Abstract
Drinking water quality and its public health effect are ignored in urban slum households of Ethiopia. The aim of this study was to assess physicochemical and microbial quality of drinking water stored in slum households of Hawassa City, Ethiopia. Cross-sectional study was conducted and a total of 120 water samples were collected from 60 households (60 tap, 60 households) to test the quality. Wagtech Potalab + PTW − 1000 was used to test the parameters. Physicochemical parameters—temperature, turbidity, pH and residual free chlorine were measured. Presence of total and faecal coliform bacteria was tested using the Wagtech membrane filtration procedure. Heads of the households were asked about the case of diarrhoeal diseases in any of their family members. Data were statistically analysed and compared with World Health Organization (WHO) standards. Paired t test was used to analyse the mean difference between tap and household water samples. Binary logistic regression was used to investigate any significant association between presence of faecal coliform in the water samples and occurrence of diarrhoeal diseases. Eight (13.3%) tap and 28 (46.7%) household water samples were found positive for total coliform; five (8.3%) tap and 19 (31.7%) household water samples were positive for faecal coliform. Eleven (18.3%) household water samples had faecal coliform 10–100 CFU/100 ml, which falls under high-risk category based on WHO standard. The paired t test (p < 0.05) showed significant mean difference between faecal coliform count of the tap and household water samples. The binary logistic regression analysis implied the odds for occurrence of diarrhoeal disease is 17.33 more in households with positive faecal coliform results (p < 0.05). It is concluded that there was a significant level of faecal contamination of drinking water at the household level. Therefore, it is recommended that continuous health education on drinking water handling should be given to slum households.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Access to safe drinking water is a basic human right. Besides its aesthetic appearance, water intended for human consumption should not contain chemical contaminants and any microorganisms and parasites in such a level that could be harmful to human health. It is clear that quality is the most important and the primary indicator for drinking water safety due to its major public health implications (WHO 2021; Mohammed and Abdulrazzaq 2018). The UN Sustainable Development Goal (SDG) 6.1 aspires to achieve universal and equitable access to safe and affordable drinking water for all by 2030 (UN 2016). In order to achieve this goal, countries are striving to ensure sufficient (in terms of quantity, quality, accessibility and affordability) drinking water supply (UN 2020). In this regard, most countries develop their own regulation and standards for drinking water supply by adopting the WHO’s International Guidelines for Drinking-water Quality (GDWQ) (WHO 2021).
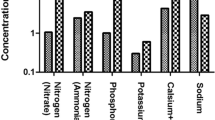
Drinking water qualities are commonly addressed based on the physicochemical, radiological and microbial characteristics of the water and usually compared to national and international standards (WHO 2021; Mohammed and Abdulrazzaq 2018). Acceptability, taste, odour and appearance of drinking water are determined from consumers preferences. Parameters including colour, taste, odour, temperature, pH, turbidity, water hardness, sodium, calcium and total dissolved solids are common parameters used to address acceptability of drinking water by consumers. Chemical (inorganic and organic) parameters are also used to investigate safety of drinking water. Inorganic chemicals like arsenic, cadmium, lead, chromium, mercury, chlorine, cyanide and fluoride and organic compounds like pesticides, chloroform and carbon tetrachloride are used to investigate chemical characteristics of drinking water. Parameters including bacterial, viral, protozoan and helminth pathogens are used to identify microbiological characteristics of drinking water (WHO 2021, 2011). Total and faecal coliform bacteria and enterococci (faecal streptococci) are the most widely used indicator organisms to determine microbial quality of drinking water. Faecal coliform and faecal streptococci are important indicators of faecal contamination of water. They are widely used in most developing countries since most water contaminations are caused from poor sanitation and hygienic practices (Gizachew et al. 2020; Mohammed and Abdulrazzaq 2018; Sitotaw and Geremew 2021).
In most of the developing countries, lack of access to safe drinking water is a major problem. Millions of people are still suffering from communicable diseases due to the use of unsafe drinking water and poor sanitation (Wolde et al. 2020). In Ethiopia, over 60% of communicable diseases are due to poor environmental health conditions arising from lack of safe and adequate water supply (Abera et al. 2011). In recent years, the country’s domestic water supply from any improved water sources reached 64.8%. However, diarrhoea prevalence is highest among children residing in households that drink from unprotected wells (18%), rural areas (14%) and urban areas (CSA and ICF 2016).
