Abstract
Background
As ovarian clear cell carcinoma (OCCC) has distinct clinical features, biology, genetic characteristics and mechanisms of pathogenesis, and whether the origin of endometriosis or not affects the prognosis of OCCC remains controversial.
Methods
We retrospectively collected medical records and follow-up data of patients with OCCC treated at the Obstetrics and Gynecology Hospital of Fudan University from January 2009 to December 2019. Further, we divided patients into 2 groups. Group 1: non-endometriosis origin; Group 2: endometriosis origin. Clinicopathological characteristics and survival outcomes were compared between the 2 groups.
Results
A total of one hundred and twenty-five patients with ovarian clear cell carcinoma were identified and included. In the overall patients’ population, the 5 year overall survival was 84.8%, the mean overall survival was 85.9 months. The results of the stratified analysis showed that early stage (FIGO stage I/II) OCCC had a good prognosis. The results of univariate analyses indicated that a statistically significant relationship between overall survival (OS) and FIGO stage, lymph node metastasis, peritoneum metastasis, chemotherapy administration methods, Chinese herbal treatment, molecular target therapy. As for progression-free survival (PFS), a significant relationship between PFS and child-bearing history, largest residual tumor size, FIGO stage, tumor maximum diameter, lymph node metastasis was found, respectively. FIGO stage and lymph node metastasis are common poor prognostic factors affecting OS and PFS. The multivariate regression analysis revealed that FIGO stage (p = 0.028; HR, 1.944; 95% CI 1.073–3.52) and treatment by Chinese herbs (p = 0.018; HR, 0.141; 95% CI 0.028–0.716) were identified as influencing factors with regard to survival. The presence or absence of lymphadenectomy did not affect OS of 125 OCCC patients (p = 0.851; HR, 0.825; 95% CI 0.111–6.153).
There was a trend towards a better prognosis for patients with OCCC of endometriosis origin than those with OCCC of non-endometriosis origin (p = 0.062; HR, 0.432; 95% CI 0.179–1.045). The two groups differed with respect to several clinicopathological factors. And the proportion of patients with disease relapse was higher in Group 1 (46.9%) than in Group 2 (25.0%), with a statistically significant difference (p = 0.048).
Conclusions
Surgical staging and treatment by Chinese herbs postoperatively are two independent prognostic factors affecting the OS of OCCC, early detection and Chinese herbal medicine combined with chemotherapy postoperatively may be a good choice. Tumor with endometriosis-origin was found less likely to relapse. While the non-necessity of lymphadenectomy in advanced ovarian cancer has been proven, the need for lymphadenectomy in the early stage ovarian cancer, including early stage OCCC, still deserved to be explored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Epithelial ovarian cancers (EOCs) is one of the most common gynecologic malignancies with a high mortality rate. BRCA1/2 germline mutations are the strongest known genetic risk factors for EOCs and are found in 6–15% of women with EOC. The BRCA1/2 status can be used for patients’ counselling regarding expected survival, as BRCA1/2 carriers with EOC respond better than non-carriers to platinum-based chemotherapies. This yields greater survival, even though the disease is generally diagnosed at a later stage and higher grade [1]. EOCs are classified into type I and type II [2]; Of these, ovarian clear cell carcinoma (OCCC), endometrioid ovarian carcinoma, mucinous ovarian carcinoma and low-grade serous ovarian carcinoma are classified as type I, while type II is represented by high-grade serous ovarian cancer (HGSOC) [3]. The tumor that is currently classified as ovarian clear cell carcinoma was most likely originally described in 1899 by Peham as “hypernephroma of the ovary”, based on the striking similarity of the reported case to renal clear cell carcinoma [4]. Scully and Barlow’s seminal report [5] was also significant to detail a strong association between endometriosis and OCCC, and introduce the term clear cell carcinoma for these tumor. In 1973, ovarian clear cell carcinoma was included in the World Health Organization (WHO) classification of ovarian tumors [6].
Ovarian clear cell carcinoma (OCCC) is the second most common histological subtype, accounting for 5–25% of all EOCs [7, 8]. The prevalence of OCCC is largely region and ethnicity specific, it accounts for approximately 10% of EOCs in Europe and the United States with a higher incidence of about 10%-25% in Asian populations [9,10,11]. Compared to HGSOC, the most common type of EOC, OCCC has a younger onset, is more likely to be diagnosed in the early stage, is closely associated with endometriosis, and is characterized microscopically by a typical glycogen-filled clear cytoplasm and the presence of hobnail cells with a typical immunohistochemical phenotype [12,13,14,15]. OCCC has a unique genetic profile with a lower p53 mutation rate (25%) and a lower BRCA1/2 mutation rate (6.3%) but higher mutation rates in ARID1A, PIK3CA and PTEN compared to HGSOC [16,17,18,19,20]. Since inflammatory and epigenetic processes seem to play a predominant role in the pathogenesis of OCCC, immune checkpoint inhibitors and targeting the PI3K pathway as well as epigenetic treatment approaches may play an important role in the treatment of these tumor entities [21]. Current treatment recommendation for OCCC is based on data collected from cohort studies based on HGSOC, and surgery combined with postoperative platinum-based chemotherapy is the recommended option [22]. Moreover, we noticed that when mutations occur within DNA repair pathways, there is an increased risk of chemotherapy resistance. Given that a significant proportion of OCCC shows homologous recombination deficiency, they should be susceptible to PARP inhibitor therapy. Among PARP inhibitors, olaparib, rucaparib, and niraparib have been approved by the FDA and/or the EMA in EOC in different settings. Olaparib, rucaparib, and niraparib trap PARP approximately 100-fold more efficiently than veliparib [23]. Early stage OCCC has a better prognosis, while advanced/recurrent patients have a poor prognosis, which is related to their insensitivity to chemotherapy and chemoresistance [24, 25].
