Abstract
Background
Cervical cancer is emerging as a potential target of increased susceptibility to coronavirus disease-2019 (COVID-19), leading to compromised survival rates. Despite this critical link, efficacious anti-cervical cancer/COVID-19 interventions remain limited. Quercetin, known for its efficacy against both cancer and viral infections, holds promise as a therapeutic agent. This study aims to elucidate quercetin’s anti-cervical cancer/COVID-19 mechanisms and potential targets.
Methods
We initiated our investigation with differential gene expression analysis using cervical cancer transcriptome data from The Cancer Genome Atlas (TCGA) and The Genotype-Tissue Expression (GTEx), focusing on intersections with COVID-19-related genes. Network pharmacology was employed to identify the shared targets between cervical cancer/COVID-19 DEGs and quercetin’s targets. Subsequently, Cox proportional hazards analyses were employed to establish a risk score based on these genes. Molecular docking techniques were applied to predict quercetin’s therapeutic targets and mechanisms for mitigating cervical cancer and COVID-19.
Results
Our findings unveiled 45 potential quercetin targets with anti-cervical cancer/COVID-19 actions. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses highlighted significant enrichment in immune pathways and COVID-19-related pathways. A refined risk score model, comprising PLA2G7, TNF, TYK2, F2, and NRP1, effectively stratified cervical cancer patients into distinct risk groups. Importantly, molecular docking analyses illuminated quercetin’s remarkable binding affinity to the primary protease of the coronavirus.
Conclusions
In summation, our study suggests that quercetin holds promise as a potential therapeutic agent for mitigating coronavirus function, specifically through its interaction with the primary protease. This research offers novel insights into exploring COVID-19 susceptibility and enhancing survival in cervical cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since its emergence in 2019, coronavirus disease-2019 (COVID-19) caused by SARS-CoV-2 has wreaked havoc globally, inflicting profound tolls on public health, economies, and societies [1]. SARS-CoV-2 exhibits various mutants such as Alpha, Beta, Gamma, Kappa, Delta and Omicron [2, 3]. Clinical trials are underway to identify effective treatments for COVID-19. Notably, a randomized controlled trial incorporating lopinavir and ritonavir in severe COVID-19 cases yielded no substantial clinical symptom improvement or reduced mortality compared to standard supportive care [4]. Among the gravest concerns is the heightened susceptibility of cancer patients to COVID-19, resulting in exacerbated symptoms and elevated mortality risk [5]. This predicament is particularly worrisome for cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC) patients, who constitute a significant cohort of cancer cases [6]. Cervical cancer, the fourth most prevalent cancer among women, claims the lives of over 300,000 women annually [7]. According to the statistic, nearly 11 women were dying from cervical cancer every day [8]. The majority of cervical cancer cases are associated with human papillomavirus (HPV) infection. HPV-negative cervical cancer had a worse survival [9]. As a highly vulnerable group, cancer patients are at increased risk for SARS-CoV-2 virus infections due to longer hospital stays and weaknesses in their immune systems [10,11,12]. COVID-19 infection causes treatment delays and interruption for cervical cancer patients. Given the vulnerability of cancer patients, particularly in the context of the ongoing pandemic, identifying effective therapeutic strategies for cervical cancer patients infected with COVID-19 is imperative.
Quercetin, a polyphenolic flavonoid prominently employed in traditional Chinese medicine, exhibits promising chemo-preventive properties [13, 14]. Its role in modulating signal transduction pathways and augmenting antioxidant defenses has garnered interest in disease prevention [15]. Additionally, quercetin has emerged as an adjuvant in anti-cancer regimens, enhancing treatment sensitivity and minimizing collateral damage to healthy cells [16, 17]. Furthermore, in conjunction with vitamin C, quercetin has demonstrated synergistic potential in augmenting antiviral therapies for COVID-19 [18]. Despite these insights, comprehensive investigations into quercetin’s targets and mechanisms for treating cervical cancer patients with COVID-19 are limited.
In the realm of medicinal research, web-based pharmacology approaches have emerged as robust tools for comprehending the action mechanisms of Chinese medicines [19, 20]. Leveraging network pharmacology, which characterizes drug actions and mechanisms at the molecular level, we aimed to elucidate quercetin’s potential as an adjunctive therapy for cervical cancer patients with COVID-19. The ensuing study delineates our network pharmacology-based analysis, as depicted in Fig. 1.