In some parts of Ethiopia, drinking water quality studies were conducted by sampling different water supply sources and water from taps of the end-users. Most of the findings indicated that microbial and physicochemical characteristics of the waters were poor and below national and international water quality standards(Kassegne and Leta 2020; Gizachew et al. 2020; Werkneh et al. 2015; Yasin et al. 2015a; Sitotaw and Geremew 2021; Duressa et al. 2019; Sitotaw et al. 2021).
Lack of access to safe drinking water is more severe in urban slum areas and occurrence of communicable diseases including diarrhoea is more prevalent. In most urban slum areas of the developing countries, shortage and interruption of safe water supply as well as poor hygienic practices and lack of sanitation facilities are their common characteristics (Handam et al. 2020, Satapathy 2014, Li and Wu 2019, WHO 2019). It is also the reality of most slum households of Ethiopia. Studies also indicated that households’ poor drinking water handling and storage practices caused microbial contamination of water(Slavik et al. 2020; Girmay et al. 2021; Sharma et al. 2013). In this regard, it is recommended to inspect drinking water delivery systems from source to mouth and “handling of water at home” is one element. With all this however, little was studied about water quality issues of urban slum households, especially in Ethiopia.
Therefore, this study aimed to investigate microbial and physicochemical quality of tap water and drinking water stored at slum households.
Materials and methods
Study period and area
This study was conducted in May 2016 in Hawassa City, Ethiopia. Hawassa is the capital city of the Southern Nations Nationalities and Peoples Regional State (SNNPRS) located 275 km south of the country’s capital city—Addis Ababa. Based on the 2007 Census conducted by the Central Statistical Agency of Ethiopia, the city has a total population of 157,879. The city administration has eight subcities where some of the subcities are known for the presence of overcrowded households and substandard housings.
Study design
A cross-sectional study was used to determine physicochemical and microbial quality of drinking water taken from tap and stored at household level. Laboratory tests were conducted to investigate physicochemical and microbial quality parameters of the water samples collected from the households.
Sample size determination
First, sample size was calculated using single population proportion (SPP)formula \(N = \frac{{Z^{2} P\left( {1 - P} \right)}}{{d^{2} }}\) where N = sample size, P = proportion, d = margin of error and Z value of 1.96 is used at 95% CI and margin of error is 5%. Considering poor hygienic practices and lack of sanitation facilities in urban slum areas, it is assumed that 50% of households’ water is unsafe for drinking. Taking 50% as a proportion (p), the determined size became 385. Then, 15% of the determined sample size was taken as representative sampling points for water sample collection. As basic assumption that water quality may not vary at a nearby distance (WHO 2006), \({\text{Number}}\; {\text{of}}\;{\text{ sampling}}\;{\text{ point}}\,s = Nx15\%\), where N = sample size determined using SPP. Number of households became 57.75. Considering 4% non-response rate, the final number of households became 60. From each household, water samples were collected from tap and drinking water storing containers. A total of 120 water samples were collected for physicochemical and bacteriological tests.
Water sample collection and processing
Systematic random sampling technique was applied to select households. Water samples were collected according to the standard procedure stated in WHO drinking water guideline (WHO 2004). For each water sample, 500 ml was collected using sterile bottles and immediately transported to the SNNPRs regional public health laboratory with an ice box. The temperature, pH and turbidity of the water samples were measured at the spot of sample collection. Wagtech Potalab + PTW − 1000 was used to test the water quality parameters. Residual free chlorine was determined using Wagtech comparator-disc with DPD number 1 chlorine tablet. Wagtech membrane filtration was used to conduct bacteriological tests according to the recommended standard procedures. A 100 ml of the water sample was filtered using membrane filter (0.45 µm pore size). The membrane filter was incubated at 37 °C using Membrane Lauryl Sulphate Broth (MLSB) media for 18 h. After 18 h, colonies of total coliform bacteria were counted. The membrane was incubated at 44.5 °C for 18 h in order to detect presence of faecal coliform bacteria. Heads of the households were also asked for the occurrence of diarrhoeal diseases within the previous two weeks prior to sample collection.
