Abstract
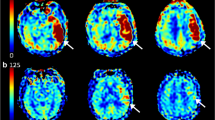
The relevance of impaired microvascular tissue reperfusion despite successful macrovascular angiographic reperfusion (no-reflow) in acute ischemic stroke (AIS) remains controversial. In this study, we aimed to investigate the impact of tissue optimal reperfusion (TOR) and its influencing factors. From December 1, 2020 to December 1, 2021, AIS patients with successful recanalization (modified Thrombolysis in Cerebral Infarction score [mTICI] ≥ 2b) after mechanical thrombectomy (MT) were retrospectively reviewed. Computed tomography perfusion was performed before and after MT. Successful reperfusion was assessed by TOR, defined as > 90% reduction of the Tmax > 6 s lesion volumes between baseline and early follow-up perfusion profiles. The impact of TOR on functional outcomes after successful recanalization and influencing factors for TOR were both investigated. Sixty-three patients were included, including 44 cases in the TOR group and 19 cases in the non-TOR group. The TOR group had a higher rate of favorable outcome (aOR 4.366, 95%CI 1.159–16.445, p = 0.030) and NIHSS improvement (aOR 5.089, 95%CI 1.340–19.322, p = 0.017) than the non-TOR group. Multivariable logistic regression showed baseline glucose (OR 0.648, 95%CI 0.492–0.854, p = 0.002) and mTICI 2c/3 (OR 10.984, 95%CI 2.220–54.343, p = 0.003) predicted TOR in model 1; in model 2, postoperative glucose (OR 0.468, 95%CI 0.278–0.787, p = 0.004) and mTICI 2c/3 (OR 9.436, 95%CI 1.889–47.144, p = 0.006) were predictive. TOR was strongly associated with good functional outcomes after successful recanalization of MT. Higher mTICI grade and lower perioperative glucose level may predict microvascular tissue reperfusion.


Similar content being viewed by others
Data Availability
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding authors.
Change history
21 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12975-022-01098-1
References
Ding Q, Liu S, Yao Y, et al. Global, Regional, and National Burden of Ischemic Stroke, 1990–2019. Neurology. 2021. https://doi.org/10.1212/WNL.0000000000013115[publishedOnlineFirst:2021/12/17].
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–418. https://doi.org/10.1161/STR.0000000000000211[publishedOnlineFirst:2019/10/31].
Desai SM, Tonetti DA, Morrison AA, et al. Relationship between reperfusion and intracranial hemorrhage after thrombectomy. J Neurointerv Surg. 2020;12(5):448–53. https://doi.org/10.1136/neurintsurg-2019-015337[publishedOnlineFirst:2019/10/28].
Ng FC, Churilov L, Yassi N, et al. Prevalence and significance of impaired microvascular tissue reperfusion despite macrovascular angiographic reperfusion (No-Reflow). Neurology. 2022;98(8):e790–801. https://doi.org/10.1212/WNL.0000000000013210[publishedOnlineFirst:2021/12/16].
Dargazanli C, Fahed R, Blanc R, et al. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights From the ASTER trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization). Stroke. 2018;49(5):1189–96. https://doi.org/10.1161/STROKEAHA.118.020700[publishedOnlineFirst:2018/04/08].
Ter Schiphorst A, Charron S, Hassen WB, et al. Tissue no-reflow despite full recanalization following thrombectomy for anterior circulation stroke with proximal occlusion: a clinical study. J Cereb Blood Flow Metab. 2021;41(2):253–66. https://doi.org/10.1177/0271678X20954929[publishedOnlineFirst:2020/09/23].
Tan Z, Parsons M, Bivard A, et al. Optimal tissue reperfusion estimation by computed tomography perfusion post-thrombectomy in acute ischemic stroke. Stroke. 2021;52(12):e760–3. https://doi.org/10.1161/STROKEAHA.121.034581 [published Online First: 2021/10/22].
Carbone F, Busto G, Padroni M, et al. Radiologic cerebral reperfusion at 24 h predicts good clinical outcome. Transl Stroke Res. 2019;10(2):178–88.https://doi.org/10.1007/s12975-018-0637-8[publishedOnlineFirst:2018/06/28].