2 Materials and methods
2.1 Screening for core genes associated with COVID-19 and potential differentially expressed genes of CESC
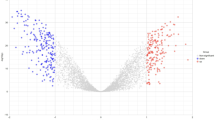
The National Center for Biotechnology Information (NCBI) and the GeneCards Database were employed to identify genes associated with COVID-19 [21]. Transcriptomic profiles of CESC and normal cervical samples were retrieved from The Cancer Genome Atlas (TCGA) on November 05, 2021 Supplementary transcriptomic profiles from the Genotype-Tissue Expression (GTEx) database was included for normal cervical samples [22]. Differential gene expression analysis for CESC was performed using the ‘DEseq2’ package in the R environment, considering genes with false discovery rate (FDR) < 0.05 and |log fold change (FC)| > 1 as differentially expressed. Visualization was facilitated using the ‘EnhancedVolcano’ and ‘ComplexHeatmap’ packages [23, 24]. Overlapping genes between COVID-19-related genes and CESC DEGs were identified.
2.2 Identification of quercetin-related genes and enrichment analysis
Potential quercetin targets were sourced from Comparative Toxicogenomics Database (CTD) [25], DrugBank [26], Swiss Target Prediction [27], TargetNet [28], Kyoto Encyclopedia of Genes and Genomes (KEGG) [29] database. Subsequently, gene ontology (GO) and KEGG enrichment analyses were performed using g:Profiler for enrichment and the ‘ggplot2’ and ‘GOplot’ packages for visualization [30, 31].
2.3 Construction of protein–protein interaction networks
The STRINGv11.5 [32] was employed to construct protein–protein interaction (PPI) networks for quercetin-related genes associated with anti-CESC/COVID-19 effects. Visual representation of results was generated using Cytoscape software (version 3.6.1) [33]. Hub genes were identified using the CytoHubba plugin based on the maximal clique centrality algorithm.
2.4 Clinical analysis for CESC/COVID-19-related genes
Clinical information of CESC patients was obtained from TCGA. Univariate Cox analysis was conducted to identify genes associated with overall survival (OS). Subsequently, multivariate Cox regression analysis were performed using the “glmnet” package to establish a risk score formula based on normalized gene expression values. Patients were categorized into high- or low-risk subgroups using the median risk score. Receiver operating characteristic (ROC) curves (including 3-year, 5-year, and 10-year survival) were plotted to evaluate predictive value using the ‘timeROC’ package.
2.5 Gene set enrichment analysis and immune cell infiltration analysis
Differentially expressed genes between high- and low-risk subgroups were identified using the ‘limma’ package Gene set enrichment analysis (GSEA) was conducted utilizing packages such as “org.Hs.eg.db”, “dplyr”, “enrichplot”, and “clusterProfiler”. Immune cell enrichment scores for 22 immune-related cells were calculated using the CIBERSORT algorithm. Immune cell infiltration content between high- and low-risk subgroups was visualized using the ‘ggpubr’ package. Additionally, the TIMER database [34] was utilized to assess the association between prognostic risk model genes and immune cell infiltration in CESC.
2.6 Prediction of immune checkpoint blockade treatment response
To gauge the risk score’s potential in predicting immune checkpoint blockade treatment response, clinical features and expression data from the IMvigor210 cohort were obtained (http://research-pub.gene.com /IMvigor210CoreBiologies) [35]. The risk score was utilized to predict OS and immune checkpoint blockade therapeutic responses [including progress disease (PD), stable disease (SD), partial remission (PR), and complete remission (CR)].
2.7 Molecular docking
Autodock 4.2 software [36] was employed for semi-flexible molecular docking. Crystal structures of COVID-19 main protease (6LU7) and spike glycoprotein (6VYB) were obtained from the Protein Data Bank (PDB) [37]. The grid box was set to contain all receptor region with the original ligand coordinates. The binding energy was got by autogrid4 and autodock4 function. Molecular docking outcomes were observed using PyMol software [38].
3 Result
3.1 Differentiation analysis of CESC
A comprehensive cohort of 306 CESC samples and 3 normal cervical tissue samples from TCGA, along with 19 cervix samples from GTEx, formed the basis for our investigation. Applying stringent criteria, we identified 4986 differentially expressed genes (DEGs) between CESC patients and controls, with 3085 genes exhibiting up-regulation and 1901 genes down-regulation (Fig. 2).
3.2 Identification of quercetin targets for CESC/COVID-19
Incorporating data from NCBI and the Genecard database, we retrieved 492 COVID-19-related genes. A total of 90 CESC/COVID-19-related genes were identified, comprising 62 up-regulated and 28 down-regulated genes in CESC. Further analysis revealed 4237 quercetin-related genes across five databases, including CTD, DrugBank, Swiss Target Prediction, TargetNet and KEGG. Our integration efforts highlighted 45 quercetin targets with implications for CESC/COVID-19, illustrated in Fig. 3A. The resultant PPI network, governed by these 45 intersection genes, was visualized via STRING and Cytoscape (Fig. 3B).
