Abstract
Neuroinflammation is associated with the pathophysiologies of neurodegenerative and psychiatric disorders. Evaluating neuroinflammation using positron emission tomography (PET) plays an important role in the early diagnosis and determination of proper treatment of brain diseases. To quantify neuroinflammatory responses in vivo, many PET tracers have been developed using translocator proteins, imidazole-2 binding site, cyclooxygenase, monoamine oxidase-B, adenosine, cannabinoid, purinergic P2X7, and CSF-1 receptors as biomarkers. In this review, we introduce the latest developments in PET tracers that can image neuroinflammation, focusing on clinical trials, and further consider their current implications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurodegeneration is characterized by gradual and progressive loss of the neuronal population, whereas psychiatric disorders are characterized by the disruption of neurocircuits in the central nervous system (CNS) [1]. These brain diseases are closely related to age, and their prevalence tends to increase as society ages; such affect not only patients themselves but also other’s lives. Therefore, diagnosing brain diseases early is crucial. Although decades of efforts developing therapeutic drugs to overcome brain diseases, most clinical trials have failed, and currently prescribed drugs are used for temporary relief and to slow disease progression [2, 3]. To understand the mechanisms underlying the pathophysiology of brain diseases, considering not only the damage to certain brain tissues but also the surrounding neuronal environment is necessary.
Neuroinflammation is an innate immunological response in the CNS activated in response to various pathological insults, including infection, misfolded protein aggregation, and trauma [4]. Microglia and astrocytes, the main immune components, are key regulators of neuroinflammation and play crucial homeostatic roles for neuronal functioning [5]. Under physiological conditions, these cells maintain homeostasis by removing cellular debris during phagocytosis. However, in pathological conditions caused by chronic insults beyond their threshold, such glial cells become overactive and release various neurotoxins that induce neuronal death. The neurotoxins in turn activate glial cells again, destroying the continuous neural circuit in a vicious cycle [6]. Neuroinflammation plays an important role in various neurodegenerative diseases and psychiatric disorders, including Alzheimer’s disease (AD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), major depressive disorder (MDD), and posttraumatic stress disorder (PTSD) [7].
Positron emission tomography (PET) is a molecular imaging technique that can evaluate in vivo biochemical changes in living organisms without pharmacological effects, allowing the functional evaluation of neuroinflammatory responses in a noninvasive manner [8]. Elucidating the dynamic roles of glial cells in disease progression with PET is useful in the determination of disease status or evaluation of therapeutic intervention, as inflammatory reactions occur before the clinical symptoms of brain diseases are expressed. Multiple lines of evidence suggest that inflammation and reactive gliosis occur years before the onset of AD [9,10,11].
As illustrated in Fig. 1, representative biomarkers for neuroinflammation can be largely divided into proteins (translocator proteins), enzymes (cyclooxygenase and monoamine oxidase-B), and various receptors (imidazole-2 binding site, and adenosine, cannabinoid, purinergic P2X7, and colony stimulating factor-1 receptors). Although research began approximately 40 years ago, attempts to assess neuroinflammation have yet to obtain robust results in clinical trials. In the present review, we introduce the state-of-the-art status of the development of PET tracers that can evaluate neuroinflammation and consider their implications at this point in time.
Imaging Microglia
Translocator Proteins (TSPO)
The first PET tracer developed to assess microglial activity through translocator proteins (TSPO) was [11C]PK11195, which showed increased binding in patients with AD compared with healthy controls [12]. In a head-to-head comparison study with [11C]PK11195 and [11C]PIB (a specific radiotracer for amyloid-β plaques), the [11C]PK11195 binding was increased in the cortical and sub-cortical areas in which uptake was increased in [11C]PIB, and an inverse correlation with the mini-mental state exam (MMSE) score, but not with the [11C]PIB binding ratio [13]. These results indicated that a neuroinflammatory response may occur prior to amyloid pathology. However, [11C]PK11195 has limitations such as low permeability and high non-specific plasma binding [14].
To overcome the shortcomings of [11C]PK11195, second-generation TSPO PET radiotracers, including [11C]DAA1106, [11C]DPA713, [18F]PBR06, [18F]PBR28, and [18F]DPA714 have been developed [15]. [3H]DAA1106 showed a tenfold higher binding affinity and approximately 1.5 times higher specific binding than [3H]PK11195 in tissues of individuals with neurological diseases compared to controls [16]; however, it failed to differentiate a rat model of herpes encephalitis from a control group [17]. PET employing [11C]DPA713 presented a lower background signal and higher specific binding than [11C]PK11195 in a rat model of herpes [18]. Yokokura et. al. reported that [11C]DPA713 PET showed increased uptake in the brain of patients with AD compared to healthy subjects. However, [11C]PK11195 PET displayed no difference in individuals with AD, and [11C]DPA713 binding values were also significantly negatively correlated with MMSE [19]. These results imply that [11C]DPA713 is more sensitive to TSPOs than [11C]PK11195. In a multiple sclerosis (MS) study using [18F]PBR06, the uptake ratio in the right striatum was elevated in patients with MS with or without fatigue [20]. In patients with early phase PD, [18F]PBR06 showed an increased brain uptake ratio in the ipsilateral putaminal side of the motor onset, and these binding ratios were correlated with dopaminergic denervation but not with disease severity [21]. In a study on TSPO changes in AD, Kreisl et al. demonstrated that the binding of [11C]PBR28 increased in the cortical region, especially in the parietal and temporal lobes, compared to the control group, and that the binding was inversely proportional to cognitive function. This increase in binding was more significant in early onset than in late onset AD [22]. In a study on lateral sclerosis using [11C]PBR28, brain uptake was increased in amyotrophic and primary lateral sclerosis [23]. An important drawback of second-generation TSPO radiotracers is their large inter-subject variability due to a single nucleotide polymorphism in rs6971 or rs2997325, which generates high-, mixed-, and low-affinity binders between subjects [24,25,26,27,28]; here, a “low-affinity binder” indicates that the radiotracer’s binding to a specific target biomarker (i.e., TSPO) is low, which greatly degrades the quality of PET images. Polymorphisms in subjects can be identified through genetic analysis of leukocytes, and the results can be used to interpret PET images from second-generation PET tracers.
Third-generation PET radiotracers, including [11C]ER176, [18F]GE180, and [18F]BS224, have been developed to minimize the effects of genetic polymorphisms. A comparative study in healthy volunteers reported that [11C]ER176 was more stable in arterial blood and possessed a higher distribution volume and binding potential than [11C]PBR28 [29]. In clinical applications, [18F]GE180 showed strong tumor uptake in patients with untreated and pretreated glioblastoma (maximum tumor-to-background ratio, 6.61) [30]. [18F]GE180 presented high uptake, determining active MS lesions, in patients with relapsing–remitting MS regardless of individual binding status [31]. [18F]GE180 displayed increased brain uptake in cerebral cavernous malformations [32]. In an in vitro competitive inhibition assay, [11C]ER176 and [18F]GE180 were reported to be minimally affected by polymorphisms; however, these PET tracers displayed a considerable decrease in low-affinity binders [33, 34]. [18F]BS224 has recently been developed as a PET tracer that is insensitive to TSPO polymorphisms, and its efficacy has been proven in a lipopolysaccharide (LPS)-based inflammatory model; however, the results of its clinical application studies are still unknown [35].
Although TSPO-specific PET tracers are the most studied biomarkers of neuroinflammation, they are localized in the outer mitochondrial membrane and are mainly expressed in microglia and astrocytes [36]. Therefore, as determining whether the increased PET signal through TSPO is caused by microglia, astrocytes, or both is not possible, other biomarker-based PET tracers with high selectivity for microglia have been developed.
Adenosine Receptor
Adenosine is an endogenous purine nucleoside derived from the hydrolysis of adenosine triphosphate. In a pathological state, neurons and glial cells release adenosine into the extracellular space, promoting inflammation that exacerbates neuronal injury [37]. Adenosine receptors are expressed on astrocytes and microglia [38]. To date, PET studies evaluating adenosine receptors have mainly been conducted using adenosine receptors 1 (A1) and 2 (A2). [11C]MPDX and [18F]CPFPX were developed as selective PET radiotracers for A1 receptors, whereas [11C]TMSX, [11C]SCH442416, [18F]MNI-444, and [11C]preladenant were developed for A2 receptors.
In early drug-naïve patients with PD, [11C]MPDX PET did not reveal altered A1 receptors compared with healthy controls [39]; however, an increased binding potential was identified in the frontal cortex, posterior cingulate cortex, and Rolandic area in patients with traumatic brain injury [40]. [18F]CPFPX PET showed increased uptake in ischemic hemispheres, followed by a progressive decline [41]; the radiotracer presented a relatively low fraction of specific binding (total equilibrium uptake: 33% and 66% in the cerebellum and cortex, respectively) in a human displacement study, resulting in difficulties in performing kinetic modeling using the cerebellum as a reference region [42].