Regenhardt RW, Etherton MR, Das AS, et al. Infarct growth despite endovascular thrombectomy recanalization in large vessel occlusive stroke. J Neuroimaging. 2021;31(1):155–64.https://doi.org/10.1111/jon.12796[publishedOnlineFirst:2020/10/30].
Renú A, Millán M, San Román L, et al. Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke. JAMA. 2022. https://doi.org/10.1001/jama.2022.1645.
Li X, Li C, Shi M, et al. Which glucose parameter best predicts poor outcome after mechanical thrombectomy for acute large vessel occlusion stroke? Intern Med J. 2021. https://doi.org/10.1111/imj.15259[publishedOnlineFirst:2021/03/06].
Semerano A, Laredo C, Zhao Y, et al. Leukocytes, collateral circulation, and reperfusion in ischemic stroke patients treated with mechanical thrombectomy. Stroke. 2019;50(12):3456–64. https://doi.org/10.1161/strokeaha.119.026743[publishedOnlineFirst:2019/10/18].
Cannarsa GJ, Wessell AP, Chryssikos T, et al. Initial stress hyperglycemia is associated with malignant cerebral edema, hemorrhage, and poor functional outcome after mechanical thrombectomy. Neurosurgery. 2022;90(1):66–71. https://doi.org/10.1227/NEU.0000000000001735[publishedOnlineFirst:2022/01/05].
Dalkara T. Pericytes: a novel target to improve success of recanalization therapies. Stroke. 2019;50(10):2985–91. https://doi.org/10.1161/STROKEAHA.118.023590[publishedOnlineFirst:2019/09/10].
Kaesmacher J, Meinel TR, Kurmann C, et al. Safety and efficacy of intra-arterial fibrinolytics as adjunct to mechanical thrombectomy: a systematic review and meta-analysis of observational data. J Neurointerv Surg. 2021. https://doi.org/10.1136/neurintsurg-2020-016680[publishedOnlineFirst:2021/01/31].
Ben Hassen W, Malley C, Boulouis G, et al. Inter- and intraobserver reliability for angiographic leptomeningeal collateral flow assessment by the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) scale. J Neurointerv Surg. 2019;11(4):338–41. https://doi.org/10.1136/neurintsurg-2018-014185[publishedOnlineFirst:2018/08/23].
Albers GW, Lansberg MG, Brown S, et al. Assessment of optimal patient selection for endovascular thrombectomy beyond 6 hours after symptom onset: a pooled analysis of the AURORA database. JAMA Neurol. 2021. https://doi.org/10.1001/jamaneurol.2021.2319[publishedOnlineFirst:2021/07/27].
Faizy TD, Kabiri R, Christensen S, et al. Perfusion imaging-based tissue-level collaterals predict ischemic lesion net water uptake in patients with acute ischemic stroke and large vessel occlusion. J Cereb Blood Flow Metab. 2021;41(8):2067–75. https://doi.org/10.1177/0271678x21992200 [published Online First: 2021/02/10]
Krishnan R, Mays W, Elijovich L. Complications of mechanical thrombectomy in acute ischemic stroke. Neurology. 2021;97(20 Suppl 2):S115–25. https://doi.org/10.1212/WNL.0000000000012803[publishedOnlineFirst:2021/11/18].
Mistry EA, Yeatts S, de Havenon A, et al. Predicting 90-day outcome after thrombectomy: baseline-adjusted 24-hour NIHSS is more powerful than NIHSS score change. Stroke. 2021;52(8):2547–53. https://doi.org/10.1161/STROKEAHA.120.032487[publishedOnlineFirst:2021/05/19].
Inoue M, Mlynash M, Straka M, et al. Clinical outcomes strongly associated with the degree of reperfusion achieved in target mismatch patients: pooled data from the Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution studies. Stroke. 2013;44(7):1885–90. https://doi.org/10.1161/STROKEAHA.111.000371[publishedOnlineFirst:2013/05/25].
