. Hormones (Athens) 13(1):79–86
Marquezine GF, Pereira AC, Sousa AG, Mill JG, Hueb WA et al (2008) TCF7L2 variant genotypes and type 2 diabetes risk in Brazil: significant association, but not a significant tool for risk stratification in the general population. BMC Med Genet 9:106. doi:10.1186/1471-2350-9-106
Marti A, Ochoa MC, Sanchez-Villegas A, Martinez JA, Martinez-Gonzalez MA, Hebebrand J, Hinney A, Vedder H (2006) Meta-analysis on the effect of the N363S polymorphism of the glucocorticoid receptor gene (GRL) on human obesity. BMC Med Genet 7:50
McTaggart JS, Clark RH, Ashcroft FM (2010) The role of the KATP channel in glucose homeostasis in health and disease: more than meets the islet. J Physiol 588(17):3201–3209
Miyake K, Horikawa Y, Hara K et al (2008) Association of TCF7L2 polymorphisms with susceptibility to type 2 diabetes in 4,087 Japanese subjects. J Hum Genet 53(2):174–180
Nanfa D, Sobngwi E, Atogho-Tiedeu B, Noubiap JJ, Donfack OS, Mofo EP et al (2015) Association between the TCF7L2 rs12255372 (G/T) gene polymorphism and type 2 diabetes mellitus in a Cameroonian population: a pilot study. Clin Transl Med 4:17
Neubauer B, Christensen NJ (1976) Norepinephrine, epinephrine, and dopamine contents of the cardiovascular system in long-term diabetics. Diabetes 25(1):6–10
Ng MC, Tam CHT, Lam VK, So WY, Ma RC et al (2007) Replication and identification of novel variants at TCF7L2 associated with type 2 diabetes in Hong Kong Chinese. J Clin Endocrinol Metab 92:3733–3737. doi:10.1210/jc.2007-0849
Nikitin AG, Potapov VA, Brovkin AN, Lavrikova EIu, Hodyrev DS, Shamkhalova MSh et al (2015) Association of the polymorphisms of the FTO, KCNJ11, SLC30A8 and CDKN2B genes with type 2 diabetes. Mol Biol (Mosk) 49(1):119–128
Pacholczyk T, Blakely RD, Amara SG (1991) Expression cloning of a cocaine- and antidepressant-sensitive human noradrenaline transporter. Nature 350(6316):350–354
Parra EJ, Hoggart CJ, Bonilla C, Dios S, Norris JM, Marshall JA, Hamman RF et al (2004) Relation of type 2 diabetes to individual admixture and candidate gene polymorphisms in the Hispanic American population of San Luis Valley, Colorado. J Med Genet 41:1–9
Pemberton TJ, Mehta NU, Witonsky D, Di RA, Allayee H et al (2008) Prevalence of common disease-associated variants in Asian Indians. BMC Genet 9:13
Pollex RL, Hanley AJ, Zinman B, Harris SB, Khan HM, Hegele RA (2006) Metabolic syndrome in aboriginal Canadians: prevalence and genetic associations. Atherosclerosis 184:121–129
Qiu L, Na R, Xu R, Wang S, Sheng H et al (2014) Quantitative assessment of the effect of KCNJ11 gene polymorphism on the risk of type 2 diabetes. PLoS One 9(4):e93961. doi:10.1371/journal.pone.0093961
Rastegari A, Rabbani M, Sadeghi HM, Imani EF, Hasanzadeh A, Moazen F (2015) Association of KCNJ11 (E23K) gene polymorphism with susceptibility to type 2 diabetes in Iranian patients. Adv Biomed Res 4:1
Raza ST, Abbas S, Ahmad A, Ahmed F, Zaidi ZH, Mahdi F (2014) Association of glutathione-S-transferase (GSTM1 and GSTT1) and FTO gene polymorphisms with type 2 diabetes mellitus cases in Northern India. Balkan J Med Genet 17(1):47–54
Rizvi S, Raza ST, Mahdi F (2014) Association of genetic variants with diabetic nephropathy. World J Diabet 5(6):809–816
Rosmond R, Holm GJ (2008) A 5-year follow-up study of 3 polymorphisms in the human glucocorticoid receptor gene in relation to obesity, hypertension, and diabetes. Cardiometab Syndr 3(3):132–135. doi:10.1111/j.1559-4572.2008.00008.x
Roussel R, Reis AF, Dubois-Laforgue D, Bellanné-Chantelot C, Timsit J, Velho G (2003) The N363S polymorphism in the glucocorticoid receptor gene is associated with overweight in subjects with type 2 diabetes mellitus. Clin Endocrinol (Oxf) 59(2):237–241
Sakamoto Y, Inoue H, Keshavarz P et al (2007) SNPs in the KCNJ11-ABCC8 gene locus are associated with type 2 diabetes and blood pressure levels in the Japanese population. J Hum Genet 52(10):781–793
Sale MM, Smith SG, Mychaleckyj JC et al (2007) Variants of the transcription factor 7-like 2 (TCF7L2) gene are associated with type 2 diabetes in an African-American population enriched for nephropathy. Diabetes 56(10):2638–2642
Schafer SA, Tschritter O, Machicao F et al (2007) Impaired glucagon-like peptide-1-induced insulin secretion in carriers of transcription factor 7-like 2 (TCF7L2) gene polymorphisms. Diabetologia 50(12):2443–2450
Scott LJ, Bonnycastle C, Willer CJ, Sprau AG, Jackson AU et al (2006) Association of transcription factor 7-like 2 (TCF7L2) variants with type 2 diabetes in a Finnish sample. Diabetes 55:2649–2653. doi:10.2337/db06-0341