Data analysis
Data were analysed using SPSS statistical software (version 23). Results obtained for the measured physicochemical parameters and bacteria counts were compared with national and international (WHO) drinking water quality standards. Paired t test was used to analyse if there was any significant mean difference in the measured results of the tap and the household water samples at p < 0.05. Binary logistic regression at p < 0.05 was used to determine if there was any significant association between tap and household water contamination (positive for faecal coliform test) and occurrence of diarrhoeal diseases.
Results and discussion
Physicochemical parameters
As shown in Table 1, temperature > 20 °C were measured for 45 (75%) household and 43 (71.7%) tap water samples. Turbidity > 5NTU was measured for 5 (8.3%) water samples taken from households, no tap water sample was found with turbidity > 5NTU. From the total water samples, pH > 8 was measured for 9 (15%) households and for 1 (1.7%) tap water sample (Table 1).
High water temperature enhances the growth of microorganisms and may also cause taste, odour, colour and corrosion problems (Girmay et al. 2021; Price et al. 2019). Most pathogens require higher temperature to proliferate in the water (Slavik et al. 2020; WHO 2021; Gizachew et al. 2020). Prevalence of Vibrio cholerae in water is higher at a temperature above 20 °C and it is recommended to keep water below 20 °C (WHO 2008). Other similar studies also reported that majority of drinking water samples taken from taps or storage containers have a temperature > 20 °C, which is above WHO standard (Abera et al. 2011; Tabor et al. 2011; Tsega et al. 2013; Yasin et al. 2015b). Water pH (acidic or alkaline) is a factor that determines solubility of both organic and inorganic compounds in the water. International and national guidelines recommend a pH range of 6.5–8.0 for drinking water. Out of the total samples collected from the households, 15% were not met the recommended pH range. Turbidity deteriorates the physical quality and acceptance of drinking water as well contributes to the alteration of colour, odour and taste of the water (WHO 2021; Mohammed and Abdulrazzaq 2018; Sitotaw and Geremew 2021). All the sampled tap water met both the WHO and national standard (< 5NTU) while 5 (8.3%) of household water samples had turbidity above the standards. Residual free chlorine is important to control re-growth of microbes in the distribution system and at home (WHO 2019, 2011). In 9 (15%) tap and 25 (41.7%) household water samples, no residual free chlorine was detected. In 17 (28.3%) tap and29 (43.3%) household water samples, the detected residual free chlorine was < 0.2 mg/L (Table 1). The result implied that majority of the water (43.3% tap and 85% household) samples tested for residual free chlorine fall below the standard level of WHO (0.2–0.5 mg/L). Water samples—15% from the tap and 41.7% from the household water—were also fall below the national standard (0.1–0.2 mg/L).
The paired t test result showed that there was a significant mean difference (p < 0.05) between the physicochemical parameters measured to the tap water samples and the household water samples, except for the temperature (Table 2). The t values indicated that the household water samples had higher turbidity and pH and lower residual free chlorine than the tap water samples (the quality decreased after storage).
Bacteriological quality
Regarding the bacteriological quality, 8 (13.3%) tap and 28 (46.7%) household water samples were found positive for the total coliform test; 4 (6.7%) tap and 19 (31.6%) household water samples were found positive for the faecal coliform test (Table 3). Other similar studies conducted in different cities of Ethiopia also revealed comparable findings regarding microbial quality of drinking water (Sitotaw et al. 2021; Wolde et al. 2020; Yasin et al. 2015a; Edessa et al. 2017; Feleke et al. 2018; Gizachew et al. 2020; Adane et al. 2017). Both the national and WHO standard recommended 0 CFU/100 ml of water for coliform. Based on the level of faecal coliform present, WHO drinking water sanitary inspection guideline also set risk-to-health category (Table 3). The paired t test analysed to bacteriological test results indicated that there was a significant mean difference (p < 0.05) between the measured results of the tap and household water samples. The t values implied that more coliform bacteria detected in household water samples than the tap water samples (Table 2).
