Abstract
Background
We aimed to construct a risk model to assess the diagnostic value of predicting hypertensive disorders of pregnancy (HDPs) by screening a range of prenatal markers, including pregnancy-associated plasma protein A (PAPP-A), free beta-human chorionic gonadotropin (free β-hCG), and fetal nuchal translucency (NT).
Method
We analyzed 902 women, classified into four groups: healthy gravidas (n = 680, controls), gravidas with gestational hypertension (n = 61; GH), gravidas with preeclampsia (n = 90; PE), and gravidas with severe preeclampsia (n = 71, SPE). We then compared the multiple of median (MoM) of PAPP-A, free β-hCG, and NT. A risk model was constructed and receiver operating characteristic curve (ROC) analysis was used to diagnose HDPs.
Results
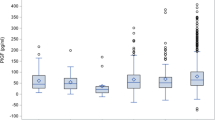
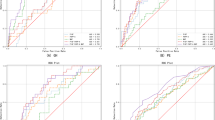
Levels of PAPP-A and free β-hCG levels in the GH, PE, and SPE groups were significantly lower than those in the control group (χ2 = 7.522, P = 0.001; χ2 = 17.775, P < 0.001). NT did not differ significantly when compared across all four groups (χ2 = 1.592, P > 0.05). When the cut-off values for PAPP-A and free β-hCG were 0.795 MoM and 1.185 MoM, the corresponding sensitivities and specificities were 0.514 and 0.635, and 0.734 and 0.450, respectively. The best risk calculation featured PAPP-A, free β-hCG, and NT; this model exhibited the highest diagnostic value in the SPE group, followed by the GH group and then the PE group.
Conclusion
The use of prenatal screening markers during early pregnancy can identify fetal aneuploidy and can also predict HDPs. The development of innovative screening strategies for gravidas and the targeted prevention of HDPs in high-risk gravidas are essential for perinatal care and early intervention, thus creating significant opportunities for predictive and preventive personalized medicine. In our study, we found that the combination of a series of prenatal screening markers in early pregnancy is better than a single marker; our data clearly demonstrate the diagnostic value of combining PAPP-A, free β-hCG, and NT for patients with SPE.


Similar content being viewed by others
Abbreviations
- PAPP-A:
-
pregnancy-associated plasma protein A
- free β-hCG:
-
free beta-human chorionic gonadotropin
- NT:
-
nuchal translucency
- HDP:
-
hypertensive disorders of pregnancy
- GH:
-
gestational hypertension
- PE:
-
preeclampsia
- SPE:
-
severe preeclampsia
- MoM:
-
multiple of the median
- ROC:
-
receiver operating characteristic
- AUC:
-
area under curve
- PPPM:
-
predictive, preventive and personalized medicine
- OR:
-
odds ratio
References
Webster K, Fishburn S, Maresh M, Findlay SC, Chappell LC. Diagnosis and management of hypertension in pregnancy: summary of updated NICE guidance. BMJ. 2019;366:l5119. https://doi.org/10.1136/bmj.l5119.
Peres GM, Mariana M, Cairrao E. Pre-Eclampsia and Eclampsia: An Update on the Pharmacological Treatment Applied in Portugal. J Cardiovasc Dev Dis. 2018;5(1):3. https://doi.org/10.3390/jcdd5010003.
Armaly Z, Jadaon JE, Jabbour A, Abassi ZA. Preeclampsia: Novel Mechanisms and Potential Therapeutic Approaches. Front Physiol. 2018;9:973. https://doi.org/10.3389/fphys.2018.00973.
Helmo FR, Lopes A, Carneiro A, Campos CG, Silva PB, Dos RMM, et al. Angiogenic and antiangiogenic factors in preeclampsia. Pathol Res Pract. 2018;214(1):7–14. https://doi.org/10.1016/j.prp.2017.10.021.
Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 2014;4(2):97–104. https://doi.org/10.1016/j.preghy.2014.02.001.