Functional Enrichment Analysis of Quercetin Targets. A Venn diagram depicting the intersection of quercetin, CESC, and COVID-19 genes. B Protein–protein interaction (PPI) network was visualized using Cytoscape, indicating the gene associations. C GO analysis showing the top 10 biological processes (BP), cellular components (CC), and molecular functions (MF) of intersecting genes. D KEGG pathway analysis of quercetin targets for CESC/COVID-19.
3.3 GO enrichment analysis and KEGG pathway analysis
To illuminate the functional underpinnings of quercetin’s action in the context of CESC/COVID-19, we conducted Gene Ontology (GO) and KEGG pathway analyses on the 45 intersect genes. GO analyses revealed that these genes were predominantly involved in biological regulation, response to stimulus, and cellular response to stimulus. Cellular component enrichment centered around cytoplasm, extracellular region, and extracellular space, while molecular function analysis underscored signaling receptor binding, molecular function regulation, and cytokine receptor binding (Fig. 3C). KEGG pathway analysis unveiled significant enrichment in coronavirus disease-COVID-19, necroptosis, cytokine-cytokine receptor interaction, viral protein interaction with cytokine and cytokine receptor, and an array of signaling pathways (Fig. 3D).
3.4 Independent prognostic signatures and risk analysis
Our exploration into overlapping genes’ impact on survival encompassed both univariate and multivariate Cox regression analyses. Eight genes emerged from univariate Cox regression, including TNF (tumor necrosis factor), IFNG (interferon gamma), IL1A (interleukin-1), F2 (coagulation factor II), NRP1 (neuropilin 1), TYK2 (tyrosine kinase 2), IDO1 (indoleamine 2,3-dioxygenase 1), and PLA2G7 (phospholipase A2 group VII) (P < 0.05, Fig. 4A). Subsequent multivariate Cox regression identified five independent prognostic factors-TNF, F2, NRP1, TYK2, and PLA2G7 (P < 0.05, Fig. 4B). The risk score was calculated as follows: risk score = (0.079934737 * TNF exp.) + (0.754296176 * F2 exp.) + (0.077712628 * NRP1 exp.) − (0.052768486 * TYK2 exp.) − (0.130543819 * PLA2G7 exp.). The derived risk score formula enabled the stratification of patients into high- and low-risk groups, with high-risk associated with poorer OS (Fig. 4C). ROC analysis showed robust predictive performance, with AUCs of 0.733, 0.738, and 0.614 at 3, 5, and 10 years, respectively (Fig. 4D). Survival scatter plots demonstrated the superior survival of low-risk patients (Fig. 4E, F). Notably, TNF, NRP1, TYK2, and PLA2G7 exhibited differential expression between high- and low-risk groups. The expression of TNF and NRP1 was lower in low-risk group, while the expression of TYK2 and PLA2G7 was higher in low-risk group (Fig. 5A). Additionally, NRP1 and PLA2G7 displayed heightened expression in grade 3/4 compared to grade 1/2 (Fig. 5A–C).
Construction and validation of prognostic signatures. A Forest plot presenting HR and P-values from univariate Cox regression analysis. B Multivariate Cox analysis revealing independent prognostic signatures. C Kaplan-Meier survival analysis indicated significantly shorter OS in the high-risk group (P < 0.001). D Time-dependent ROC curves assessing prognostic signature accuracy. E Risk score distribution among CESC patients. F Scatterplot depicting the correlation between risk scores and survival time/status
3.5 Functional enrichment analyses
The high-risk group was linked to responses to immobilization stress, lipid catabolic processes, substrate adhesion-dependent cell spreading, vasoconstriction, and hormone activity in the c5.go dataset (Fig. 6A, B). Conversely, the low-risk group exhibited significant enrichment of immune-related biological processes such as adaptive immune response, activation of the immune response, and myeloid leukocyte immunity (Fig. 6C, D). In the c2.cp.kegg dataset, the high-risk group displayed associations with ribosome, PPAR signaling pathway, tyrosine metabolism, nitrogen metabolism, and metabolism of xenobiotics by cytochrome P450 (Fig. 6E, F). On the other hand, the low-risk group was enriched in cytokine receptor interaction, chemokine signaling pathway, cell adhesion molecules, T cell receptor signaling pathway, and natural killer cell-mediated cytotoxicity (Fig. 6G, H).