Variables were also computed to identify the specific points of faecal contamination. From 19 (31.7%) faecally contaminated household water samples, 15 (25%) water samples were contaminated at the household level. From 11 (18.3%) abdominal discomfort cases, 9 (15%) of them occurred in the households where stored water samples were positive for faecal coliform and 7 (11.7%) of the cases were reported from households where tap water samples were negative but household water samples were positive for faecal coliform (Table 4). This result has an important implication regarding the need to deal with drinking water quality beyond the source and the tap, at the household level. The association between quality and household water handling also well noted in other studies (Abera et al. 2018; Handam et al. 2020; Li and Wu, 2019; Duressa et al. 2019; Feleke et al. 2018).
Binary logistic regression was done to investigate any significant association between occurrence of diarrhoeal diseases and faecal contamination of water samples taken from the tap and from households’ storage containers. Presence or absence of faecal coliform in the tap and stored water samples were taken as explanatory variables to evaluate their effect on the occurrence of diarrhoeal diseases. The Hosmer–Lemeshow goodness-of-fit (p = 0.971) implies the model is fit to explain the association and the overall percentage (81.7%) from the classification table also implied the occurrence of diarrhoeal diseases can be predicted with the two variables.
As shown in Table 5c, the odds of the occurrence of diarrhoeal disease is 17.33 for households with stored water samples test results became positive for faecal coliform than those households with stored water samples test results became negative for faecal coliform (p < 0.05). It clearly indicates that drinking water contamination that occurred at the household level is a major public health problem. The occurrence of such health problem is also supported by other similar studies (Slavik et al. 2020; Feleke et al. 2018; Li and Wu 2019).
In conclusion, the physicochemical and microbial quality of drinking water stored at the household level is significantly different from the corresponding tap water. Faecal contamination occurred at the household level is significantly high and is a possible cause of abdominal discomfort and diarrhoeal diseases occurred in the family members of the slum households. In general, drinking water quality in urban slum households of Hawassa city is an actual public health concern. Finally, it is recommended that community-based health education about proper drinking water handling practices and prevention of communicable diseases like diarrhoea is very important in urban slum dwellings.
References
Abera B, Mulu W, Yizengaw E, Hailu T, Kibret M (2018) Water safety, sanitation and hygiene related knowledge, attitudes and practices among household residents in peri-urban areas in Northwest Ethiopia. Ethiopian J Health Develop, 32
Abera S, Zeyinudin A, Kebede B, Deribew A, Ali S, Zemene E (2011) Bacteriological analysis of drinking water sources. African Journal of Microbiology Research 5:2638–2641
Adane M, Mengistie B, Medhin G, Kloos H, Mulat W (2017) Piped water supply interruptions and acute diarrhea among under-five children in Addis Ababa slums, Ethiopia: a matched case-control study. PLoS One 12:e0181516
CSA & ICF (2016) Ethiopia demographic health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.
Duressa G, Assefa F & Jida M (2019) Assessment of bacteriological and physicochemical quality of drinking water from source to household tap connection in Nekemte, Oromia, Ethiopia. J Environ Public Health, 2019
Edessa N, Geritu N, Mulugeta K (2017) Microbiological assessment of drinking water with reference to diarrheagenic bacterial pathogens in Shashemane rural district, Ethiopia. African J Microbiol Res 11:254–263
Feleke H, Medhin G, Kloos H, Gangathulasi J, Asrat D (2018) Household-stored drinking water quality among households of under-five children with and without acute diarrhea in towns of Wegera District, in North Gondar, Northwest Ethiopia. Environ Monit Assess 190:1–12
Girmay AM, Gari SR, Gessew GT, Reta MT (2021) Determinants of drinking water quality and sanitary risk levels of water storage in food establishments of Addis Ababa, Ethiopia. J Water Sanitation Hygiene Develop 11:831–840
