Abstract
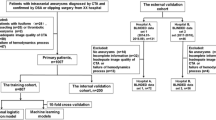
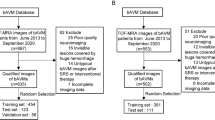
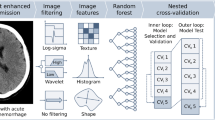
This study aimed to develop a machine learning model for predicting brain arteriovenous malformation (bAVM) rupture using a combination of traditional risk factors and radiomics features. This multicenter retrospective study enrolled 586 patients with unruptured bAVMs from 2010 to 2020. All patients were grouped into the hemorrhage (n = 368) and non-hemorrhage (n = 218) groups. The bAVM nidus were segmented on CT angiography images using Slicer software, and radiomic features were extracted using Pyradiomics. The dataset included a training set and an independent testing set. The machine learning model was developed on the training set and validated on the testing set by merging numerous base estimators and a final estimator based on the stacking method. The area under the receiver operating characteristic (ROC) curve, precision, and the f1 score were evaluated to determine the performance of the model. A total of 1790 radiomics features and 8 traditional risk factors were contained in the original dataset, and 241 features remained for model training after L1 regularization filtering. The base estimator of the ensemble model was Logistic Regression, whereas the final estimator was Random Forest. In the training set, the area under the ROC curve of the model was 0.982 (0.967–0.996) and 0.893 (0.826–0.960) in the testing set. This study indicated that radiomics features are a valuable addition to traditional risk factors for predicting bAVM rupture. In the meantime, ensemble learning can effectively improve the performance of a prediction model.






Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Lawton MT, Rutledge WC, Kim H, et al. Brain arteriovenous malformations. Nat Rev Dis Primers. 2015;1:15008. https://doi.org/10.1038/nrdp.2015.8.
Kim H, Al-Shahi Salman R, McCulloch CE, et al. Untreated brain arteriovenous malformation: patient-level meta-analysis of hemorrhage predictors. Neurology. 2014;83:590–7. https://doi.org/10.1212/WNL.0000000000000688.
Hernesniemi JA, Dashti R, Juvela S, et al. Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurg. 2008;63:823–9. https://doi.org/10.1227/01.NEU.0000330401.82582.5E.
Mohr JP, Parides MK, Stapf C, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. The Lancet. 2014;383:614–21. https://doi.org/10.1016/S0140-6736(13)62302-8.
Mohr JP, Overbey JR, Hartmann A, et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 2020;19:573–81. https://doi.org/10.1016/S1474-4422(20)30181-2.
Kim H, Sidney S, McCulloch CE, et al. Racial/Ethnic differences in longitudinal risk of intracranial hemorrhage in brain arteriovenous malformation patients. Stroke. 2007;38:2430–7. https://doi.org/10.1161/STROKEAHA.107.485573.
Guo Y, Saunders T, Su H, et al. Silent intralesional microhemorrhage as a risk factor for brain arteriovenous malformation rupture. Stroke. 2012;43:1240–6. https://doi.org/10.1161/STROKEAHA.111.647263.
Thompson KP, Nelson J, Kim H, et al. Predictors of mortality in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2021;16:12. https://doi.org/10.1186/s13023-020-01579-2.
Feghali J, Yang W, Xu R, et al. R2eD AVM Score. Stroke. 2019;50(7):1703–10. https://doi.org/10.1161/STROKEAHA.119.025054.
Jiao Y, Zhang J-Z, Zhao Q, et al. Machine Learning-Enabled Determination of Diffuseness of Brain Arteriovenous Malformations from Magnetic Resonance Angiography. Transl Stroke Res. 2021. https://doi.org/10.1007/s12975-021-00933-1.
Zhao S, Zhao Q, Jiao Y, et al. Radiomics Analysis for Predicting Epilepsy in Patients With Unruptured Brain Arteriovenous Malformations. Front Neurol. 2021;12:767165. https://doi.org/10.3389/fneur.2021.767165.
Ding D, Chen C-J, Starke RM, et al. Risk of Brain Arteriovenous Malformation Hemorrhage Before and After Stereotactic Radiosurgery: A Multicenter Study. Stroke. 2019;50:1384–91. https://doi.org/10.1161/STROKEAHA.118.024230.
Rutledge WC, Ko NU, Lawton MT, Kim H. Hemorrhage Rates and Risk Factors in the Natural History Course of Brain Arteriovenous Malformations. Transl Stroke Res. 2014;5:538–42. https://doi.org/10.1007/s12975-014-0351-0.
Stefani MA, Sgarabotto Ribeiro D, Mohr JP. Grades of brain arteriovenous malformations and risk of hemorrhage and death. Ann Clin Transl Neurol. 2019;6:508–14. https://doi.org/10.1002/acn3.723.
van Griethuysen JJM, Fedorov A, Parmar C, et al. Computational Radiomics System to Decode the Radiographic Phenotype. Cancer Res. 2017;77:e104–7. https://doi.org/10.1158/0008-5472.CAN-17-0339.