Elgendy IY, Ya’Qoub L, Chen KH, et al. Coronary microvascular dysfunction in patients with non-obstructive coronary arteries: current gaps and future directions. Drugs. 2022;82(3):241–50. https://doi.org/10.1007/s40265-021-01667-y[publishedOnlineFirst:20220129].
Sucato V, Novo G, Saladino A, et al. Coronary microvascular dysfunction. Minerva Cardioangiol. 2020;68(2):153–63. https://doi.org/10.23736/s0026-4725.20.05070-7[published Online First: 20200220].
Chen VHE, Lee GKH, Tan CH, et al. Intra-arterial adjunctive medications for acute ischemic stroke during mechanical thrombectomy: a meta-analysis. Stroke. 2021; 52(4):1192–202. https://doi.org/10.1161/STROKEAHA.120.031738 [published Online First: 2021/02/23]
Anderson RE, Tan WK, Martin HS, et al. Effects of glucose and PaO2 modulation on cortical intracellular acidosis, NADH redox state, and infarction in the ischemic penumbra. Stroke. 1999;30(1):160–70. https://doi.org/10.1161/01.str.30.1.160[publishedOnlineFirst:1999/01/08].
Kawai N, Keep RF, Betz AL. Hyperglycemia and the vascular effects of cerebral ischemia. Acta Neurochir Suppl. 1997;70:27–9. https://doi.org/10.1007/978-3-7091-6837-0_8[publishedOnlineFirst:1997/01/01].
Dietrich WD, Alonso O, Busto R. Moderate hyperglycemia worsens acute blood-brain barrier injury after forebrain ischemia in rats. Stroke. 1993;24(1):111–6. https://doi.org/10.1161/01.str.24.1.111[publishedOnlineFirst:1993/01/01].
Aly M, Abdalla RN, Batra A, et al. Follow-up neutrophil-lymphocyte ratio after stroke thrombectomy is an independent biomarker of clinical outcome. J Neurointerv Surg. 2020. https://doi.org/10.1136/neurintsurg-2020-016342[publishedOnlineFirst:2020/08/09].
Brooks SD, Spears C, Cummings C, et al. Admission neutrophil-lymphocyte ratio predicts 90 day outcome after endovascular stroke therapy. J Neurointerv Surg. 2014;6(8):578–83. https://doi.org/10.1136/neurintsurg-2013-010780[publishedOnlineFirst:2013/10/15].
Altintas O, Altintas MO, Tasal A, et al. The relationship of platelet-to-lymphocyte ratio with clinical outcome and final infarct core in acute ischemic stroke patients who have undergone endovascular therapy. Neurol Res. 2016;38(9):759–65. https://doi.org/10.1080/01616412.2016.1215030[publishedOnlineFirst:2016/08/02].
Takase H, Regenhardt RW. Motor tract reorganization after acute central nervous system injury: a translational perspective. Neural Regen Res. 2021;16(6):1144–9. https://doi.org/10.4103/1673-5374.300330[publishedOnlineFirst:2020/12/04].
Author information
Authors and Affiliations
Contributions
XB, FY, JL, and LJ developed the initial idea for this study. XB, FY, JL, and LJ designed the study. XB, FY, WL, AS, WC, ZF, YF, and RY collected the data. QT analyzed the data. BY, YC, PG, YW, JC, JL, and LJ were consulted about clinical issues. XB and FY contributed to the original draft. XB, FY, AA, RR, QM, JL, and LJ were responsible for the revision of the draft. XB and FY contributed equally and are co-first authors. All authors approved the final version of the manuscript before submission.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
It was waived due to the retrospective nature of this study.
Human and Animal Ethics
Not applicable.
Consent for Publication
All authors have read and approved the submitted manuscript.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bai, X., Yu, F., Tian, Q. et al. Clinical Significance and Influencing Factors of Microvascular Tissue Reperfusion After Macrovascular Recanalization. Transl. Stroke Res. 14, 446–454 (2023). https://doi.org/10.1007/s12975-022-01053-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-022-01053-0