In a clinical study on [11C]TMSX, Mishina et al. demonstrated increased putaminal binding in patients with PD with dyskinesia, but similar striatal binding between drug-naïve patients with PD and healthy controls [43]. [11C]TMSX PET showed increased brain uptake in a study of secondary progressive MS [44]. [11C]SCH442416 PET revealed that patients with PD with levodopa-induced dyskinesia possessed higher binding values than those without dyskinesia, who had comparable binding potential to healthy controls [45]. [18F]MNI-444 PET showed reasonable binding values (binding potentials: 2.6–4.9 in A2-rich regions) and good test-retest variability (<10%) in a preliminary human study [46]; however, a clinical application study using [18F]MNI-444 has not yet been conducted. Employing the [11C]preladenant, PET generated similar basal ganglia binding between the PD and control groups [47].
Cannabinoid Receptor 2 (CB2)
The cannabinoid receptor 2 (CB2) is primarily expressed on the peripheral immune cells [48]. In the brain, CB2 expression is low and mainly found in microglia [49]. In an inflammatory state, CB2 expression is upregulated depending on the inflammatory context [50]. The radiochemistry of [11C]methoxy-Sch225336 was established, however, its brain uptake was low, possibly due to efflux pumps in the blood-brain barrier [51]. The [11C]NE40 demonstrated specific binding to CB2 in a rat model with local overexpression of the human CB2 receptor [52]. However, in the first-in-human study, [11C]NE40 PET presented a lower receptor availability in patients with AD, and did not differentiate patients with AD from healthy controls [53]. The reason for the failure in clinical patient application was thought to be the low affinity for CB2, and subsequent studies were conducted to improve the binding affinity.
Although [11C]A-836339 greatly improved the binding affinity for CB2 compared to [11C]NE40 (Ki 0.7 nM and 9.6 nM for [11C]A-836339 and [11C]NE40, respectively), no significant was identified difference between stroke or ischemic animal models and sham operated ones [54,55,56]. [11C]GW405833 showed a high affinity for CB2 (Ki 3.6 nM) and 78-fold selectivity for rats’ CB1 [57]. However, it presented a slow washout and high non-specific binding in a nonhuman primate model [58]. [18F]MA3 with 62 times greater affinity for CB2 and 13 times greater selectivity than [11C]NE40, has been developed [59]; in a subsequent study, [18F]MA3 showed specific binding in a rat model with local overexpression of the CB2 receptor; however, no difference was found between the control and blockade in a healthy nonhuman primate [60].
Cyclooxygenase (COX)
Arachidonic acid (AA) is a polyunsaturated fatty acid found in the cell membrane phospholipids. If tissue injury occurs, the phospholipid membrane produces AA by phospholipases A2 and C. Then, cyclooxygenase (COX) catalyzes the conversion of AA to prostaglandins G2 and H2, which are related to neuroinflammation [61]. COX-1 and COX-2 are expressed in microglia and neurons in the CNS and are involved in neuroinflammation [62].
[11C]KTP-Me has been developed for selectivity against COX-1 and showed high and fast brain uptake in the early phase, whereas [11C]PK11195 uptake gradually increased and remained for 14 days in a head-to-head comparison study in an LPS-induced inflammation model [63]. Subsequent immunohistochemistry experiments showed that the distribution of activated microglia initially increased because of the expression of COX-1 but not COX-2. In a comparative study with [11C]PIB PET, brain uptake increased in the order of healthy controls, mild cognitive impairment (MCI), and AD, however, no significant difference was identified in amyloid-positive [11C]KTP-Me PET (average peak cortical standard uptake value: healthy control = 2.3, MCI = 1.6, and AD = 2.1) (Fig. 2. [64]). [11C]PS13 presented specific binding for COX-1 in most organs, including the spleen, those in the gastrointestinal tract, and kidneys with abundant COX-1 expression; however, [11C]MC1 showed low selective binding for COX-2 in major organs, except for the ovaries [65]. In a recent study involving healthy human subjects, Choi et al. demonstrated that [11C]PS13 selectively binds to COX-1 and measured the in vivo potency of nonsteroidal anti-inflammatory drugs against COX-1 [66].
Comparison of [11C]PIB and [11C]KTP-Me in Alzheimer’s disease. Reprinted from “Exploratory human PET study of the effectiveness of 11C-ketoprofen methyl ester, a potential biomarker of neuroinflammatory processes in Alzheimer's disease”, volume 43, Ohnishi A, Senda M, Yamane T, Mikami T, Nishida H, Nishio T, et al. Nuclear Medicine and Biology, 438-444, Copyright (2016), with permission from Elsevier
P2X7 Receptor
The P2X7 receptor is a member of the ATP-gated ion channel purinergic P2X receptor family and is highly expressed in microglia, oligodendrocytes and astrocytes [67]. [11C]JNJ54173717 has high affinity for P2X7 (IC50 values= 7.6 and 4.2 nM for rat and recombinant human P2X7 orthologs, respectively) and selectively binds to the hP2X7 in nonhuman primates [68]. However, [11C]JNJ54173717 PET presented no significant differences in binding between healthy subjects and patients with PD because of a genetic polymorphism (rs3751143) [69]. [18F]JNJ64413739 PET displayed increased binding in LPS-treated rats [70]; the radiotracer showed a low test-retest variability (10.7%) and reasonable radiation dosimetry (average effective dose = 22 μSv/MBq) in healthy subjects [71], yet no studies on patients have been reported to date.
Colony Stimulating Factor 1 (CSF-1) Receptor
Colony stimulating factor-1 (CSF-1) receptors are predominantly expressed in microglia [72]. Although AZ683 has a high affinity for CSF-1R (Ki = 8 nM) and >250 times more selectivity than other kinases, [11C]AZ683 PET presented very low brain uptake (< 0.5 SUV) in normal rodents and nonhuman primates [73]. [11C]CPPC showed reasonable binding and selectivity to CSF-1R based on findings from preclinical experiments (increment of specific binding: 59% and 120% in LPS-induced mice and baboons, respectively, and 31% in AD mice) and in vitro postmortem autoradiography studies (selectivity baseline/blockade ratio: 2.7) [74]. However, a subsequent study using [3H]CPPC showed low specific and off-target binding to many kinase targets [75].
Imaging Astrocyte
Imidazole-2 Binding Site (I2BS)
The imidazole-2 biding site (I2BS) is involved in the regulation of glial fibrillary acidic proteins and is expressed in the mitochondrial membranes of astrocytes. [11C]FTIMD showed specific binding to I2BS in rodent and nonhuman primate brains, but remaining radioactivity in the pretreatment experiment was approximately 66–75% of baseline, indicating moderate non-specific binding [76, 77], possibly due to the improper specific activity. To overcome this issue, Kawamura et al. developed [11C]FTIMD, which possesses ultra-high specific activity (>2000 GBq/μmol), generating a 17–34% decrease in non-specific binding [78]. Kawamura et al. additionally synthesized [11C]metrazoline, [18F]FEBU, and [11C]TEIMD as new radiotracers for I2BS. [11C]metrazoline and [18F]FEBU showed highly specific binding to I2BS, but [11C]TEIMD had poor brain permeability [79, 80].
Tyache et al. developed [11C]BU99008, which has a high specific binding to I2BS with a test-retest variability of 15–25% in healthy subjects [81]. In PD, [11C]BU99008 PET demonstrated an increased I2BS binding in patients with early PD but decreased I2BS expression in patients with moderate and advanced PD [82]. In a subsequent study, Mohamed et. al. reported that the binding of [11C]BU99008 did not differ between patients with MDD and healthy controls [83]. In a study of cognitively impaired subjects with MCI or probable AD, [11C]BU99008 binding was elevated compared to healthy controls [84]. In an AD study using [11C]BU99008, astrocyte activity increased in the early stages of low amyloid burden and decreased in the advanced stages of high amyloid burden. In statistical parametric mapping, [11C]BU99008 was positively associated with amyloid PET and negatively associated with gray matter volume and glucose PET (Fig. 3. [85]).
Relationship between [11C]BU99008, [18F]FDG, gray matter volume and [18F]florbetaben in AD patients. This research was originally published in Mol Psychiatry. Livingston NR, Calsolaro V, Hinz R, Nowell J, Raza S, Gentleman S, et al. Relationship between astrocyte reactivity, using novel 11C-BU99008 PET, and glucose metabolism, grey matter volume and amyloid load in cognitively impaired individuals. Mol Psychiatry. 2022;27:2019-29. http://creativecommons.org/licenses/by/4.0/
Monoamine Oxidase B
Monoamine oxidase B (MAO-B) plays a prominent role in the degradation of monoamine neurotransmitters, and abnormally high levels of MAO-B activity are associated with various brain diseases. MAO-B is present at low concentrations in microglia and oligodendrocytes and is mainly expressed in the outer mitochondrial membrane of astrocytes [86].
[11C]D-deprenyl showed fast clearance, whereas [11C]L-deprenyl was retained within the MAO-B-rich regions. Although [11C]L-deprenyl exhibited a much higher brain uptake than [11C]D-deprenyl, its fast and irreversible binding to MAO-B hinders kinetic analysis [87]. Because carbon-hydrogen dissociation is faster than carbon-deuterium dissociation, the so-called kinetic isotope effect, the same group introduced [11C]L-deprenyl-D2 ([11C]DED) by substituting hydrogen with deuterium in deprenyl [88].