Karim AM, Kaya H, Güzel MS, et al. A Novel Framework Using Deep Auto-Encoders Based Linear Model for Data Classification. Sensors. 2020;20:6378. https://doi.org/10.3390/s20216378.
Shen D, Wu G, Suk HI. Deep Learning in Medical Image Analysis. Annu Rev Biomed Eng. 2017;19:221–48. https://doi.org/10.1146/annurev-bioeng-071516-044442.
Walsh ES, Kreakie BJ, Cantwell MG, Nacci D. A Random Forest approach to predict the spatial distribution of sediment pollution in an estuarine system. PloS One. 2017;12:e0179473. https://doi.org/10.1371/journal.pone.0179473.
Yang L, Wu H, Jin X, et al. Study of cardiovascular disease prediction model based on random forest in eastern China. Sci Rep. 2020;10:5245. https://doi.org/10.1038/s41598-020-62133-5.
Li K, Yao S, Zhang Z, et al. Efficient gradient boosting for prognostic biomarker discovery. Bioinformatics. 2022:btab869. https://doi.org/10.1093/bioinformatics/btab869.
Wongyikul P, Thongyot N, Tantrakoolcharoen P, et al. High alert drugs screening using gradient boosting classifier. Sci Rep. 2021;11:20132. https://doi.org/10.1038/s41598-021-99505-4.
Abraham A, Pedregosa F, Eickenberg M, et al. Machine learning for neuroimaging with scikit-learn. Front Neuroinform. 2014;8:14. https://doi.org/10.3389/fninf.2014.00014.
Huang Y, Liang C, He L, et al. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. JCO. 2016;34:2157–64. https://doi.org/10.1200/JCO.2015.65.9128.
Tomaszewski MR, Gillies RJ. The Biological Meaning of Radiomic Features. Radiology. 2021;298:505–16. https://doi.org/10.1148/radiol.2021202553.
Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48:441–6. https://doi.org/10.1016/j.ejca.2011.11.036.
Bera K, Braman N, Gupta A, et al. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat Rev Clin Oncol. 2022;19:132–46. https://doi.org/10.1038/s41571-021-00560-7.
Elshafeey N, Kotrotsou A, Hassan A, et al. Multicenter study demonstrates radiomic features derived from magnetic resonance perfusion images identify pseudoprogression in glioblastoma. Nat Commun. 2019;10:3170. https://doi.org/10.1038/s41467-019-11007-0.
Giger ML. Machine Learning in Medical Imaging. J Am Coll Radiol. 2018;15:512–20. https://doi.org/10.1016/j.jacr.2017.12.028.
Larvie M. Machine Learning in Radiology: Resistance Is Futile. Radiology. 2019;290:465–6. https://doi.org/10.1148/radiol.2018182312.
Jamieson AR, Giger ML, Drukker K, Pesce LL. Enhancement of breast CADx with unlabeled data. Med Phys. 2010;37:4155–72. https://doi.org/10.1118/1.3455704.
Jamieson AR, Giger ML, Drukker K, et al. Exploring nonlinear feature space dimension reduction and data representation in breast Cadx with Laplacian eigenmaps and t-SNE. Med Phys. 2010;37:339–51. https://doi.org/10.1118/1.3267037.
Kniep HC, Madesta F, Schneider T, et al. Radiomics of Brain MRI: Utility in Prediction of Metastatic Tumor Type. Radiology. 2019;290:479–87. https://doi.org/10.1148/radiol.2018180946.
Mohan G, Subashini MM. MRI based medical image analysis: Survey on brain tumor grade classification. Biomed Signal Process Control. 2018;39:139–61. https://doi.org/10.1016/j.bspc.2017.07.007.
Ibrahim A, Primakov S, Beuque M, et al. Radiomics for precision medicine: Current challenges, future prospects, and the proposal of a new framework. Methods. 2021;188:20–9. https://doi.org/10.1016/j.ymeth.2020.05.022.
Chen C-J, Ding D, Derdeyn CP, et al. Brain arteriovenous malformations: A review of natural history, pathobiology, and interventions. Neurology. 2020;95:917–27. https://doi.org/10.1212/WNL.0000000000010968.
Westerlaan HE, van Dijk JMC, van Dijk MJ, et al. Intracranial aneurysms in patients with subarachnoid hemorrhage: CT angiography as a primary examination tool for diagnosis--systematic review and meta-analysis. Radiology. 2011;258:134–45. https://doi.org/10.1148/radiol.10092373.
Yang J, Xie M, Hu C, et al. Deep Learning for Detecting Cerebral Aneurysms with CT Angiography. Radiology. 2021;298:155–63. https://doi.org/10.1148/radiol.2020192154.
Funding
This study was funded by the National Key Research and Disease Program (CN): Early Identification and Screening of Panvascular Diseases (2021YFC2500502)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, S., Wang, J., Sun, S. et al. CT Angiography Radiomics Combining Traditional Risk Factors to Predict Brain Arteriovenous Malformation Rupture: a Machine Learning, Multicenter Study. Transl. Stroke Res. (2023). https://doi.org/10.1007/s12975-023-01166-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12975-023-01166-0