GO and KEGG Pathway Enrichment Analysis. Enrichment plot illustrating the running sum of enrichment scores (left curve), gene position within pathways (middle part), and metric distribution (bottom part) in high and low-risk groups. The upSet plot displays the metric distribution of core enrichment genes. A, B GO analysis in the high-risk group. C, D GO analysis in a low-risk group. E, F KEGG pathway enrichment in the high-risk group. G, H KEGG pathway enrichment in a low-risk group
3.6 Tumor immune microenvironment and immunotherapeutic response
Application of CIBERSORT unveiled variations in the tumor immune microenvironment between high- and low-risk groups in CESC. The high-risk group exhibited lower immune cell infiltration levels, particularly CD8+ T cells, M1 macrophages, M2 macrophages, regulatory T cells (Tregs), resting mast cells, activated memory CD4+ T cells, and dendritic cells. Conversely, infiltration of M0 macrophages, resting memory CD4+ T cells, active NK cells, and dendritic cells was significantly elevated in the high-risk group (Fig. 7A). Employing the IMvigor210 immunotherapy cohort, we found that low-risk patients enjoyed notable survival benefits from anti-PD-L1 immunotherapy (P = 0.005) (Fig. 7B). The risk model demonstrated fair predictive accuracy for immunotherapy responsiveness with AUC values of 0.644, 0.586, and 0.554 at 1, 3, and 5 years, respectively (Fig. 7C). Further analysis established that low-risk patients were more responsive to immunotherapy (P = 0.0027) (Fig. 7D).
Immune Microenvironment and Therapeutic Response. A Comparison of immune cell infiltration between high-risk and low-risk groups. B Kaplan-Meier survival curves for IMvigor210 cohort based on risk scores. C ROC curves assessing predictive accuracy of the risk score in the IMvigor210 cohort. D Comparison of risk scores in different anti-PD-L1 treatment response groups. ****P < 0.0001, **P < 0.01, *P < 0.05
3.7 Association of genes with tumor immune infiltrates
Exploring the correlation between the expression of TNF, F2, NRP1, TYK2, and PLA2G7 and immune cell infiltrates revealed positive associations between higher expression levels and increased immune cell infiltration in tumors, including B cells, CD8+ T cells, CD4+ T cells, macrophages, neutrophils, and dendritic cells (Fig. 8A–E). Moreover, copy number variations (CNVs) of these genes exhibited notable impacts on immune cell infiltration levels. Specifically, deep deletion, arm-level deletion, arm-level gain, and high amplification of these genes significantly influenced immune cell infiltration in CESC (Fig. 9A–E).
3.8 Docking results
Molecular docking assays revealed robust binding interactions between quercetin and the crystal structures of COVID-19 main protease and spike glycoprotein, with favorable docking energies and hydrogen bond formation (− 5.88 kcal mol−1 for main protease and − 3.42 kcal mol−1 for spike glycoprotein). The quercetin formed hydrogen bonds with residues GLU-166 and THR-190 of the main protease and residue LEU-977 of spike glycoprotein (Table 1). Moreover, the docking analysis indicated favorable binding activities between quercetin and the five independent prognostic signatures with docking energy less than − 5 kcal mol−1 and two or more hydrogen bonds formed (Fig. 10; Table 2).
4 Discussion
Evidence has shown potential therapeutic strategies for colon adenocarcinoma (COAD) and COVID-19 by quercetin. A total of 105 gene were potential targets of quercetin for anti-COAD/COVID-19, which were correlated with apoptosis, immune, oxidative stress. IL-17, HIF-1 and TNF were involved in quercetin-mediated treatment in COAD/COVID-19 patients [39]. Our investigation corroborates previous studies showcasing quercetin’s synergistic anti-CESC effects when combined with cisplatin [40, 41]. Employing network pharmacology, we pinpointed 45 target genes through which quercetin exerts its action against CESC and COVID-19. Enrichment analysis illuminated the therapeutic mechanisms, primarily centered around necroptosis, cytokine-cytokine receptor interaction, and viral protein interaction with cytokine and cytokine receptor pathways. Importantly, we identified that five independent prognostic signatures, including TNF, F2, NRP1, TYK2, and PLA2G7, via multivariate Cox regression could be biomarkers for prognosis.
TNF is a cytokine with potent pro-inflammatory effects [42]. Previous studies have shown that TNF had antitumor activity [43], playing an important role in tumor proliferation, migration, and invasion [44]. In CESC, it could induce apoptosis by activating the mitochondrial caspase-9 death signaling pathway. Moreover, recent study found that serum TNF level in patients with CESC were usually significantly elevated than this in non-CESC patients [45]. After surgical treatment, serum TNF level will gradually return to normal in CESC patients. Consistent with previous researches, TNF was considered as a risk factor for prognosis of CESC in our study. The expression level of TNF was significantly higher in high-risk group and tumor tissue than that in low-risk group and normal tissue.