[11C]SL25.1188 was developed as a reversible PET tracer for MAO-B and showed high brain permeability and good test-retest reproducibility (12%) in initial clinical trials evaluating healthy subjects [89]. Moriguci et al. reported that the binding of [11C]SL25.1188 was significantly increased by approximately 25% in the prefrontal cortex of patients with a major depressive episode [90]. For patients with PTSD, [11C]SL25.1188 PET showed an 8–17% reduced availability across the brain regions [91]. Additionally, the total distribution volume of [11C]SL25.1188 in traumatic brain injury was considerably higher in the prefrontal cortex compared to the control group [92].
To increase the clinical applicability of radiotracers, [18F]F-DED and [18F]FSL25.1188 were developed substituting C-11 by F-18. [18F]F-DED PET presented an age-dependent increase in binding in an AD animal model (i.e., APP/PS2), and the PET signals in the hippocampus and thalamus positively correlated with MAO-B expression in glial fibrillary acidic protein (GFAP)-positive astrocytes (R > 0.70). In an initial clinical study that recruited various patients and healthy subjects, [18F]F-DED uptake patterns were consistent with MAO-B expression in neurological diseases, as follows: AD without tau and neurodegeneration (A+T-N-), high cortical binding; AD with tau and neurodegeneration (A+T+N+), relatively low cortical binding; PD, moderate global binding with enhanced signal in the basal ganglia; multiple system atrophy, strong cortical binding; and autoimmune encephalitis, strong cerebellar peduncles binding (Fig. 4. [93]). A PET imaging study of [18F]FSL25.1188 in nonhuman primates showed a high brain uptake and regional distribution in accordance with MAO-B expression [94].
[18F]F-DED PET images in various neurodegenerative diseases. This research was originally published in J Neuroinflammation. Ballweg A, Klaus C, Vogler L, Katzdobler S, Wind K, Zatcepin A, et al. [18F]F-DED PET imaging of reactive astrogliosis in neurodegenerative diseases: preclinical proof of concept and first-in-human data. J Neuroinflammation. 2023;20:68. http://creativecommons.org/licenses/by/4.0/
In vitro autoradiography of postmortem experiments showed that [18F]SMBT-1 possessed a higher specific binding in brain sections of patients with AD than in the control group, and this result was reproduced by MAO-B immunohistochemistry [95]. In a preliminary clinical study, [18F]SMBT-1 binding highly correlated with amyloid but not with tau burden. Patients positive for Aβ with normal cognition and those with MCI presented a significantly higher regional binding of [18F]SMBT-1 (Fig. 5, [96]). Additionally, Chatterjee et al. have demonstrated that plasma GFAP was associated with regional [18F]SMBT-1 signaling in patients with AD [97].
Discussion
The development of PET tracers for imaging-reactive gliosis based on microglia and astrocytes started in the 1980s, and research and development are currently underway. PET tracers targeting TSPO have been the most actively studied and recent results from MAO-B have been reported. However, no significant differences were found between patient and healthy control groups in clinical trials for CB2, COX, and P2X7 [52, 63, 68]. Moreover, the use of [11C]CPPC for CSF-1R has the disadvantage of off-target binding [74]. Among the PET tracers developed for the diagnosis of neuroinflammation, the most promising are [11C]BU99008, [18F]SMBT-1, and [11C]SL25.1188 for MAO-B, as such tracers reversible binding to I2BS or MAO-B in astrocytes and high permeability to the brain (SUV > 7). However, the clinical efficacy of these PET tracers should be proven through further studies.
In an LPS-based neuroinflammation study by Shukuri et al., COX PET using [11C]KTP-Me showed rapid uptake in the inflammatory region and rapid excretion, allowing low non-specific binding; however, TSPO PET using [11C]PK11195 displayed relatively slow uptake and maintained the signal in the lesion site, indicating high non-specific binding [62]. These results demonstrate the high nonspecific binding of [11C]PK11195 and suggest that other targets are more suitable than TSPO as biomarkers for evaluating neuroinflammation. To clarify this, a comparative study between a third-generation TSPO PET tracer with less nonspecific binding and other target-based PET tracers is warranted.
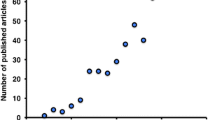
Biomarker-based PET tracers for microglia and astrocytes development began with TSPO and MAO-B and proceeded in the order of adenosine, CB2, COX, P2X7, CSF-1, and I2BS (Fig. 6, Table 1) [17, 33, 35, 46, 51, 53, 54, 58,59,60, 63, 65, 68,69,70,71, 73, 74, 76, 77, 79, 80, 87,88,89, 93,94,95, 103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161]. Examining clinical trials employing PET tracers conducted after 2014, specific studies on patients, except for healthy subjects, are fewer than those published during the entire drug development period. Most clinical studies using the developed PET tracers vary depending on the biomarkers, however, overall, they have been mainly conducted in North America (US, Canada), Europe (Germany, Belgium, United Kingdom), and Japan. The number of applications for AD and PD was the highest, and studies on degenerative brain diseases, such as neuropsychiatric disorders, MS, and multiple system atrophy, were limited to one or two (Table 2) [29, 31,32,33, 46, 47, 53, 64, 66, 69, 71, 81, 82, 84, 85, 90, 91, 93, 97, 141, 145, 147, 150, 154, 162,163,164].
Although PET tracers developed thus far have shown excellent pharmacokinetic characteristics in the preclinical stage (such as high affinity and selectivity, and metabolic stability), most clinical studies did not identify significant differences between patients and control groups or showed inconsistent results. The main issues in developing a successful PET tracer that can be used in clinical settings are as follows. First, previous studies have mainly used rodents, whereas glial cells have species-specific differences. Human microglia and astrocytes are significantly different from those of rodents in terms of morphology, gene expression, and function [98,99,100,101,102]. Therefore, despite the limitations of using postmortem human microglia and astrocytes, research on human in vitro models is indispensable to verify their efficacy. Second, the reason for the lack of a significant differences between the patient and control groups may be that the affinity of the PET tracer is not high enough to detect changes in low concentrations of biomarkers. [11C]PS13 for COX-1 and [11C]MC1 for COX-2 had similar affinities at a level of 1nM, yet only [11C]PS13 possessed reasonable brain uptake. To address this, Kim et al. suggested that the constituent density of COX-2 was much lower than that of COX-1, which indicates that the PET tracer for COX-2 should have a high affinity at the pM level. Additionally, Atili et al. suggested that the reason for the failure of the blockade experiment for [11C]MA3 was that the expression of CB2 receptors was too low at normal levels. Third, the degree of neuroinflammation does not appear to have a one-dimensional proportional relationship with the severity of brain disease pathology. That is, although neuroinflammation is closely related to various brain diseases, the density of activated glial cells tends to decrease as the disease progresses. Therefore, PET-identified gliosis may not be different from the healthy control group depending on the severity of the disease in the participating patient. For instance, studies on AD have shown that the density of reactive glial cells increases before tau pathology (A+T-N-) accumulates, but decreases after tauopathies are severed. Some researchers have suggested that neuroinflammation occurs faster than amyloid pathology during the course of AD. However, to the best of our knowledge, studies related to temporal changes over time are limited, and further research is required to address this issue.
Neuroinflammation in brain diseases may be caused by the interaction between microglia and astrocytes rather than by the activation of the two alone. Most studies conducted to date have focused on in vivo changes in one biomarker and used it in a specific disease stage rather than in life-cycle studies. However, if further research using PET tracers for each biomarker is conducted, the role of temporal and causal interactions between the two glial components could also be identified. In addition, future studies should identify and verify reference issues that are specific to diseases. For AD, the cerebellum is proposed to be a pseudo-reference tissue, as the disease does not appear considerably in the cerebellum until it progresses. However, if a pathology affects the cerebellum, such as in multiple system atrophy or autoimmune encephalitis, another reference region should be identified. Lastly, determining the optimal scan time window after tracer injection through a comparative study of arterial input function-based and reference tissue-based dynamic scans could reduce the burden on subjects and contribute to clinical research.
Conclusion
Non-invasive in vivo evaluation of neuroinflammation based on activated glial cells is expected to play an important role in the course of neurodegenerative and psychiatric disorders, influencing the development of therapeutic drugs as well as determining disease severity and treatment methods. Despite the development of PET tracers based on several biomarkers, only a few drugs that can be used in clinical practice currently exist.
If research is conducted in the direction of 1) verifying validity by conducting multicenter clinical studies or follow-up studies using previously developed candidate PET tracers and 2) developing new PET tracers to overcome the difficulties highlighted in this review, promising PET radiopharmaceuticals that can be used in clinical practice could be available in the near future.
Data availability
Data sharing not applicable to this article as no datasets were generated in the current study.
Change history
27 August 2024
A Correction to this paper has been published: https://doi.org/10.1007/s13139-024-00880-3
References
Kempuraj D, Thangavel R, Natteru PA, Selvakumar GP, Saeed D, Zahoor H, et al. Neuroinflammation Induces Neurodegeneration. J Neurol Neurosurg Spine. 2016;1:1003.
Dong X. Current Strategies for Brain Drug Delivery. Theranostics. 2018;8:1481–93.
Sun YX, Minthon L, Wallmark A, Warkentin S, Blennow K, Janciauskiene S. Inflammatory markers in matched plasma and cerebrospinal fluid from patients with Alzheimer’s disease. Dement Geriatr Cogn Disord. 2003;16:136–44.
