Abstract
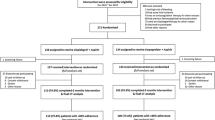
Optimal medical therapy following endovascular therapy (EVT) for femoropopliteal (FP) lesions remains unclear. Therefore, we investigated whether sarpogrelate improves primary patency after EVT for FP lesions. This study was performed as a multicenter, randomized, open-label clinical trial. 186 patients (mean age 75 ± 9 years, 78 % men) with Rutherford class 2–5 due to an FP lesion were randomly assigned to receive or not receive sarpogrelate in addition to aspirin. Primary endpoint was 1-year primary patency and the secondary endpoints were target lesion revascularization (TLR) and secondary patency. Primary patency was defined as a treated vessel without restenosis or repeat revascularization. Restenosis was defined as >2.5 of peak systolic velocity ratio. Patient, lesion, and procedural characteristics did not differ significantly between two groups (mean lesion length 156 ± 94 mm, total occlusion 35 %). Stenting was performed in 133 patients (76 %). Eighty-four (94 %) could ingest sarpogrelate during follow-up period. Primary patency was 66 % in sarpogrelate group and 56 % in non-sarpogrelate group, showing no significant difference between the groups (p = 0.33). The incidence of TLR did not differ in both groups (sarpogrelate 24 % vs non-sarpogrelate 32 %, p = 0.12). Secondary patency also did not differ (sarpogrelate 90 % vs non-sarpogrelate 92 %, p = 0.43). When the interaction of sarpogrelate with the primary patency was analyzed in previously established subgroups, no interactions were noted for any subset. Sarpogrelate did not improve primary patency after EVT for FP disease in this study.





Similar content being viewed by others
References
Laird JR, Katzen BT, Scheinert D, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv. 2010;3:267–76.
Sabeti S, Schillinger M, Amighi J, et al. Primary patency of femoropopliteal arteries treated with nitinol versus stainless steel self-expanding stents: propensity score-adjusted analysis. Radiology. 2004;232:516–21.
Dick P, Wallner H, Sabeti S, et al. Balloon angioplasty versus stenting with nitinol stents in intermediate length superficial femoral artery lesions. Catheter Cardiovasc Interv. 2009;74:1090–5.
Schillinger M, Sabeti S, Loewe C, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354:1879–88.
Norgren L, Hiatt WR, Dormandy JA, et al. Intersociety consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33(Suppl 1):S1–75.
Soga Y, Yokoi H, Kawasaki T, et al. Efficacy of cilostazol after endovascular therapy for femoropopliteal artery disease in patients with intermittent claudication. J Am Coll Cardiol. 2009;53:48–53.
Iida O, Yokoi H, Soga Y, et al. Cilostazol reduces angiographic restenosis after endovascular therapy for femoropopliteal lesions in the Sufficient Treatment of Peripheral Intervention by Cilostazol study. Circulation. 2013;127:2307–15.
Fujita M, Mizuno K, Ho M, et al. Sarpogrelate treatment reduces restenosis after coronary stenting. Am Heart J. 2003;145:E16.
Tamura A, Watanabe T, Shinozaki K, et al. Comparison of sarpogrelate and ticlopidine in bare metal coronary stent implantation. Int J Cardiol. 2008;126:79–83.
Sharma SK, Del Rizzo DF, Zahradka P, et al. Sarpogrelate inhibits serotonin-induced proliferation of porcine coronary artery smooth muscle cells: implications for long-term graft patency. Ann Thorac Surg. 2001;71:1856–64.
Kodama A, Komori K, Hattori K, et al. Sarpogrelate hydrochloride reduced intimal hyperplasia in experimental rabbit vein graft. J Vasc Surg. 2009;49:1272–81.
Saini HK, Takeda N, Goyal RK, et al. Therapeutic potentials of sarpogrelate in cardiovascular disease. Cardiovasc Drug Rev. 2004;22:27–54.
Matsuo H, Shigematsu H. Effects of the 5-HT2A antagonist sarpogrelate on walking ability in patients with intermittent claudication as measured using the walking impairment questionnaire. Ann Vasc Dis. 2008;1:102–10.
Nagayama D, Ohira M, Saiki A, et al. Sarpogrelate hydrochloride decreases cardio-ankle vascular index accompanied by increased serum lipoprotein lipase mass in type 2 diabetic patients. Int Heart J. 2014;55:337–41.
Chen YX, Wang WD, Song XJ, et al. Prospective randomized study of sarpogrelate versus clopidogrel-based dual antiplatelet therapies in patients undergoing femoropopliteal arterial endovascular interventions: preliminary results. Chin Med J. 2015;128:1563–6.
Acknowledgments
We acknowledge the expertise of Dr. Fumitoshi Toyoda (Chidoribashi Hospital), Dr. Yuki Imoto (Fukuoka Wajiro Hospital), Dr. Tatsuya Nakama (Miyazaki Medical Association Hospital), Dr. Masasto Taniguchi (Fukuyama), Dr. Toshinobu Ishikwa (Oita Oka Hospital), Dr. Hideki Doi (Kumamoto Rosai Hospital), Dr. Yuki Uehara (Urasoe General Hospital), Dr. Kenji Iwamoto (Iwakuni Medical center), and the medical staff and clinical research coordinators in all the participating centers.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding source
Association for Establishment of Evidence in Interventions, 2-5-3 New-Hamamatsu building, Hamamatsucho, Minato-ku, Tokyo 105-0013, Japan.
Rights and permissions
About this article
Cite this article
Soga, Y., Shintani, Y., Hamasaki, T. et al. Effectiveness of sarpogrelate after endovascular treatment for femoropopliteal artery disease: ESPALIER study. Cardiovasc Interv and Ther 32, 325–332 (2017). https://doi.org/10.1007/s12928-016-0414-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-016-0414-0