Hitti J, Sienas L, Walker S, Benedetti TJ, Easterling T. Contribution of hypertension to severe maternal morbidity. Am J Obstet Gynecol. 2018;219(4):405.e1–7. https://doi.org/10.1016/j.ajog.2018.07.002.
Nathan HL, Seed PT, Hezelgrave NL, De Greeff A, Lawley E, Conti-Ramsden F, et al. Maternal and perinatal adverse outcomes in women with pre-eclampsia cared for at facility-level in South Africa: a prospective cohort study. J Glob Health. 2018;8(2):020401. https://doi.org/10.7189/jogh.08-020401.
Manna S, McCarthy C, McCarthy FP. Placental Ageing in Adverse Pregnancy Outcomes: Telomere Shortening, Cell Senescence, and Mitochondrial Dysfunction. Oxid Med Cell Longev. 2019;2019:3095383–11. https://doi.org/10.1155/2019/3095383.
Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalized medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J. 2014;5(1):6. https://doi.org/10.1186/1878-5085-5-6.
Lemke HU, Golubnitschaja O. Towards personal health care with model-guided medicine: long-term PPPM-related strategies and realisation opportunities within ‘Horizon 2020’. EPMA J. 2014;5(1):8. https://doi.org/10.1186/1878-5085-5-8.
Anto EO, Roberts P, Coall D, Turpin CA, Adua E, Wang Y, et al. Integration of suboptimal health status evaluation as a criterion for prediction of preeclampsia is strongly recommended for healthcare management in pregnancy: a prospective cohort study in a Ghanaian population. EPMA J. 2019;10(3):211–26. https://doi.org/10.1007/s13167-019-00183-0.
Li B, Sahota DS, Lao TT, Xu J, Hu SQ, Zhang L, et al. Applicability of first-trimester combined screening for fetal trisomy 21 in a resource-limited setting in mainland China. BJOG. 2016;123(Suppl 3):23–9. https://doi.org/10.1111/1471-0528.14004.
Hartwig TS, Sorensen S, Jorgensen FS. The maternal age-related first trimester risks for trisomy 21, 18 and 13 based on Danish first trimester data from 2005 to 2014. Prenat Diagn. 2016;36(7):643–9. https://doi.org/10.1002/pd.4833.
Lan RY, Chou CT, Wang PH, Chen RC, Hsiao CH. Trisomy 21 screening based on first and second trimester in a Taiwanese population. Taiwan J ObstetGynecol. 2018;57(4):551–4. https://doi.org/10.1016/j.tjog.2018.06.014.
Cuckle H, Maymon R. Development of prenatal screening--A historical overview. SeminPerinatol. 2016;40(1):12–22. https://doi.org/10.1053/j.semperi.2015.11.003.
Bernardes TP, Zwertbroek EF, Broekhuijsen K, Koopmans C, Boers K, Owens M, et al. Delivery or expectant management for prevention of adverse maternal and neonatal outcomes in hypertensive disorders of pregnancy: an individual participant data meta-analysis. Ultrasound Obstet Gynecol. 2019;53(4):443–53. https://doi.org/10.1002/uog.20224.
Quan LM, Xu QL, Zhang GQ, Wu LL, Xu H. An analysis of the risk factors of preeclampsia and prediction based on combined biochemical indexes. Kaohsiung J Med Sci. 2018;34(2):109–12. https://doi.org/10.1016/j.kjms.2017.10.001.
LI Ping. Study on the relationship between the changes of serum EGF via β-hCG and the pathogenesis of preeclampsia [D]. Hebei Medical University, [Artile in Chinese]. http://kns.cnki.net/KCMS/detail/detail.aspx?FileName=1015327834.nh&DbName=CMFD2016
Wright A, Guerra L, Pellegrino M, Wright D, Nicolaides KH. Maternal serum PAPP-A and free beta-hCG at 12, 22 and 32 weeks' gestation in screening for pre-eclampsia. Ultrasound Obstet Gynecol. 2016;47(6):762–7. https://doi.org/10.1002/uog.15849.
Tiyatha S, Sirilert S, Sekararithi R, Tongsong T. Association between unexplained thickened nuchal translucency and adverse pregnancy outcomes. Arch Gynecol Obstet. 2018;298(1):97–101. https://doi.org/10.1007/s00404-018-4790-9.