Shastri A, Bonifati DM, Kishore U. Innate immunity and neuroinflammation. Mediators Inflamm. 2013;2013: 342931.
Kwon HS, Koh SH. Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Transl Neurodegener. 2020;9:42.
Jellinger KA. Basic mechanisms of neurodegeneration: a critical update. J Cell Mol Med. 2010;14:457–87.
de Araujo Boleti AP, de Oliveira Flores TM, Moreno SE, Anjos LD, Mortari MR, Migliolo L. Neuroinflammation: An overview of neurodegenerative and metabolic diseases and of biotechnological studies. Neurochem Int. 2020;136: 104714.
MacRitchie N, Frleta-Gilchrist M, Sugiyama A, Lawton T, McInnes IB, Maffia P. Molecular imaging of inflammation - Current and emerging technologies for diagnosis and treatment. Pharmacol Ther. 2020;211: 107550.
Brosseron F, Krauthausen M, Kummer M, Heneka MT. Body fluid cytokine levels in mild cognitive impairment and Alzheimer’s disease: a comparative overview. Mol Neurobiol. 2014;50:534–44.
Morgan AR, Touchard S, Leckey C, O'Hagan C, Nevado-Holgado AJ, Consortium N et al. Inflammatory biomarkers in Alzheimer's disease plasma. Alzheimers Dement. 2019;15:776-87.
Nordengen K, Kirsebom BE, Henjum K, Selnes P, Gisladottir B, Wettergreen M, et al. Glial activation and inflammation along the Alzheimer’s disease continuum. J Neuroinflammation. 2019;16:46.
Cagnin A, Brooks DJ, Kennedy AM, Gunn RN, Myers R, Turkheimer FE, et al. In-vivo measurement of activated microglia in dementia. Lancet. 2001;358:461–7.
Edison P, Archer HA, Gerhard A, Hinz R, Pavese N, Turkheimer FE, et al. Microglia, amyloid, and cognition in Alzheimer’s disease: An [11C](R)PK11195-PET and [11C]PIB-PET study. Neurobiol Dis. 2008;32:412–9.
Vivash L, O’Brien TJ. Imaging Microglial Activation with TSPO PET: Lighting Up Neurologic Diseases? J Nucl Med. 2016;57:165–8.
Zhang L, Hu K, Shao T, Hou L, Zhang S, Ye W, Josephson L, Meyer JH, Zhang MR, Vasdev N, Wang J, Xu H, Wang L, Liang SH. Recent developments on PET radiotracers for TSPO and their applications in neuroimaging. Acta Pharm Sin B. 2021;11:373–93.
Venneti S, Wang G, Nguyen J, Wiley CA. The positron emission tomography ligand DAA1106 binds with high affinity to activated microglia in human neurological disorders. J Neuropathol Exp Neurol. 2008;67:1001–10.
Doorduin J, Klein HC, de Jong JR, Dierckx RA, de Vries EF. Evaluation of [11C]DAA1106 for imaging and quantification of neuroinflammation in a rat model of herpes encephalitis. Nucl Med Biol. 2010;37:9–15.
Doorduin J, Klein HC, Dierckx RA, James M, Kassiou M, de Vries EF. [11C]DPA-713 and [18F]DPA-714 as new PET tracers for TSPO: a comparison with [11C](R)-PK11195 in a rat model of herpes encephalitis. Mol Imaging Biol. 2009;11:386–98.
Yokokura M, Terada T, Bunai T, Nakaizumi K, Takebayashi K, Iwata Y, et al. Depiction of microglial activation in aging and dementia: Positron emission tomography with [11C]DPA713 versus [11C](R)PK11195. J Cereb Blood Flow Metab. 2017;37:877–89.
Singhal T, Cicero S, Pan H, Carter K, Dubey S, Chu R, et al. Regional microglial activation in the substantia nigra is linked with fatigue in MS. Neurol Neuroimmunol Neuroinflamm. 2020;7: e854.
Liu SY, Qiao HW, Song TB, Liu XL, Yao YX, Zhao CS, et al. Brain microglia activation and peripheral adaptive immunity in Parkinson’s disease: a multimodal PET study. J Neuroinflammation. 2022;19:209.
Kreisl WC, Lyoo CH, McGwier M, Snow J, Jenko KJ, Kimura N, et al. In vivo radioligand binding to translocator protein correlates with severity of Alzheimer’s disease. Brain. 2013;136:2228–38.
Alshikho MJ, Zurcher NR, Loggia ML, Cernasov P, Reynolds B, Pijanowski O, et al. Integrated magnetic resonance imaging and [11C]PBR28 positron emission tomographic imaging in amyotrophic lateral sclerosis. Ann Neurol. 2018;83:1186–97.
Felsky D, Roostaei T, Nho K, Risacher SL, Bradshaw EM, Petyuk V, et al. Neuropathological correlates and genetic architecture of microglial activation in elderly human brain. Nat Commun. 2019;10:409.
Hagens MHJ, Golla SV, Wijburg MT, Yaqub M, Heijtel D, Steenwijk MD, et al. In vivo assessment of neuroinflammation in progressive multiple sclerosis: a proof of concept study with [18F]DPA714 PET. J Neuroinflammation. 2018;15:314.
Hamelin L, Lagarde J, Dorothee G, Potier MC, Corlier F, Kuhnast B, et al. Distinct dynamic profiles of microglial activation are associated with progression of Alzheimer’s disease. Brain. 2018;141:1855–70.
Kobayashi M, Jiang T, Telu S, Zoghbi SS, Gunn RN, Rabiner EA, et al. 11C-DPA-713 has much greater specific binding to translocator protein 18 kDa (TSPO) in human brain than 11C-(R)-PK11195. J Cereb Blood Flow Metab. 2018;38:393–403.
Owen DR, Yeo AJ, Gunn RN, Song K, Wadsworth G, Lewis A, et al. An 18-kDa translocator protein (TSPO) polymorphism explains differences in binding affinity of the PET radioligand PBR28. J Cereb Blood Flow Metab. 2012;32:1–5.
Zanotti-Fregonara P, Pascual B, Veronese M, Yu M, Beers D, Appel SH, et al. Head-to-head comparison of 11C-PBR28 and 11C-ER176 for quantification of the translocator protein in the human brain. Eur J Nucl Med Mol Imaging. 2019;46:1822–9.
Albert NL, Unterrainer M, Fleischmann DF, Lindner S, Vettermann F, Brunegraf A, et al. TSPO PET for glioma imaging using the novel ligand 18F-GE-180: first results in patients with glioblastoma. Eur J Nucl Med Mol Imaging. 2017;44:2230–8.
Unterrainer M, Mahler C, Vomacka L, Lindner S, Havla J, Brendel M, et al. TSPO PET with [18F]GE-180 sensitively detects focal neuroinflammation in patients with relapsing-remitting multiple sclerosis. Eur J Nucl Med Mol Imaging. 2018;45:1423–31.
Kim SJW, Lupo JM, Chen Y, Pampaloni MH, VanBrocklin HF, Narvid J, et al. A feasibility study for quantitative assessment of cerebrovascular malformations using flutriciclamide ([18F]GE-180) PET/MRI. Front Med (Lausanne). 2023;10:1091463.
Ikawa M, Lohith TG, Shrestha S, Telu S, Zoghbi SS, Castellano S, et al. 11C-ER176, a Radioligand for 18-kDa Translocator Protein, Has Adequate Sensitivity to Robustly Image All Three Affinity Genotypes in Human Brain. J Nucl Med. 2017;58:320–5.
Vettermann FJ, Harris S, Schmitt J, Unterrainer M, Lindner S, Rauchmann BS, et al. Impact of TSPO Receptor Polymorphism on [18F]GE-180 Binding in Healthy Brain and Pseudo-Reference Regions of Neurooncological and Neurodegenerative Disorders. Life (Basel). 2021;11:484.
Lee SH, Denora N, Laquintana V, Mangiatordi GF, Lopedota A, Lopalco A, et al. Radiosynthesis and characterization of [18F]BS224: a next-generation TSPO PET ligand insensitive to the rs6971 polymorphism. Eur J Nucl Med Mol Imaging. 2021;49:110–24.
Rupprecht R, Papadopoulos V, Rammes G, Baghai TC, Fan J, Akula N, et al. Translocator protein (18 kDa) (TSPO) as a therapeutic target for neurological and psychiatric disorders. Nat Rev Drug Discov. 2010;9:971–88.
Hasko G, Pacher P, Vizi ES, Illes P. Adenosine receptor signaling in the brain immune system. Trends Pharmacol Sci. 2005;26:511–6.
Sheth S, Brito R, Mukherjea D, Rybak LP, Ramkumar V. Adenosine receptors: expression, function and regulation. Int J Mol Sci. 2014;15:2024–52.
Mishina M, Ishii K, Kimura Y, Suzuki M, Kitamura S, Ishibashi K et al. Adenosine A1 receptors measured with 11C-MPDX PET in early Parkinson's disease. Synapse. 2017;71.