Besides, current studies have proved that TNF-308 gene GA and AA polymorphisms were associated with the risk of cervical cancer [46, 47]. Moreover, TNF-308 AA and IL-10-592 CA/AA polymorphisms are linked to an increased risk of cervical cancer [48]. F2 was considered as an important determinant of thrombin generation [49]. A number of studies discovered that complement activation following SARS-CoV-2 infections generates thrombin and produces thrombosis [50, 51]. NRP1 is a semaphorin III receptor that is the foundation of neurosynapses [52]. NRP1 has been reported to induce tumor-associated macrophage activation and exert pro-tumor effects in cervical cancer under hypoxia [53]. Previous study have shown that NRP1 was associated with cervical cancer progression and poor survival, suggesting that NRP1 could be an independent prognostic factor in cervical cancer [54]. High expression of NRP1 in cervical cancer patients was correlated with shorter OS [55]. Moreover, preoperative chemoradiation therapy reduced Treg and Nrp1 + Treg levesl in lymph nodes of cervical cancer patients [56]. Soluble NRP1 (sNRP) in circulating and NRP1 proteins were associated with cervical cancer stages. In addition, sNRP exhibited a possible diagnostic biomarker for cervical cancer [57]. Transportin-1 (TNPO1)-induced nuclear import of FUBP1 (Far upstream element binding protein 1) led to tumor immune evasion via upregulation of NRP1 in cervical cancer [58]. And high expression level of NRP1 was associated with poor 5-year survival rates. Similarly, NRP1 was confirmed as an oncogene in this study.
In COVID-19 patients, a significant decrease in TYK2 level was observed in male patients compared to male controls [59]. The down-regulation of TYK2 was proposed as a molecular mechanism causing SARS-CoV-2 to be incapable of inducing a competent interferon response. Castineira et al. [60] demonstrated that there is an association between life-threatening diseases in COVID-19 and high level of TYK2. PLA2G7 is a calcium-independent lipoprotein-binding phospholipase, involved in cell signaling and metabolism [61]. On the one hand, some studies have shown that high level of PLA2G7 was positively correlated with aggressiveness in cancer [62,63,64]. PLA2G7 promoted cell migration and invasion in prostate cancer [63]. Meanwhile, Morigny et al. demonstrated that secretion and expression of PLA2G7 are positively correlated with cancer cachexia [65]. Depletion of PLA2G7 reduced intestinal polyposis and tumorigenesis in APC (Min/+) mice [66]. PLAG7 exhibited protective function in breast cancer via negative regulation of the Wnt signaling pathway [67]. On the other hand, Liao et al. discovered that high PLA2G7 protein level was associated with significantly longer OS than low protein level of PLA2G7 in ovarian cancer patients. The protective character of PLA2G7 was speculated to be mediated by negatively regulating the Wnt/β-catenin pathway [68]. Similarly, our analysis showed that PLA2G7 was associated with a better prognosis in CESC.
Quercetin has been reported to influence SARS-CoV-2 infection and COVID-19-associated cancer progression via suppression of HIF-1a and mTOR [69]. Quercetin influenced several signaling pathways, including TNF, TRAIL and FASL, and induced cell apoptosis in cervical cancer [70]. There are several limitations in this study. For example, a comprehensive cohort of 306 CESC samples and 3 normal cervical tissues from TCGA was used. Only 3 normal cervical tissues were included in this study. In addition, this work lacks cell line experiments and animal studies. It is worthy to note that in vitro experiments and in vivo mouse models are necessary to validate the function of quercetin for the treatment of COVID-19 with CESC.
5 Conclusion
Based on the results above, we believe that adjuvant therapy with quercetin may contribute to the treatment of COVID-19 or COVID-19 with CESC. The findings from this study identified molecules involved in the link between CESC and COVID-19, and five key genes of quercetin for CESC/COVID-19 treatment, including PLA2G7, TNF, TYK2, F2, NRP1. This finding can help the treatment of patients with CESC/COVID-19.
Data availability
The data are available from the corresponding author upon reasonable request.
Database
NCBI: https://www.ncbi.nlm.nih.gov/.
GeneCards Database:https://www.genecards.org/.
TCGA:https://portal.gdc.cancer.gov/.
GTEx:https://www.gtexportal.org/.
CTD: https://ctdbase.org/.
DrugBank: https://go.drugbank.com/.
SwissTargetPrediction: http://swisstargetprediction.ch/.
TargetNet: http://targetnet.scbdd.com/.
Kyoto Encyclopedia of Genes and Genomes: https://www.genome.jp/kegg/.
g:Profiler: https://biit.cs.ut.ee/gprofiler.
STRING: https://cn.string-db.org/.
Protein Data Bank website: https://www.rcsb.org/search.
References
Lotfinejad P, Asadzadeh Z, Najjary S, Somi MH, Hajiasgharzadeh K, Mokhtarzadeh A, et al. COVID-19 infection: concise review based on the immunological perspective. Immunol Invest. 2022;51:246–65.
Chen Q, Zhang J, Wang P, Zhang Z. The mechanisms of immune response and evasion by the main SARS-CoV-2 variants. iScience. 2022;25:105044.
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141–54.
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–99.
