Abstract
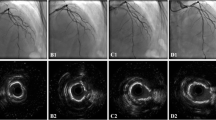
Cutting balloons are commonly used to treat patients with coronary artery disease (CAD) presenting with calcified lesions, but the efficacy of cutting balloons has not been elucidated. We aimed to investigate the impact of novel cutting balloons (Wolverine™) relative to conventional balloons on post-interventional stent expansion for coronary calcified lesions. This study was a single-center, retrospective, observational study. We analyzed 636 lesions from 543 patients with moderate-to-severely calcified CAD lesions undergoing intravascular ultrasound (IVUS)-guided percutaneous coronary intervention using cutting balloons or conventional balloons prior to drug-eluting stent implantation. The primary outcome was post-interventional minimum stent area (MSA) evaluated by IVUS. Propensity score matching was performed to adjust for baseline characteristics. The interaction effects between balloon type and baseline characteristics were also assessed in MSA > 5.5 mm2. Data on pairs of lesions (n = 168) were extracted with no major intergroup differences in baseline characteristics. Post-interventional MSA was not significantly different in the two groups (5.3 ± 2.0 mm2 versus 5.1 ± 1.9 mm2, P = 0.42). Subgroup analysis indicated the subgroup (calcium arc > 180°) showed the qualitative interaction of balloon type effect (P for interaction = 0.056) and the use of cutting balloons was more favorable for lesions with calcium arc ≤ 180° (adjusted odds ratio 4.10, 95% confidence interval 1.14–14.69). The use of cutting balloons did not demonstrate the beneficial effect on post-interventional MSA relative to conventional balloons for patients with CAD presenting moderate-to-severely calcified lesion. However, the use of cutting balloons was more favorable for lesions with calcium arc ≤ 180° to obtain the optimal MSA.



Similar content being viewed by others
References
Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349:1315–23.
Choi SY, Witzenbichler B, Maehara A, Lansky AJ, Guagliumi G, Brodie B, et al. Intravascular ultrasound findings of early stent thrombosis after primary percutaneous intervention in acute myocardial infarction: a Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONSAMI) substudy. Circ Cardiovasc Interv. 2011;4:239–47.
Prati F, Kodama T, Romagnoli E, Gatto L, Di Vito L, Ramazzotti V, et al. Suboptimal stent deployment is associated with subacute stent thrombosis: optical coherence tomography insights from a multicenter matched study. From the CLI Foundation investigators: the CLI-THRO study. Am Heart J. 2015;169:249–56.
Song HG, Kang SJ, Ahn JM, Kim WJ, Lee JY, Park DW, et al. Intravascular ultrasound assessment of optimal stent area to prevent in-stent restenosis after zotarolimus-, everolimus-, and sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2014;83:873–8.
Song L, Mintz GS, Yin D, Yamamoto MH, Chin CY, Matsumura M, et al. Characteristics of early versus late in-stent restenosis in second-generation drug-eluting stents: an optical coherence tomography study. EuroIntervention. 2017;13:294–302.
Vavuranakis M, Toutouzas K, Stefanadis C, Chrisohou C, Markou D, Toutouzas P. Stent deployment in calcified lesions: can we overcome calcific restraint with high-pressure balloon inflations? Catheter Cardiovasc Interv. 2001;52:164–72.
Fujino A, Mintz GS, Matsumura M, Lee T, Kim SY, Hoshino M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018;13:e2182–9.
Okura H, Hayase M, Shimodozono S, Kobayashi T, Sano K, Matsushita T, et al. Mechanisms of acute lumen gain following cutting balloon angioplasty in calcified and noncalcified lesions: an intravascular ultrasound study. Catheter Cardiovasc Interv. 2002;57:429–36.
Song X, Adachi T, Kawase Y, Kimura T, Saito N. Efficacy of the Wolverine cutting balloon on a circumferential calcified coronary lesion: Bench test using a three-dimensional printer and computer simulation with the finite element method. Cardiovasc Interv Ther. 2021. https://doi.org/10.1007/s12928-020-00739-2.
Ryan TJ, Faxon DP, Gunnar RM, Kennedy JW, King SB 3rd, Loop FD, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation. 1988;78:486–502.
Suzuki N, Asano T, Nakazawa G, Aoki J, Tanabe K, Hibi K, et al. Clinical expert consensus document on quantitative coronary angiography from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther. 2020;35:105–16.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS): a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37:1478–92.
Kotani J, Mintz GS, Castagna MT, Pinnow E, Berzingi CO, Bui AB, et al. Intravascular ultrasound analysis of infarct-related and non-infarct-related arteries in patients who presented with an acute myocardial infarction. Circulation. 2003;107:2889–93.
Sonoda S, Morino Y, Ako J, Terashima M, Hassan AH, Bonneau HN, et al. Impact of final stent dimensions on long-term results following sirolimus-eluting stent implantation: serial intravascular ultrasound analysis from the SIRIUS trial. J Am Coll Cardiol. 2004;43:1959–63.
Saito Y, Kobayashi Y, Fujii K, Sonoda S, Tsujita K, Hibi K, et al. Clinical expert consensus document on standards for measurements and assessment of intravascular ultrasound from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther. 2020;35:1–12.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–51.
Räber L, Mintz GS, Koskinas KC, Johnson TW, Holm NR, Onuma Y, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018;39:3281–300.
Ozaki Y, Yamaguchi T, Suzuki T, Nakamura M, Kitayama M, Nishikawa H, et al. Impact of cutting balloon angioplasty (CBA) prior to bare metal stenting on restenosis. Circ J. 2007;71:1–8.
Tang Z, Bai J, Su SP, Wang Y, Liu MH, Bai QC, et al. Cutting-balloon angioplasty before drug-eluting stent implantation for the treatment of severely calcified coronary lesions. J Geriatr Cardiol. 2014;11:44–9.
Amemiya K, Yamamoto MH, Maehara A, Oyama Y, Igawa W, Ono M, et al. Effect of cutting balloon after rotational atherectomy in severely calcified coronary artery lesions as assessed by optical coherence tomography. Catheter Cardiovasc Interv. 2019;94:936–44.
Maejima N, Hibi K, Saka K, Akiyama E, Konishi M, Endo M, et al. Relationship between thickness of calcium on optical coherence tomography and crack formation after balloon dilatation in calcified plaque requiring rotational atherectomy. Circ J. 2016;80:1413–9.
Fujino A, Mintz GS, Lee T, Hoshino M, Usui E, Kanaji Y, et al. Predictors of calcium fracture derived from balloon angioplasty and its effect on stent expansion assessed by optical coherence tomography. JACC Cardiovasc Interv. 2018;11:1015–7.
Acknowledgements
We wish to thank Mr. Takashi Sumikawa, Mr. Hiroki Oyama, Mr. Kazutoshi Ito, Mr. Yusuke Katagiri, Mr. Kohei Nanri and Ms. Haruna Miyaguchi for their expertise in performing the IVUS examinations and Mrs. Saori Sinohara for her expertise in the collection of data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsujimura, T., Ishihara, T., Takahashi, K. et al. Cutting balloons versus conventional balloons for treating patients with coronary artery disease presenting with moderate-to-severely calcified lesions: impact on post-interventional minimum stent area. Cardiovasc Interv and Ther 37, 700–709 (2022). https://doi.org/10.1007/s12928-022-00860-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-022-00860-4