Gizachew M, Admasie A, Wegi C, Assefa E (2020) Bacteriological contamination of drinking water supply from protected water sources to point of use and water handling practices among beneficiary households of boloso sore woreda, wolaita zone, Ethiopia. Int J Microbiol 2020:1–10
Handam NB, Santos JAAD, Moraes Neto AHAD, Alencar MDFL, Ignacio CF, Sotero-Martins A (2020) Drinking water quality in Brazilian urban slums. Revista Ambiente Água, 15
Kassegne AB, Leta S (2020) Assessment of physicochemical and bacteriological water quality of drinking water in Ankober district, Amhara region. Ethiopia Cogent Environ Sci 6:1791461
Li P, Wu J (2019) Drinking water quality and public health. Exposure Health 11:73–79
Mohammed SI, Abdulrazzaq KA (2018) Developing water quality index to assess the quality of the drinking water. Civil Eng J 4:2345–2355
Price H, Adams E, Quilliam RS (2019) The difference a day can make: the temporal dynamics of drinking water access and quality in urban slums. Sci Total Environ 671:818–826
Satapathy BK (2014) Safe drinking water in slums: from water coverage to water quality. Economic Political Weekly, 50–55
Sharma HR, Worku W, Hassen M, Tadesse Y, Zewdu M, Kibret D, Gashe A, Meseret M, Gessesse D, Kebede A (2013) Water handling practices and level of contamination between source and point-of-use in Kolladiba Town, Ethiopia. Environ We Int J Sci Technol 8:25–35
Sitotaw B, Geremew M (2021) Bacteriological and physicochemical quality of drinking water in Adis Kidame town, Northwest Ethiopia. Int J microbiol, 2021
Sitotaw B, Melkie E, Temesgen D (2021) Bacteriological and physicochemical quality of drinking water in Wegeda Town, Northwest Ethiopia. J Environ Public Health, 2021
Slavik I, Oliveira KR, Cheung PB, Uhl W (2020) Water quality aspects related to domestic drinking water storage tanks and consideration in current standards and guidelines throughout the world–a review. J Water Health 18:439–463
Tabor M, Kibret M, Abera B (2011) Bacteriological and physicochemical quality of drinking water and hygiene-sanitation practices of the consumers in Bahir Dar city, Ethiopia. Ethiop J Health Sci 21:19–26
Tsega N, Sahile S, Kibret M, Abera B (2013) Bacteriological and physico-chemical quality of drinking water sources in a rural community of Ethiopia. Afr Health Sci 13:1156–1161
UN 2016. Transforming our world: The 2030 agenda for sustainable development.
UN 2020. The sustainable development goals report 2020.
Werkneh AA, Medhanit BZ, Abay AK, Damte JY (2015) Physico-chemical analysis of drinking water quality at Jigjiga City, Ethiopia. Am J Environ Protection 4:29–32
WHO (2004) Guidelines for drinking-water quality. World Health Organization
WHO (2006) Guidelines for drinking-water quality [electronic resource]: incorporating first addendum. Vol 1, Recommendations. third edition (ed) World Health Organization, Geneva, Switzerland
WHO. 2008. Guidelines for drinking-water quality: incorporating first and second addenda, Vol1, Recommendations
WHO 2011. Guidelines for drinking-water quality, Fourth Edition. WHO chronicle, 38, 104–8
WHO (2019) Progress on household drinking water, sanitation and hygiene 2000–2017: special focus on inequalities. World Health Organization, Geneva, Switzerland
WHO (2021) A global overview of national regulations and standards for drinking-water quality
Wolde AM, Jemal K, Woldearegay GM, Tullu KD (2020) Quality and safety of municipal drinking water in Addis Ababa City, Ethiopia. Environ Health Prev Med 25:1–6
Yasin M, Ketema T, Bacha K (2015a) Physico-chemical and bacteriological quality of drinking water of different sources, Jimma zone, Southwest Ethiopia. BMC Res Notes 8:1–13
Yasin M, Ketema T, Bacha K (2015b) Physico-chemical and bacteriological quality of drinking water of different sources, Jimma zone. Southwest Ethiopia BMC Res Notes 8:541
Funding
The study was funded by Hawassa College of Health Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest regarding this publication.
Ethical approval
The authors declare that the study was conducted considering all the necessary research ethics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bekele, R.S., Teka, M.A. Physicochemical and microbial quality of drinking water in slum households of Hawassa City, Ethiopia. Appl Water Sci 13, 4 (2023). https://doi.org/10.1007/s13201-022-01806-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13201-022-01806-0