Hayashi S, Inaji M, Nariai T, Oda K, Sakata M, Toyohara J, et al. Increased Binding Potential of Brain Adenosine A1 Receptor in Chronic Stages of Patients with Diffuse Axonal Injury Measured with [1-methyl-11C] 8-dicyclopropylmethyl-1-methyl-3-propylxanthine Positron Emission Tomography Imaging. J Neurotrauma. 2018;35:25–31.
Joya A, Ardaya M, Montilla A, Garbizu M, Plaza-Garcia S, Gomez-Vallejo V, et al. In vivo multimodal imaging of adenosine A1 receptors in neuroinflammation after experimental stroke. Theranostics. 2021;11:410–25.
Meyer PT, Elmenhorst D, Matusch A, Winz O, Zilles K, Bauer A. A1 adenosine receptor PET using [18F]CPFPX: displacement studies in humans. Neuroimage. 2006;32:1100–5.
Mishina M, Ishiwata K, Naganawa M, Kimura Y, Kitamura S, Suzuki M, et al. Adenosine A2A receptors measured with [11C]TMSX PET in the striata of Parkinson’s disease patients. PLoS One. 2011;6: e17338.
Rissanen E, Virta JR, Paavilainen T, Tuisku J, Helin S, Luoto P, et al. Adenosine A2A receptors in secondary progressive multiple sclerosis: a [11C]TMSX brain PET study. J Cereb Blood Flow Metab. 2013;33:1394–401.
Ramlackhansingh AF, Bose SK, Ahmed I, Turkheimer FE, Pavese N, Brooks DJ. Adenosine 2A receptor availability in dyskinetic and nondyskinetic patients with Parkinson disease. Neurology. 2011;76:1811–6.
Barret O, Hannestad J, Vala C, Alagille D, Tavares A, Laruelle M, et al. Characterization in humans of 18F-MNI-444, a PET radiotracer for brain adenosine 2A receptors. J Nucl Med. 2015;56:586–91.
Ishibashi K, Miura Y, Wagatsuma K, Toyohara J, Ishiwata K, Ishii K. Occupancy of adenosine A2A receptors by istradefylline in patients with Parkinson’s disease using 11C-preladenant PET. Neuropharmacology. 2018;143:106–12.
Pacher P, Mechoulam R. Is lipid signaling through cannabinoid 2 receptors part of a protective system? Prog Lipid Res. 2011;50:193–211.
Schmole AC, Lundt R, Gennequin B, Schrage H, Beins E, Kramer A, et al. Expression Analysis of CB2-GFP BAC Transgenic Mice. PLoS One. 2015;10: e0138986.
Benito C, Tolon RM, Pazos MR, Nunez E, Castillo AI, Romero J. Cannabinoid CB2 receptors in human brain inflammation. Br J Pharmacol. 2008;153:277–85.
Evens N, Bosier B, Lavey BJ, Kozlowski JA, Vermaelen P, Baudemprez L, et al. Labelling and biological evaluation of [11C]methoxy-Sch225336: a radioligand for the cannabinoid-type 2 receptor. Nucl Med Biol. 2008;35:793–800.
Evens N, Vandeputte C, Coolen C, Janssen P, Sciot R, Baekelandt V, et al. Preclinical evaluation of [11C]NE40, a type 2 cannabinoid receptor PET tracer. Nucl Med Biol. 2012;39:389–99.
Ahmad R, Postnov A, Bormans G, Versijpt J, Vandenbulcke M, Van Laere K. Decreased in vivo availability of the cannabinoid type 2 receptor in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2016;43:2219–27.
Horti AG, Gao Y, Ravert HT, Finley P, Valentine H, Wong DF, et al. Synthesis and biodistribution of [11C]A-836339, a new potential radioligand for PET imaging of cannabinoid type 2 receptors (CB2). Bioorg Med Chem. 2010;18:5202–7.
Pottier G, Gomez-Vallejo V, Padro D, Boisgard R, Dolle F, Llop J, et al. PET imaging of cannabinoid type 2 receptors with [11C]A-836339 did not evidence changes following neuroinflammation in rats. J Cereb Blood Flow Metab. 2017;37:1163–78.
Vandeputte C, Casteels C, Struys T, Koole M, van Veghel D, Evens N, et al. Small-animal PET imaging of the type 1 and type 2 cannabinoid receptors in a photothrombotic stroke model. Eur J Nucl Med Mol Imaging. 2012;39:1796–806.
Valenzano KJ, Tafesse L, Lee G, Harrison JE, Boulet JM, Gottshall SL, et al. Pharmacological and pharmacokinetic characterization of the cannabinoid receptor 2 agonist, GW405833, utilizing rodent models of acute and chronic pain, anxiety, ataxia and catalepsy. Neuropharmacology. 2005;48:658–72.
Vandeputte C, Evens N, Toelen J, Deroose CM, Bosier B, Ibrahimi A, et al. A PET brain reporter gene system based on type 2 cannabinoid receptors. J Nucl Med. 2011;52:1102–9.
Ahamed M, van Veghel D, Ullmer C, Van Laere K, Verbruggen A, Bormans GM. Synthesis, Biodistribution and In vitro Evaluation of Brain Permeable High Affinity Type 2 Cannabinoid Receptor Agonists [11C]MA2 and [18F]MA3. Front Neurosci. 2016;10:431.
Attili B, Celen S, Ahamed M, Koole M, Haute CVD, Vanduffel W, et al. Preclinical evaluation of [18F]MA3: a CB(2) receptor agonist radiotracer for PET. Br J Pharmacol. 2019;176:1481–91.
Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van De Putte LB, et al. Cyclooxygenase in biology and disease. FASEB J. 1998;12:1063–73.
Choi SH, Aid S, Bosetti F. The distinct roles of cyclooxygenase-1 and -2 in neuroinflammation: implications for translational research. Trends Pharmacol Sci. 2009;30:174–81.
Shukuri M, Takashima-Hirano M, Tokuda K, Takashima T, Matsumura K, Inoue O, et al. In vivo expression of cyclooxygenase-1 in activated microglia and macrophages during neuroinflammation visualized by PET with 11C-ketoprofen methyl ester. J Nucl Med. 2011;52:1094–101.
Ohnishi A, Senda M, Yamane T, Mikami T, Nishida H, Nishio T, et al. Exploratory human PET study of the effectiveness of 11C-ketoprofen methyl ester, a potential biomarker of neuroinflammatory processes in Alzheimer’s disease. Nucl Med Biol. 2016;43:438–44.
Kim MJ, Shrestha SS, Cortes M, Singh P, Morse C, Liow JS, et al. Evaluation of Two Potent and Selective PET Radioligands to Image COX-1 and COX-2 in Rhesus Monkeys. J Nucl Med. 2018;59:1907–12.
Kim MJ, Anaya FJ, Manly LS, Lee JH, Hong J, Shrestha S, et al. Whole-Body PET Imaging in Humans Shows That 11C-PS13 Is Selective for Cyclooxygenase-1 and Can Measure the In Vivo Potency of Nonsteroidal Antiinflammatory Drugs. J Nucl Med. 2023;64:159–64.
Zhao YF, Tang Y, Illes P. Astrocytic and Oligodendrocytic P2X7 Receptors Determine Neuronal Functions in the CNS. Front Mol Neurosci. 2021;14: 641570.
Ory D, Celen S, Gijsbers R, Van Den Haute C, Postnov A, Koole M, et al. Preclinical Evaluation of a P2X7 Receptor-Selective Radiotracer: PET Studies in a Rat Model with Local Overexpression of the Human P2X7 Receptor and in Nonhuman Primates. J Nucl Med. 2016;57:1436–41.
Van Weehaeghe D, Koole M, Schmidt ME, Deman S, Jacobs AH, Souche E, et al. [11C]JNJ54173717, a novel P2X7 receptor radioligand as marker for neuroinflammation: human biodistribution, dosimetry, brain kinetic modelling and quantification of brain P2X7 receptors in patients with Parkinson’s disease and healthy volunteers. Eur J Nucl Med Mol Imaging. 2019;46:2051–64.
Berdyyeva T, Xia C, Taylor N, He Y, Chen G, Huang C, et al. PET Imaging of the P2X7 Ion Channel with a Novel Tracer [18F]JNJ-64413739 in a Rat Model of Neuroinflammation. Mol Imaging Biol. 2019;21:871–8.
Koole M, Schmidt ME, Hijzen A, Ravenstijn P, Vandermeulen C, Van Weehaeghe D, et al. 18F-JNJ-64413739, a Novel PET Ligand for the P2X7 Ion Channel: Radiation Dosimetry, Kinetic Modeling, Test-Retest Variability, and Occupancy of the P2X7 Antagonist JNJ-54175446. J Nucl Med. 2019;60:683–90.
Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S, et al. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science. 2010;330:841–5.
Tanzey SS, Shao X, Stauff J, Arteaga J, Sherman P, Scott PJH, et al. Synthesis and Initial In Vivo Evaluation of [11C]AZ683-A Novel PET Radiotracer for Colony Stimulating Factor 1 Receptor (CSF1R). Pharmaceuticals (Basel). 2018;11:136.
Horti AG, Naik R, Foss CA, Minn I, Misheneva V, Du Y, et al. PET imaging of microglia by targeting macrophage colony-stimulating factor 1 receptor (CSF1R). Proc Natl Acad Sci U S A. 2019;116:1686–91.