Han HJ, Nwagwu C, Anyim O, Ekweremadu C, Kim S. COVID-19 and cancer: from basic mechanisms to vaccine development using nanotechnology. Int Immunopharmacol. 2021;90:107247.
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8:e191–e203.
Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019;393:169–82.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics. CA Cancer J Clin. 2021;71:7–33.
Perkins RB, Wentzensen N, Guido RS, Schiffman M. Cervical cancer screening: a review. JAMA. 2023;330:547–58.
Kamboj M, Sepkowitz KA. Nosocomial infections in patients with cancer. Lancet Oncol. 2009;10:589–97.
Sica A, Massarotti M. Myeloid suppressor cells in cancer and autoimmunity. J Autoimmun. 2017;85:117–25.
Wu Z, McGoogan JM. Characteristics of and important Lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42.
Fraga CG, Croft KD, Kennedy DO, Tomás-Barberán FA. The effects of polyphenols and other bioactives on human health. Food Funct. 2019;10:514–28.
Rauf A, Imran M, Khan IA, Ur-Rehman M, Gilani SA, Mehmood Z, et al. Anticancer potential of quercetin: a comprehensive review. Phytother Res. 2018;32:2109–30.
Xu D, Hu MJ, Wang YQ, Cui YL. Antioxidant activities of quercetin and its complexes for medicinal application. Molecules. 2019;24:1123.
Reyes-Farias M, Carrasco-Pozo C. The anti-cancer effect of quercetin: molecular implications in cancer metabolism. Int J Mol Sci. 2019;20:3177.
Tang SM, Deng XT, Zhou J, Li QP, Ge XX, Miao L. Pharmacological basis and new insights of quercetin action in respect to its anti-cancer effects. Biomed Pharmacother. 2020;121:109604.
Colunga Biancatelli RML, Berrill M, Catravas JD, Marik PE, Quercetin, Vitamin C. An experimental, synergistic therapy for the prevention and treatment of SARS-CoV-2 related disease (COVID-19). Front Immunol. 2020;11:1451.
Song X, Zhang Y, Dai E, Wang L, Du H. Prediction of triptolide targets in rheumatoid arthritis using network pharmacology and molecular docking. Int Immunopharmacol. 2020;80:106179.
Aihaiti Y, Song Cai Y, Tuerhong X, Ni Yang Y, Ma Y, Shi Zheng H, et al. Therapeutic effects of naringin in rheumatoid arthritis: network pharmacology and experimental validation. Front Pharmacol. 2021;12:672054.
Gussow AB, Auslander N, Faure G, Wolf YI, Zhang F, Koonin EV. Genomic determinants of pathogenicity in SARS-CoV-2 and other human coronaviruses. Proc Natl Acad Sci U S A. 2020;117:15193–9.
Carithers LJ, Ardlie K, Barcus M, Branton PA, Britton A, Buia SA, et al. A novel approach to high-quality postmortem tissue procurement: the GTEx project. Biopreserv Biobank. 2015;13:311–9.
Gu Z, Eils R, Schlesner M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32:2847–9.
Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550.
Davis AP, Grondin CJ, Johnson RJ, Sciaky D, Wiegers J, Wiegers TC, et al. Comparative toxicogenomics database (CTD): update 2021. Nucleic Acids Res. 2021;49:D1138–d1143.
Wishart DS, Feunang YD, Guo AC, Lo EJ, Marcu A, Grant JR, et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 2018;46:D1074–d1082.
Gfeller D, Grosdidier A, Wirth M, Daina A, Michielin O, Zoete V. SwissTargetPrediction: a web server for target prediction of bioactive small molecules. Nucleic Acids Res. 2014;42:W32–38.
Yao ZJ, Dong J, Che YJ, Zhu MF, Wen M, Wang NN, et al. TargetNet: a web service for predicting potential drug-target interaction profiling via multi-target SAR models. J Comput Aided Mol Des. 2016;30:413–24.
Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30.
Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25:25–9.
Raudvere U, Kolberg L, Kuzmin I, Arak T, Adler P, Peterson H, et al. G:profiler: a web server for functional enrichment analysis and conversions of gene lists (2019 update). Nucleic Acids Res. 2019;47:W191–w198.
Szklarczyk D, Gable AL, Nastou KC, Lyon D, Kirsch R, Pyysalo S, et al. The STRING database in 2021: customizable protein-protein networks, and functional characterization of user-uploaded gene/measurement sets. Nucleic Acids Res. 2021;49:D605–d612.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504.
Li B, Severson E, Pignon JC, Zhao H, Li T, Novak J, et al. Comprehensive analyses of tumor immunity: implications for cancer immunotherapy. Genome Biol. 2016;17:174.
Zeng D, Ye Z, Wu J, Zhou R, Fan X, Wang G, et al. Macrophage correlates with immunophenotype and predicts anti-PD-L1 response of urothelial cancer. Theranostics. 2020;10:7002–14.