Sesti G, Laratta E, Cardellini M, Andreozzi F, Del Guerra S, Irace C et al (2006) The E23K variant of KCNJ11 encoding the pancreatic beta-cell adenosine 5′-triphosphate-sensitive potassium channel subunit Kir6.2 is associated with an increased risk of secondary failure to sulfonylurea in patients with type 2 diabetes. J Clin Endocrinol Metab 91:2334–2339
Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I et al (2000) Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med 342(8):541–549
Shokouhi S, Delpisheh A, Haghani K, Mahdizadeh M, Bakhtiyari S (2014) Association of rs7903146, rs12255372, and rs290487 polymorphisms in TCF7L2 gene with type 2 diabetes in an Iranian Kurdish ethnic group. Clin Lab 60(8):1269–1276
Shu L, Sauter NS, Schulthess FT, Matveyenko AV, Oberholzer J, Maedler K (2008) Transcription factor 7-like 2 regulates beta-cell survival and function in human pancreatic islets. Diabetes 57(3):645–653
Siffert W (2005) G protein polymorphisms in hypertension, atherosclerosis, and diabetes. Annu Rev Med 56:17–28
Tellioglu T, Robertson D (2001) Genetic or acquired deficits in the norepinephrine transporter: current understanding of clinical implications. Expert Rev Mol Med 29:1–10
Tong Y, Lin Y, Zhang L, Yang J, Zhang Y, Liu H et al (2009) Association between TCF7L2 gene polymorphisms and susceptibility to Type 2 Diabetes Mellitus: a large Human Genome Epidemiology (HuGE) review and meta-analysis. BMC Med Genet 10:15. doi:10.1186/1471-2350-10-15
Trementino L, Appolloni G, Concettoni C, Cardinaletti M, Boscaro M, Arnaldi G (2012) Association of glucocorticoid receptor polymorphism A3669G with decreased risk of developing diabetes in patients with Cushing’s syndrome. Eur J Endocrinol 166:35–42
Tsuchiya T, Schwarz PE, Bosque-Plata LD, Hayes MG, Dina C, Froguel P et al (2006) Association of the calpain-10 gene with type 2 diabetes in Europeans: results of pooled and meta-analyses. Mol Genet Metab 89:174–184
van Raalte DH, van Leeuwen N, Simonis-Bik AM, Nijpels G, van Haeften TW, Schafer SA et al (2012) Glucocorticoid receptor gene polymorphisms are associated with reduced first-phase glucose-stimulated insulin secretion and disposition index in women, but not in men. Diabet Med 29(8):e211–e216. doi:10.1111/j.1464-5491.2012.03690.x
van Vliet-Ostaptchouk JV, Shiri-Sverdlov R, Zhernakova A, Strengman E, van Haeften TW et al (2007) Association of variants of transcription factor 7-like 2 (TCF7L2) with susceptibility to type 2 diabetes in the Dutch Breda cohort. Diabetologia 50:59–62. doi:10.1007/s00125-006-0477-z
Wang J, Zhang J, Li L, Wang Y, Wang Q, Zhai Y et al (2013) Association of rs12255372 in the TCF7L2 gene with type 2 diabetes mellitus: a meta-analysis. Braz J Med Biol Res 46(4):382–393
Weaver JU, Hitman GA, Kopelman PG (1992) An association between a Bc1I restriction fragment length polymorphism of the glucocorticoid receptor locus and hyperinsulinaemia in obese women. J Mol Endocrinol 9(3):295–300
Yamada Y, Matsuo H, Segawa T, Watanabe S, Kato K, Kameyama T et al (2006) Assessment of genetic factors for type 2 diabetes mellitus. Int J Mol Med 18:299–308
Zhai Y, Zhao J, You H, Pang C, Yin L, Guo T (2014) Association of the rs11196218 polymorphism in TCF7L2 with type 2 diabetes mellitus in Asian population. Meta Gene 2:332–341
Zhang C, Qi L, Hunter DJ, Meigs JB, Manson JE et al (2006) Variant of transcription factor 7-like 2 (TCF7L2) gene and the risk of type 2 diabetes in large cohorts of U.S. women and men. Diabetes 55:2645–2648. doi:10.2337/db06-0643
Zhou D, Zhang D, Liu Y et al (2009) The E23K variation in the KCNJ11 gene is associated with type 2 diabetes in Chinese and East Asian population. J Hum Genet 54(7):433–435
Zychma MJ, Zukowska-Szczechowska E, Ossowska-Szymkowicz I et al (2000) G-protein β3 subunit C825T variant, nephropathy and hypertension in patients with type 2 (non-insulin-dependent) diabetes mellitus. Am J Nephrol 20:305–310
Acknowledgements
We are thankful for the support received from Era’s Lucknow Medical College and Hospital, Lucknow, Uttar Pradesh, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rizvi, S., Raza, S.T., Rahman, Q. et al. Role of GNB3, NET, KCNJ11, TCF7L2 and GRL genes single nucleotide polymorphism in the risk prediction of type 2 diabetes mellitus. 3 Biotech 6, 255 (2016). https://doi.org/10.1007/s13205-016-0572-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13205-016-0572-x