Knight AC, Varlow C, Zi T, Liang SH, Josephson L, Schmidt K, et al. In Vitro Evaluation of [3H]CPPC as a Tool Radioligand for CSF-1R. ACS Chem Neurosci. 2021;12:998–1006.
Kawamura K, Maeda J, Hatori A, Okauchi T, Nagai Y, Higuchi M, et al. In vivo and in vitro imaging of I2 imidazoline receptors in the monkey brain. Synapse. 2011;65:452–5.
Kawamura K, Naganawa M, Konno F, Yui J, Wakizaka H, Yamasaki T, et al. Imaging of I2-imidazoline receptors by small-animal PET using 2-(3-fluoro-[4-11C]tolyl)-4,5-dihydro-1H-imidazole ([11C]FTIMD). Nucl Med Biol. 2010;37:625–35.
Kawamura K, Kimura Y, Yui J, Wakizaka H, Yamasaki T, Hatori A, et al. PET study using [11C]FTIMD with ultra-high specific activity to evaluate I2-imidazoline receptors binding in rat brains. Nucl Med Biol. 2012;39:199–206.
Kawamura K, Shimoda Y, Kumata K, Fujinaga M, Yui J, Yamasaki T, et al. In vivo evaluation of a new 18F-labeled PET ligand, [18F]FEBU, for the imaging of I2-imidazoline receptors. Nucl Med Biol. 2015;42:406–12.
Kawamura K, Yui J, Konno F, Yamasaki T, Hatori A, Wakizaka H, et al. Synthesis and evaluation of PET probes for the imaging of I2 imidazoline receptors in peripheral tissues. Nucl Med Biol. 2012;39:89–99.
Tyacke RJ, Myers JFM, Venkataraman A, Mick I, Turton S, Passchier J, et al. Evaluation of 11C-BU99008, a PET Ligand for the Imidazoline2 Binding Site in Human Brain. J Nucl Med. 2018;59:1597–602.
Wilson H, Dervenoulas G, Pagano G, Tyacke RJ, Polychronis S, Myers J, et al. Imidazoline 2 binding sites reflecting astroglia pathology in Parkinson’s disease: an in vivo 11C-BU99008 PET study. Brain. 2019;142:3116–28.
Mohamed MA, Zeng Z, Gennaro M, Lao-Kaim NP, Myers JFM, Calsolaro V et al. Astrogliosis in aging and Parkinson's disease dementia: a new clinical study with 11C-BU99008 PET. Brain Commun. 2022;4:fcac199.
Calsolaro V, Matthews PM, Donat CK, Livingston NR, Femminella GD, Guedes SS, et al. Astrocyte reactivity with late-onset cognitive impairment assessed in vivo using 11C-BU99008 PET and its relationship with amyloid load. Mol Psychiatry. 2021;26:5848–55.
Livingston NR, Calsolaro V, Hinz R, Nowell J, Raza S, Gentleman S, et al. Relationship between astrocyte reactivity, using novel 11C-BU99008 PET, and glucose metabolism, grey matter volume and amyloid load in cognitively impaired individuals. Mol Psychiatry. 2022;27:2019–29.
Levitt P, Pintar JE, Breakefield XO. Immunocytochemical demonstration of monoamine oxidase B in brain astrocytes and serotonergic neurons. Proc Natl Acad Sci U S A. 1982;79:6385–9.
Fowler JS, MacGregor RR, Wolf AP, Arnett CD, Dewey SL, Schlyer D, et al. Mapping human brain monoamine oxidase A and B with 11C-labeled suicide inactivators and PET. Science. 1987;235:481–5.
Fowler JS, Wolf AP, MacGregor RR, Dewey SL, Logan J, Schlyer DJ, et al. Mechanistic positron emission tomography studies: demonstration of a deuterium isotope effect in the monoamine oxidase-catalyzed binding of [11C]L-deprenyl in living baboon brain. J Neurochem. 1988;51:1524–34.
Rusjan PM, Wilson AA, Miler L, Fan I, Mizrahi R, Houle S et al. Kinetic modeling of the monoamine oxidase B radioligand [11C]SL25.1188 in human brain with high-resolution positron emission tomography. J Cereb Blood Flow Metab. 2014;34:883-9.
Moriguchi S, Wilson AA, Miler L, Rusjan PM, Vasdev N, Kish SJ et al. Monoamine Oxidase B Total Distribution Volume in the Prefrontal Cortex of Major Depressive Disorder: An [11C]SL25.1188 Positron Emission Tomography Study. JAMA Psychiatry. 2019;76:634-41.
Gill T, Watling SE, Richardson JD, McCluskey T, Tong J, Meyer JH et al. Imaging of astrocytes in posttraumatic stress disorder: A PET study with the monoamine oxidase B radioligand [11C]SL25.1188. Eur Neuropsychopharmacol. 2022;54:54-61.
Koshimori Y, Cusimano MD, Vieira EL, Rusjan PM, Kish SJ, Vasdev N et al. Astrogliosis marker 11C-SL2511.88 PET in traumatic brain injury with persistent symptoms. Brain. 2023:awad279.
Ballweg A, Klaus C, Vogler L, Katzdobler S, Wind K, Zatcepin A, et al. [18F]F-DED PET imaging of reactive astrogliosis in neurodegenerative diseases: preclinical proof of concept and first-in-human data. J Neuroinflammation. 2023;20:68.
Dahl K, Bernard-Gauthier V, Nag S, Varnas K, Narayanaswami V, Mahdi Moein M et al. Synthesis and preclinical evaluation of [18F]FSL25.1188, a reversible PET radioligand for monoamine oxidase-B. Bioorg Med Chem Lett. 2019;29:1624-7.
Harada R, Hayakawa Y, Ezura M, Lerdsirisuk P, Du Y, Ishikawa Y, et al. 18F-SMBT-1: A Selective and Reversible PET Tracer for Monoamine Oxidase-B Imaging. J Nucl Med. 2021;62:253–8.
Villemagne VL, Harada R, Dore V, Furumoto S, Mulligan R, Kudo Y, et al. Assessing Reactive Astrogliosis with 18F-SMBT-1 Across the Alzheimer Disease Spectrum. J Nucl Med. 2022;63:1560–9.
Chatterjee P, Dore V, Pedrini S, Krishnadas N, Thota R, Bourgeat P, et al. Plasma Glial Fibrillary Acidic Protein Is Associated with 18F-SMBT-1 PET: Two Putative Astrocyte Reactivity Biomarkers for Alzheimer’s Disease. J Alzheimers Dis. 2023;92:615–28.
Galatro TF, Holtman IR, Lerario AM, Vainchtein ID, Brouwer N, Sola PR, et al. Transcriptomic analysis of purified human cortical microglia reveals age-associated changes. Nat Neurosci. 2017;20:1162–71.
Gosselin D, Skola D, Coufal NG, Holtman IR, Schlachetzki JCM, Sajti E et al. An environment-dependent transcriptional network specifies human microglia identity. Science. 2017;356:eaal3222.
Oberheim NA, Goldman SA, Nedergaard M. Heterogeneity of astrocytic form and function. Methods Mol Biol. 2012;814:23–45.
Tarassishin L, Suh HS, Lee SC. LPS and IL-1 differentially activate mouse and human astrocytes: role of CD14. Glia. 2014;62:999–1013.
Zhang Y, Sloan SA, Clarke LE, Caneda C, Plaza CA, Blumenthal PD, et al. Purification and Characterization of Progenitor and Mature Human Astrocytes Reveals Transcriptional and Functional Differences with Mouse. Neuron. 2016;89:37–53.
Camsonne R, Crouzel C, Comar D, Mazi6re M, Prenant C, Sastre J et al. Synthesis of N-(11C) methyl, N-(methyl-1 propyl), (chloro-2 phenyl)-1 isoquinoleine carboxamide-3 (PK 11195): A new ligand for peripheral benzodiazepine receptors. J Label Compd Radiopharm. 1984;21:985-91.
Schroeter M, Dennin MA, Walberer M, Backes H, Neumaier B, Fink GR, et al. Neuroinflammation extends brain tissue at risk to vital peri-infarct tissue: a double tracer [11C]PK11195- and [18F]FDG-PET study. J Cereb Blood Flow Metab. 2009;29:1216–25.
Becker G, Debatisse J, Riviere M, Crola Da Silva C, Beaudoin-Gobert M, Eker O et al. Spatio-Temporal Characterization of Brain Inflammation in a Non-human Primate Stroke Model Mimicking Endovascular Thrombectomy. Neurotherapeutics. 2023;20:789-802.
Debruyne JC, Versijpt J, Van Laere KJ, De Vos F, Keppens J, Strijckmans K, et al. PET visualization of microglia in multiple sclerosis patients using [11C]PK11195. Eur J Neurol. 2003;10:257–64.
Zhang MR, Kida T, Noguchi J, Furutsuka K, Maeda J, Suhara T, et al. [11C]DAA1106: radiosynthesis and in vivo binding to peripheral benzodiazepine receptors in mouse brain. Nucl Med Biol. 2003;30:513–9.