Tsai MS, Lee FK, Cheng CC, Hwa KY, Cheong ML, She BQ. Association between fetal nuchal translucency thickness in first trimester and subsequent gestational hypertension and preeclampsia. Prenat Diagn. 2002;22(9):747–51. https://doi.org/10.1002/pd.396.
Chinese Medical Association Obstetrics, Gynecology Branch Pregnancy Hypertension Disease Group. Guidelines for Diagnosis and Treatment of Hypertension during Pregnancy (2015). Chin J Obstet Gynecol. 2015;50:721–8. [Artile in Chinese]. https://doi.org/10.3760/cma.j.issn.0529-567x.2015.10.001.
Bestwick JP, Huttly WJ, Wald NJ. Distribution of nuchal translucency in antenatal screening for Down's syndrome. J Med Screen. 2010;17(1):8–12. https://doi.org/10.1258/jms.2010.009107.
Bestwick JP, Huttly WJ, Wald NJ. The estimation of median nuchal translucency values between 10 and 14 weeks of pregnancy. J Med Screen. 2014;21(2):110–2. https://doi.org/10.1177/0969141314536890.
Royston P, Thompson SG. Model-based screening by risk with application to Down's syndrome. Stat Med. 1992;11(2):257–68. https://doi.org/10.1002/sim.4780110211.
Bock JL. Current issues in maternal serum alpha-fetoprotein screening. Am J Clin Pathol. 1992;97(4):541–54. https://doi.org/10.1093/ajcp/97.4.541.
Cuckle HS, Wald NJ, Thompson SG. Estimating a woman's risk of having a pregnancy associated with Down's syndrome using her age and serum alpha-fetoprotein level. Br J Obstet Gynaecol. 1987;94(5):387–402. https://doi.org/10.1111/j.1471-0528.1987.tb03115.x.
Chen Y, Huang J, Mei J. A risk prediction model for fetal hypospadias by testing maternal serum AFP and free beta-HCG. Clin Biochem. 2019;69(7):21–5. https://doi.org/10.1016/j.clinbiochem.2019.05.015.
Memtsa M, Jurkovic D, Jauniaux E. Diagnostic Biomarkers for Predicting Adverse Early Pregnancy Outcomes: Scientific Impact Paper No. 58. BJOG. 2019;126(3):e107–13. https://doi.org/10.1111/1471-0528.15468.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. Epma J. 2016;7:23. https://doi.org/10.1186/s13167-016-0072-4.
Kaijomaa M, Rahkonen L, Ulander VM, Hamalainen E, Alfthan H, Markkanen H, et al. Low maternal pregnancy-associated plasma protein A during the first trimester of pregnancy and pregnancy outcomes. Int J Gynaecol Obstet. 2017;136(1):76–82. https://doi.org/10.1002/ijgo.12002.
Morris RK, Bilagi A, Devani P, Kilby MD. Association of serum PAPP-A levels in first trimester with small for gestational age and adverse pregnancy outcomes: systematic review and meta-analysis. Prenat Diagn. 2017;37(3):253–65. https://doi.org/10.1002/pd.5001.
Ozdamar O, Gun I, Keskin U, Kocak N, Mungen E. The role of maternal serumbeta- HCG and PAPP-A levels at gestational weeks 10 to 14 in the prediction of pre- eclampsia. Pak J Med Sci. 2014;30(3):568–73. https://doi.org/10.12669/pjms.303.4554.
Mikat B, Zeller A, Scherag A, Drommelschmidt K, Kimmig R, Schmidt M. betahCG and PAPP-A in first trimester: predictive factors for preeclampsia? Hypertens Pregnancy. 2012;31(2):261–7. https://doi.org/10.3109/10641955.2011.638956.
Ceylan N, Ozaksit G, Unlu BS, Yildiz Y, Yilmaz S, Agaca F. Can first trimester placental protein-13 and pregnancy-associated plasma protein-A predict pre-eclampsia in Turkish women? J Obstet Gynaecol. 2014;34(6):482–5. https://doi.org/10.3109/01443615.2014.911832.