Trott O, Olson AJ. AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J Comput Chem. 2010;31:455–61.
Berman HM, Westbrook J, Feng Z, Gilliland G, Bhat TN, Weissig H, et al. The protein data bank. Nucleic Acids Res. 2000;28:235–42.
Seeliger D, de Groot BL. Ligand docking and binding site analysis with PyMOL and Autodock/Vina. J Comput Aided Mol Des. 2010;24:417–22.
Li X, Liang W, Yu C, Meng Q, Zhang W, Wu X, et al. Potential therapeutic strategies for quercetin targeting critical pathological mechanisms associated with colon adenocarcinoma and COVID-19. Front Pharmacol. 2022;13:988153.
Ji H, Li K, Xu W, Li R, Xie S, Zhu X. Prediction of the mechanisms by which quercetin enhances cisplatin action in cervical cancer: a network pharmacology study and experimental validation. Front Oncol. 2021;11:780387.
Lin M, Pan C, Xu W, Li J, Zhu X. Leonurine promotes cisplatin sensitivity in human cervical Cancer cells through increasing apoptosis and inhibiting drug-resistant proteins. Drug Des Devel Ther. 2020;14:1885–95.
Salomon BL, Leclerc M, Tosello J, Ronin E, Piaggio E, Cohen JL. Tumor necrosis factor α and regulatory T cells in oncoimmunology. Front Immunol. 2018;9:444.
Vredevoogd DW, Kuilman T, Ligtenberg MA, Boshuizen J, Stecker KE, de Bruijn B, et al. Augmenting immunotherapy impact by lowering Tumor TNF cytotoxicity threshold. Cell. 2019;178:585–599e515.
Balkwill F. Tumour necrosis factor and cancer. Nat Rev Cancer. 2009;9:361–71.
Sha J, Du J, Yang J, Hu X, Li L. Changes of serum levels of tumor necrosis factor (TNF-α) and soluble interleukin-2 receptor (SIL 2R) in patients with cervical cancer and their clinical significance. Am J Transl Res. 2021;13:6599–604.
Babapour N, Mehramiz M, Rastgar Moghadam A, Behboodi N, Yousefi Z, Maftouh M, et al. Association of TNF-308 G > A polymorphism located in tumor necrosis factor a with the risk of developing cervical cancer and results of pap smear. J Cell Biochem. 2019;120:5444–8.
Li L, Liu J, Liu C, Lu X. The correlation between TNF-α-308 gene polymorphism and susceptibility to cervical cancer. Oncol Lett. 2018;15:7163–7.
Du GH, Wang JK, Richards JR, Wang JJ. Genetic polymorphisms in tumor necrosis factor alpha and interleukin-10 are associated with an increased risk of cervical cancer. Int Immunopharmacol. 2019;66:154–61.
Martin-Fernandez L, Ziyatdinov A, Carrasco M, Millon JA, Martinez-Perez A, Vilalta N, et al. Genetic determinants of Thrombin Generation and their relation to venous thrombosis: results from the GAIT-2 Project. PLoS ONE. 2016;11:e0146922.
McFadyen JD, Stevens H, Peter K. The emerging threat of (Micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res. 2020;127:571–87.
Campello E, Bulato C, Spiezia L, Boscolo A, Poletto F, Cola M, et al. Thrombin generation in patients with COVID-19 with and without thromboprophylaxis. Clin Chem Lab Med. 2021;59:1323–30.
Dong Y, Ma WM, Shi ZD, Zhang ZG, Zhou JH, Li Y, et al. Role of NRP1 in bladder cancer pathogenesis and progression. Front Oncol. 2021;11:685980.
Chen XJ, Wu S, Yan RM, Fan LS, Yu L, Zhang YM, et al. The role of the hypoxia-Nrp-1 axis in the activation of M2-like tumor-associated macrophages in the tumor microenvironment of cervical cancer. Mol Carcinog. 2019;58:388–97.
Yang L, Liu L, Zhu YH, Wang BB, Chen YN, Zhang F, et al. Neuropilin-1 is associated with the prognosis of cervical cancer in Henan Chinese population. Onco Targets Ther. 2019;12:2911–20.
Dai J, Pan Y, Chen Y, Yao S. A panel of seven immune-related genes can serve as a good predictive biomarker for cervical squamous cell carcinoma. Front Genet. 2022;13:1024508.
Battaglia A, Buzzonetti A, Monego G, Peri L, Ferrandina G, Fanfani F, et al. Neuropilin-1 expression identifies a subset of regulatory T cells in human lymph nodes that is modulated by preoperative chemoradiation therapy in cervical cancer. Immunology. 2008;123:129–38.