Maeda J, Suhara T, Zhang MR, Okauchi T, Yasuno F, Ikoma Y, et al. Novel peripheral benzodiazepine receptor ligand [11C]DAA1106 for PET: an imaging tool for glial cells in the brain. Synapse. 2004;52:283–91.
Yasuno F, Ota M, Kosaka J, Ito H, Higuchi M, Doronbekov TK, et al. Increased binding of peripheral benzodiazepine receptor in Alzheimer’s disease measured by positron emission tomography with [11C]DAA1106. Biol Psychiatry. 2008;64:835–41.
James ML, Fulton RR, Henderson DJ, Eberl S, Meikle SR, Thomson S, et al. Synthesis and in vivo evaluation of a novel peripheral benzodiazepine receptor PET radioligand. Bioorg Med Chem. 2005;13:6188–94.
Chauveau F, Van Camp N, Dolle F, Kuhnast B, Hinnen F, Damont A, et al. Comparative evaluation of the translocator protein radioligands [11C]DPA-713, [18F]DPA-714, and [11C]PK11195 in a rat model of acute neuroinflammation. J Nucl Med. 2009;50:468–76.
Tsukada H, Nishiyama S, Ohba H, Kanazawa M, Kakiuchi T, Harada N. Comparing amyloid-beta deposition, neuroinflammation, glucose metabolism, and mitochondrial complex I activity in brain: a PET study in aged monkeys. Eur J Nucl Med Mol Imaging. 2014;41:2127–36.
Endres CJ, Pomper MG, James M, Uzuner O, Hammoud DA, Watkins CC, et al. Initial evaluation of 11C-DPA-713, a novel TSPO PET ligand, in humans. J Nucl Med. 2009;50:1276–82.
Imaizumi M, Briard E, Zoghbi SS, Gourley JP, Hong J, Musachio JL, et al. Kinetic evaluation in nonhuman primates of two new PET ligands for peripheral benzodiazepine receptors in brain. Synapse. 2007;61:595–605.
Lartey FM, Ahn GO, Shen B, Cord KT, Smith T, Chua JY, et al. PET imaging of stroke-induced neuroinflammation in mice using [18F]PBR06. Mol Imaging Biol. 2014;16:109–17.
Fujimura Y, Zoghbi SS, Simeon FG, Taku A, Pike VW, Innis RB, et al. Quantification of translocator protein (18 kDa) in the human brain with PET and a novel radioligand, [18F]PBR06. J Nucl Med. 2009;50:1047–53.
Briard E, Zoghbi SS, Imaizumi M, Gourley JP, Shetty HU, Hong J, et al. Synthesis and evaluation in monkey of two sensitive 11C-labeled aryloxyanilide ligands for imaging brain peripheral benzodiazepine receptors in vivo. J Med Chem. 2008;51:17–30.
Imaizumi M, Kim HJ, Zoghbi SS, Briard E, Hong J, Musachio JL, et al. PET imaging with [11C]PBR28 can localize and quantify upregulated peripheral benzodiazepine receptors associated with cerebral ischemia in rat. Neurosci Lett. 2007;411:200–5.
Imaizumi M, Briard E, Zoghbi SS, Gourley JP, Hong J, Fujimura Y, et al. Brain and whole-body imaging in nonhuman primates of [11C]PBR28, a promising PET radioligand for peripheral benzodiazepine receptors. Neuroimage. 2008;39:1289–98.
Zanotti-Fregonara P, Pascual B, Rizzo G, Yu M, Pal N, Beers D, et al. Head-to-Head Comparison of [11C]PBR28 and [18F]GE180 for Quantification of the Translocator Protein in the Human Brain. J Nucl Med. 2018;59:1260–6.
James ML, Fulton RR, Vercoullie J, Henderson DJ, Garreau L, Chalon S, et al. DPA-714, a new translocator protein-specific ligand: synthesis, radiofluorination, and pharmacologic characterization. J Nucl Med. 2008;49:814–22.
Arlicot N, Vercouillie J, Ribeiro MJ, Tauber C, Venel Y, Baulieu JL, et al. Initial evaluation in healthy humans of [18F]DPA-714, a potential PET biomarker for neuroinflammation. Nucl Med Biol. 2012;39:570–8.
Wadsworth H, Jones PA, Chau WF, Durrant C, Fouladi N, Passmore J, et al. [18F]GE-180: a novel fluorine-18 labelled PET tracer for imaging Translocator protein 18 kDa (TSPO). Bioorg Med Chem Lett. 2012;22:1308–13.
Liu B, Le KX, Park MA, Wang S, Belanger AP, Dubey S, et al. In Vivo Detection of Age- and Disease-Related Increases in Neuroinflammation by [18F]GE180 TSPO MicroPET Imaging in Wild-Type and Alzheimer’s Transgenic Mice. J Neurosci. 2015;35:15716–30.
Lee JH, Simeon FG, Liow JS, Morse CL, Gladding RL, Santamaria JAM, et al. In Vivo Evaluation of 6 Analogs of 11C-ER176 as Candidate 18F-Labeled Radioligands for 18-kDa Translocator Protein. J Nucl Med. 2022;63:1252–8.
Simeon FG, Lee JH, Morse CL, Stukes I, Zoghbi SS, Manly LS, et al. Synthesis and Screening in Mice of Fluorine-Containing PET Radioligands for TSPO: Discovery of a Promising 18F-Labeled Ligand. J Med Chem. 2021;64:16731–45.
Zanotti-Fregonara P, Zhang Y, Jenko KJ, Gladding RL, Zoghbi SS, Fujita M, et al. Synthesis and evaluation of translocator 18 kDa protein (TSPO) positron emission tomography (PET) radioligands with low binding sensitivity to human single nucleotide polymorphism rs6971. ACS Chem Neurosci. 2014;5:963–71.
Ishiwata K, Noguchi J, Wakabayashi S, Shimada J, Ogi N, Nariai T, et al. 11C-labeled KF18446: a potential central nervous system adenosine A2A receptor ligand. J Nucl Med. 2000;41:345–54.
Mishina M, Ishiwata K, Kimura Y, Naganawa M, Oda K, Kobayashi S, et al. Evaluation of distribution of adenosine A2A receptors in normal human brain measured with [11C]TMSX PET. Synapse. 2007;61:778–84.
Todde S, Moresco RM, Simonelli P, Baraldi PG, Cacciari B, Spalluto G, et al. Design, radiosynthesis, and biodistribution of a new potent and selective ligand for in vivo imaging of the adenosine A2A receptor system using positron emission tomography. J Med Chem. 2000;43:4359–62.
Moresco RM, Todde S, Belloli S, Simonelli P, Panzacchi A, Rigamonti M, et al. In vivo imaging of adenosine A2A receptors in rat and primate brain using [11C]SCH442416. Eur J Nucl Med Mol Imaging. 2005;32:405–13.
Marques TR, Natesan S, Rabiner EA, Searle GE, Gunn R, Howes OD, et al. Adenosine A2A receptor in schizophrenia: an in vivo brain PET imaging study. Psychopharmacology (Berl). 2022;239:3439–45.
Ishiwata K, Nariai T, Kimura Y, Oda K, Kawamura K, Ishii K, et al. Preclinical studies on [11C]MPDX for mapping adenosine A1 receptors by positron emission tomography. Ann Nucl Med. 2002;16:377–82.
Fukumitsu N, Ishii K, Kimura Y, Oda K, Sasaki T, Mori Y, et al. Imaging of adenosine A1 receptors in the human brain by positron emission tomography with [11C]MPDX. Ann Nucl Med. 2003;17:511–5.
Holschbach MH, Olsson RA, Bier D, Wutz W, Sihver W, Schuller M, et al. Synthesis and evaluation of no-carrier-added 8-cyclopentyl-3-(3-[18F]fluoropropyl)-1-propylxanthine ([18F]CPFPX): a potent and selective A1-adenosine receptor antagonist for in vivo imaging. J Med Chem. 2002;45:5150–6.
Bauer A, Holschbach MH, Cremer M, Weber S, Boy C, Shah NJ, et al. Evaluation of 18F-CPFPX, a novel adenosine A1 receptor ligand: in vitro autoradiography and high-resolution small animal PET. J Nucl Med. 2003;44:1682–9.
Bauer A, Holschbach MH, Meyer PT, Boy C, Herzog H, Olsson RA, et al. In vivo imaging of adenosine A1 receptors in the human brain with [18F]CPFPX and positron emission tomography. Neuroimage. 2003;19:1760–9.
Zhou X, Khanapur S, Huizing AP, Zijlma R, Schepers M, Dierckx RA, et al. Synthesis and preclinical evaluation of 2-(2-furanyl)-7-[2-[4-[4-(2-[11C]methoxyethoxy)phenyl]-1-piperazinyl]ethyl]7H-pyrazolo[4,3-e][1,2,4]triazolo[1,5-c]pyrimidine-5-amine ([11C]Preladenant) as a PET tracer for the imaging of cerebral adenosine A2A receptors. J Med Chem. 2014;57:9204–10.
Zhou X, Boellaard R, Ishiwata K, Sakata M, Dierckx R, de Jong JR, et al. In Vivo Evaluation of 11C-Preladenant for PET Imaging of Adenosine A2A Receptors in the Conscious Monkey. J Nucl Med. 2017;58:762–7.