Yucel B, Gedikbasi A, Dundar O, Olgac Y, Yildirim D, Yildirim G, et al. The utility of first trimester uterine artery Doppler, placental volume and PAPP-A levels alone and in combination to predict preeclampsia. Pregnancy Hypertens. 2016;6(4):269–73. https://doi.org/10.1016/j.preghy.2016.04.007.
Jelliffe-Pawlowski LL, Baer RJ, Currier RJ, Lyell DJ, Blumenfeld YJ, El-Sayed YY, et al. Early-onset severe preeclampsia by first trimester pregnancy- associated plasma protein A and total human chorionic gonadotropin. Am J Perinatol. 2015;32(7):703–12. https://doi.org/10.1055/s-0034-1396697.
Spencer CA, Allen VM, Flowerdew G, Dooley K, Dodds L. Low levels of maternal serum PAPP-A in early pregnancy and the risk of adverse outcomes. Prenat Diagn. 2008;28(11):1029–36. https://doi.org/10.1002/pd.2116.
Hedley PL, Placing S, Wojdemann K, Carlsen AL, Shalmi AC, Sundberg K, et al. Free leptin index and PAPP-A: a first trimester maternal serum screening test for pre-eclampsia. Prenat Diagn. 2010;30(2):103–9. https://doi.org/10.1002/pd.2337.
Golubnitschaja O, Costigliola V, EPMA. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European association for predictive, preventive and personalised medicine. EPMA J. 2012;3(1):14. https://doi.org/10.1186/1878-5085-3-14.
Ornaghi S, Algeri P, Todyrenchuk L, Vertemati E, Vergani P. Impact of excessive pre-pregnancy body mass index and abnormal gestational weight gain on pregnancy outcomes in women with chronic hypertension. Pregnancy Hypertens. 2018;12:90–5. https://doi.org/10.1016/j.preghy.2018.04.005.
Chen Y, Lu S, Gu L, Zhang Y, Chu X, Zhang W, et al. Relationship between serum PAPP-A, free β-hCG and preeclampsia during early pregnancy. Zhejiang Practical Medicine. 2018;23(1):50–2.[Artile in Chinese]. https://doi.org/10.3969/j.issn.1007-3299.2018.01.019.
Acknowledgments
The authors wish to acknowledge the assistance of Songhe Chen from the medical records room of Hangzhou Women’s Hospital in case collection and data matching. We thank International Science Editing ( http: //www.internationalscienceediting.com ) for editing our manuscript.
Statement of Ethics
The study was approved by Hangzhou Women’s Hospital (Hangzhou Maternity and Child Health Care Hospital) ethics committee, in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. And the approval number was [2018] medical ethics (004) no.01. Consent obtained from study participants was written.
Funding
This study is funded by the Natural Science Foundation of Zhejiang (Grant number LGF19H040006), Zhejiang Medicine and Health Scientific Research Project (disciplinary platform-2018ZD036), Hangzhou Medicine and Health Scientific Research Project (2017A052), and Hangzhou Yuhang District Science and Technology Bureau Research Project (Medical Treatment and Public Health-2018008)
Author information
Authors and Affiliations
Contributions
Yiming Chen (corresponding author) performed laboratory measurements, statistical analysis, and wrote the first draft of the manuscript. Zhen Xie, Xue Wang, Yiming Chen, and Qingxin Xiao contributed to experimental design and participated in laboratory analyses. Xiao Lu and Yezhen Shi were involved in protocol development, patient recruitment, data acquisition, and data analysis. Sha Lu and Shaolei Lv provided intellectual guidance and critically reviewed the manuscript. Yiming Chen conceived and designed the study and critically reviewed the manuscript. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Y., Xie, Z., Wang, X. et al. A risk model of prenatal screening markers in first trimester for predicting hypertensive disorders of pregnancy. EPMA Journal 11, 343–353 (2020). https://doi.org/10.1007/s13167-020-00212-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-020-00212-3