Yang S, Cheng H, Huang Z, Wang X, Wan Y, Cai J, et al. Circulating soluble neuropilin-1 in patients with early cervical cancer and cervical intraepithelial neoplasia can be used as a valuable diagnostic biomarke. Dis Markers. 2015;2015:506428.
Yang B, Chen J, Teng Y. TNPO1-mediated nuclear import of fubp1 contributes to tumor immune evasion by increasing NRP1 expression in cervical cancer. J Immunol Res. 2021;2021:9994004.
Akbari M, Akhavan-Bahabadi M, Shafigh N, Taheriazam A, Hussen BM, Sayad A, et al. Expression analysis of IFNAR1 and TYK2 transcripts in COVID-19 patients. Cytokine. 2022;153:155849.
Pairo-Castineira E, Clohisey S, Klaric L, Bretherick AD, Rawlik K, Pasko D, et al. Genetic mechanisms of critical illness in COVID-19. Nature. 2021;591:92–8.
Zheng W, Lin Q, Issah MA, Liao Z, Shen J. Identification of PLA2G7 as a novel biomarker of diffuse large B cell lymphoma. BMC Cancer. 2021;21:927.
Lehtinen L, Vainio P, Wikman H, Huhtala H, Mueller V, Kallioniemi A, et al. PLA2G7 associates with hormone receptor negativity in clinical breast cancer samples and regulates epithelial-mesenchymal transition in cultured breast cancer cells. J Pathol Clin Res. 2017;3:123–38.
Vainio P, Lehtinen L, Mirtti T, Hilvo M, Seppänen-Laakso T, Virtanen J, et al. Phospholipase PLA2G7, associated with aggressive prostate cancer, promotes prostate cancer cell migration and invasion and is inhibited by statins. Oncotarget. 2011;2:1176–90.
Vainio P, Gupta S, Ketola K, Mirtti T, Mpindi JP, Kohonen P, et al. Arachidonic acid pathway members PLA2G7, HPGD, EPHX2, and CYP4F8 identified as putative novel therapeutic targets in prostate cancer. Am J Pathol. 2011;178:525–36.
Morigny P, Kaltenecker D, Zuber J, Machado J, Mehr L, Tsokanos FF, et al. Association of circulating PLA2G7 levels with cancer cachexia and assessment of darapladib as a therapy. J Cachexia Sarcopenia Muscle. 2021;12:1333–51.
Xu C, Reichert EC, Nakano T, Lohse M, Gardner AA, Revelo MP, et al. Deficiency of phospholipase A2 group 7 decreases intestinal polyposis and colon tumorigenesis in apc(Min/+) mice. Cancer Res. 2013;73:2806–16.
Liao Y, Badmann S, Kraus F, Topalov NE, Mayr D, Kolben T, et al. PLA2G7/PAF-AH as potential negative regulator of the Wnt signaling pathway mediates protective effects in BRCA1 mutant breast cancer. Int J Mol Sci. 2023;24:882.
Liao Y, Badmann S, Kaltofen T, Mayr D, Schmoeckel E, Deuster E, et al. Platelet-activating factor acetylhydrolase expression in BRCA1 mutant ovarian cancer as a protective factor and potential negative regulator of the Wnt signaling pathway. Biomedicines. 2021;9:706.
Zalpoor H, Bakhtiyari M, Liaghat M, Nabi-Afjadi M, Ganjalikhani-Hakemi M. Quercetin potential effects against SARS-CoV-2 infection and COVID-19-associated cancer progression by inhibiting mTOR and hypoxia-inducible factor-1alpha (HIF-1alpha). Phytother Res. 2022;36:2679–82.
Kedhari Sundaram M, Raina R, Afroze N, Bajbouj K, Hamad M, Haque S, et al. Quercetin modulates signaling pathways and induces apoptosis in cervical cancer cells. Biosci Rep. 2019;39:BSR20190720.
Acknowledgements
The Fig. 1 was created with BioRender.com. The authors would like to thank the TCGA, GTEx, NCBI, CTD, SwissTargetPrediction, DrugBank, TargetNet, STRING and g:Profiler databases for open access in this section.
Funding
This work was supported by Zhejiang Key Laboratory of Traditional Chinese Medicine for Diagnosis and Treatment of Gynecological Cancers (2022-11) and the Key Lab of Wenzhou city-Gynecological Oncology (ZD201603).
Author information
Authors and Affiliations
Contributions
Conceptualization, ZW and XZ. Data analysis, MC and HJ. Investigation and writing, MC and HJ. Investigation, KL, HL, and MP. Data supervision, editing manuscript, ZW and XZ. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chu, M., Ji, H., Li, K. et al. Investigating the potential mechanism of quercetin against cervical cancer. Discov Onc 14, 170 (2023). https://doi.org/10.1007/s12672-023-00788-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-023-00788-y