Ishibashi K, Miura Y, Wagatsuma K, Toyohara J, Ishiwata K, Ishii K. Adenosine A2A Receptor Occupancy by Caffeine After Coffee Intake in Parkinson’s Disease. Mov Disord. 2022;37:853–7.
Barret O, Hannestad J, Alagille D, Vala C, Tavares A, Papin C, et al. Adenosine 2A receptor occupancy by tozadenant and preladenant in rhesus monkeys. J Nucl Med. 2014;55:1712–8.
Vala C, Morley TJ, Zhang X, Papin C, Tavares AA, Lee HS, et al. Synthesis and in vivo Evaluation of Fluorine-18 and Iodine-123 Pyrazolo[4,3-e]-1,2,4-triazolo[1,5-c]pyrimidine Derivatives as PET and SPECT Radiotracers for Mapping A2A Receptors. ChemMedChem. 2016;11:1936–43.
Evens N, Muccioli GG, Houbrechts N, Lambert DM, Verbruggen AM, Van Laere K, et al. Synthesis and biological evaluation of carbon-11- and fluorine-18-labeled 2-oxoquinoline derivatives for type 2 cannabinoid receptor positron emission tomography imaging. Nucl Med Biol. 2009;36:455–65.
Takashima-Hirano M, Shukuri M, Takashima T, Goto M, Wada Y, Watanabe Y, et al. General method for the 11C-labeling of 2-arylpropionic acids and their esters: construction of a PET tracer library for a study of biological events involved in COXs expression. Chemistry. 2010;16:4250–8.
Ohnishi A, Senda M, Yamane T, Sasaki M, Mikami T, Nishio T, et al. Human whole-body biodistribution and dosimetry of a new PET tracer, [11C]ketoprofen methyl ester, for imagings of neuroinflammation. Nucl Med Biol. 2014;41:594–9.
Singh P, Shrestha S, Cortes-Salva MY, Jenko KJ, Zoghbi SS, Morse CL et al. 3-Substituted 1,5-Diaryl-1 H-1,2,4-triazoles as Prospective PET Radioligands for Imaging Brain COX-1 in Monkey. Part 1: Synthesis and Pharmacology. ACS Chem Neurosci. 2018;9:2610-9.
Kim MJ, Lee JH, Juarez Anaya F, Hong J, Miller W, Telu S, et al. First-in-human evaluation of [11C]PS13, a novel PET radioligand, to quantify cyclooxygenase-1 in the brain. Eur J Nucl Med Mol Imaging. 2020;47:3143–51.
Shrestha S, Kim MJ, Eldridge M, Lehmann ML, Frankland M, Liow JS, et al. PET measurement of cyclooxygenase-2 using a novel radioligand: upregulation in primate neuroinflammation and first-in-human study. J Neuroinflammation. 2020;17:140.
Kolb HC, Barret O, Bhattacharya A, Chen G, Constantinescu C, Huang C, et al. Preclinical Evaluation and Nonhuman Primate Receptor Occupancy Study of 18F-JNJ-64413739, a PET Radioligand for P2X7 Receptors. J Nucl Med. 2019;60:1154–9.
Coughlin JM, Du Y, Lesniak WG, Harrington CK, Brosnan MK, O’Toole R, et al. First-in-human use of 11C-CPPC with positron emission tomography for imaging the macrophage colony-stimulating factor 1 receptor. EJNMMI Res. 2022;12:64.
Kealey S, Turner EM, Husbands SM, Salinas CA, Jakobsen S, Tyacke RJ, et al. Imaging imidazoline-I2 binding sites in porcine brain using 11C-BU99008. J Nucl Med. 2013;54:139–44.
Kawamura K, Yamasaki T, Zhang Y, Wakizaka H, Hatori A, Xie L, et al. Change in the Binding of [11C]BU99008 to Imidazoline I2 Receptor Using Brain PET in Zucker Rats. Mol Imaging Biol. 2019;21:105–12.
Parker CA, Nabulsi N, Holden D, Lin SF, Cass T, Labaree D, et al. Evaluation of 11C-BU99008, a PET ligand for the imidazoline2 binding sites in rhesus brain. J Nucl Med. 2014;55:838–44.
Venkataraman AV, Keat N, Myers JF, Turton S, Mick I, Gunn RN, et al. First evaluation of PET-based human biodistribution and radiation dosimetry of 11C-BU99008, a tracer for imaging the imidazoline2 binding site. EJNMMI Res. 2018;8:71.
Bench CJ, Price GW, Lammertsma AA, Cremer JC, Luthra SK, Turton D, et al. Measurement of human cerebral monoamine oxidase type B (MAO-B) activity with positron emission tomography (PET): a dose ranging study with the reversible inhibitor Ro 19–6327. Eur J Clin Pharmacol. 1991;40:169–73.
Rodriguez-Vieitez E, Ni R, Gulyas B, Toth M, Haggkvist J, Halldin C, et al. Astrocytosis precedes amyloid plaque deposition in Alzheimer APPswe transgenic mouse brain: a correlative positron emission tomography and in vitro imaging study. Eur J Nucl Med Mol Imaging. 2015;42:1119–32.
Arakawa R, Stenkrona P, Takano A, Nag S, Maior RS, Halldin C. Test-retest reproducibility of [11C]-L-deprenyl-D2 binding to MAO-B in the human brain. EJNMMI Res. 2017;7:54.
Bramoullé Y, Puech F, Saba W, Valette H, Bottlaender M, George P et al. Radiosynthesis of (S)-5-methoxymethyl-3-[6-(4,4,4-trifluorobutoxy)benzo[d]isoxazol-3-yl] oxazolidin-2-[11C]one ([11C]SL25.1188), a novel radioligand for imaging monoamine oxidase-B with PET. Journal of Labelled Compounds and Radiopharmaceuticals. 2008;51:153-8.
Saba W, Valette H, Peyronneau MA, Bramoulle Y, Coulon C, Curet O et al. [11C]SL25.1188, a new reversible radioligand to study the monoamine oxidase type B with PET: preclinical characterisation in nonhuman primate. Synapse. 2010;64:61-9.
Nag S, Fazio P, Lehmann L, Kettschau G, Heinrich T, Thiele A, et al. In Vivo and In Vitro Characterization of a Novel MAO-B Inhibitor Radioligand, 18F-Labeled Deuterated Fluorodeprenyl. J Nucl Med. 2016;57:315–20.
Villemagne VL, Harada R, Dore V, Furumoto S, Mulligan R, Kudo Y, et al. First-in-Humans Evaluation of 18F-SMBT-1, a Novel 18F-Labeled Monoamine Oxidase-B PET Tracer for Imaging Reactive Astrogliosis. J Nucl Med. 2022;63:1551–9.
Fan Z, Calsolaro V, Atkinson RA, Femminella GD, Waldman A, Buckley C, et al. Flutriciclamide (18F-GE180) PET: First-in-Human PET Study of Novel Third-Generation In Vivo Marker of Human Translocator Protein. J Nucl Med. 2016;57:1753–9.
Feeney C, Scott G, Raffel J, Roberts S, Coello C, Jolly A, et al. Kinetic analysis of the translocator protein positron emission tomography ligand [18F]GE-180 in the human brain. Eur J Nucl Med Mol Imaging. 2016;43:2201–10.
Sakata M, Ishibashi K, Imai M, Wagatsuma K, Ishii K, Zhou X, et al. Initial Evaluation of an Adenosine A2A Receptor Ligand, 11C-Preladenant, in Healthy Human Subjects. J Nucl Med. 2017;58:1464–70.
Acknowledgements
In this paper, we used figures from the previously published papers to help readers understand. Fig. 2. was published in “Exploratory human PET study of the effectiveness of 11C-ketoprofen methyl ester, a potential biomarker of neuroinflammatory processes in Alzheimer's disease.” Nucl Med Biol 2016;43:438 and reprint permission was obtained from Elsevier. The articles containing Fig. 3 and Fig. 4. were licensed under the Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction. Fig. 3. was published in “Relationship between astrocyte reactivity, using novel 11C-BU99008 PET, and glucose metabolism, grey matter volume and amyloid load in cognitively impaired individuals.” Mol Psychiatry 2022;27:2019. Fig. 4. was published in “[18F]F-DED PET imaging of reactive astrogliosis in neurodegenerative diseases: preclinical proof of concept and first-in-human data.” J Neuroinflammation 2023;20:68. Fig 5. was originally published in “Assessing Reactive Astrogliosis with 18F-SMBT-1 Across the Alzheimer Disease Spectrum” J Nucl Med 2022;63:1560.
Funding
This study was supported by a grant from the Korea Institute of Radiological and Medical Sciences (KIRAMS), the Ministry of Science and ICT (MSIT), Republic of Korea (No. 50461–2023), and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2020R1A2C2008618).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Namhun Lee, Jae Yong Choi, and Young Hoon Ryu declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required and informed consent is not applicable.
Consent for publication
The participants signed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, N., Choi, J.Y. & Ryu, Y.H. The development status of PET radiotracers for evaluating neuroinflammation. Nucl Med Mol Imaging 58, 160–176 (2024). https://doi.org/10.1007/s13139-023-00831-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-023-00831-4