More and more studies have confirmed that OCCC and ovarian endometrioid carcinoma are all have close relationships with ovarian endometriotic cysts, which originate from atypical endometrial cells and or possibly endometriotic cells [26,27,28]. Common mutations in OCCC are frequently found in benign endometriosis without malignant lesions, including ARID1A, PIK3CA, PPP2R1A and KRAS. In particular, deletion of ARID1A gene (BAF250a) frequently occurs in atypical endometriosis, which indicates an early role in carcinogenesis [17, 18, 29]. It indicated that endometriosis as the tissue origin of OCCC, they have shared genomic abnormalities and monoclonal relationships (most likely atypical ovarian endometriotic cysts), that OCCC may be caused by malignant transformation of endometriosis with a common genetic pedigree, that known oncogenes cause malignant transformation of ovarian endometriotic epithelium, and the microenvironment of endometriosis also promotes carcinogenesis [30, 31]. In addition, it has been suggested that overexpression of HNF-1β was detected in OCCC and 40% of benign endometriotic cysts [28, 32, 33]. And biological properties such as PD-L1 overexpression and copy number variation (CNV) may promote the cancerous transformation in ovarian endometriosis from a non-invasive precursor lesion to OCCC [34,35,36]. As OCCC has distinct clinical features, biology, genetic characteristics and mechanisms of pathogenesis, as well as the dilemma of insensitivity to chemotherapy, and the exact pathogenesis of ovarian endometriosis to OCCC has not been fully elucidated, further research and exploration are still needed. In this study, we retrospectively collected medical records and follow-up data of patients with OCCC from a single center, particularly those with OCCC of endometriosis and non-endometriosis origin, try to trigger more thinking about the future management of OCCC.
2 Materials and methods
2.1 Patients
Between January 2009 and December 2019, 139 patients were diagnosed with ovarian clear cell carcinoma and treated at Obstetrics and Gynecological Hospital of Fudan University, China. This study was approved by the ethics committee of OB/GYN Hospital of Fudan University. Data were collected from electronic medical records and outpatient visits. All eligible patients had a pathological diagnosis of ovarian clear cell carcinoma in various stages, women with a concurrent malignancy were excluded. In all, 125 women were enrolled in this study.
2.2 Data collection
Data collected included demographic information, clinical, surgical and pathological information, chemotherapy information and follow-up information. Following a electronic medical records search, baseline data were obtained from the database of patients’ medical records and included age at diagnosis, BMI, menopause, parity, personal medical history, comorbid medical disease; Clinical data were also obtained from the patients and included symptom, preoperative tumor markers level, presence or absence of endometriosis, manifestations of endometriosis, duration of endometriosis, whether there is ascites, imaging findings; Surgical and pathological details included surgery mode, complete or incomplete surgery (complete surgical procedure consisted of total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, pelvic and para-aortic lymphadenectomy, and debulking procedures such as colon resection), fertility-sparing surgery (the preservation of the uterus and one adnexa), largest residual tumor size, surgical staging (the International Federation of Obstetrics and Gynecology, FIGO staging system), tumor maximum diameter, peritoneal cytology, lymph node metastasis (preoperative evaluation of retroperitoneal swollen lymph nodes was confirmed by computed tomography and MRI and/or PET-CT), omentum metastasis, peritoneum metastasis, tumor origin (histologically confirmed), postoperative pathological and immunohistochemical results (The pathologic diagnosis was performed and supervised independently by 2 pathologists). Adjuvant therapy (observation or adjuvant chemotherapy, treatment by Chinese herbs, molecular target therapy), chemotherapy circles (adjuvant chemotherapy regimen was a platinum based doublet: carboplatin (AUC = 5–6) and paclitaxel (135–175 mg/m2) every 3 weeks, for 3–6 cycles). Platinum-sensitivity was defined as relapse occurring ≥ 6 months after the completion of last regimen or lack of recurrence and platinum-resistance was defined as relapse occurring within 6 months of the completion of last regimen. Patients came back to our hospital for follow-up evaluation with the interval of 3 months for the first 2 years, with the interval of 6 months for the next 3 years, and annually thereafter. We also collected date of disease progression or death, disease progression details, adjuvant therapy after disease progression, status of the patient at the most recent follow-up. Overall survival (OS) and progression-free survival (PFS) was calculated from the date of primary surgery to death and disease progression/recurrence, respectively, or the last disease-free visit.
2.3 Analysis
The survival analysis was based on the Kaplan–Meier method, and the results were compared using the log-rank test. Cox regression analysis was used to determine factors affecting survival and recurrence, and results are presented as HRs with 95% CIs. The distributions of clinicopathological factors were evaluated using the Student’s t-test or the χ2-test as appropriate. Spearman’s correlation analysis was used to assess the correlation between endometriosis origin and clinicopathological characteristics of OCCC patients. Multivariate survival analysis was performed using Cox regression model including prognostic factors that were significant in univariate analysis. all p values reported are two-tailed and a p < 0.05 was considered significant. All statistical analyses were performed using Statistical Program for Social Sciences (SPSS) (version 19.0).
3 Result
In all, 125 women were surgically diagnosed with OCCC at Obstetrics and Gynecology Hospital of Fudan University during the study period. The characteristics of patients with OCCC involved are shown in Tables 1, 2. Besides, information on the clinical characteristics of the relapsed patients among all OCCC patients is presented in Table 3.
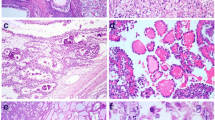
Table 1 shows us the clinical baseline information of the OCCC patients. The mean age at diagnosis was 50 years (range, 29–79 years). 68% of them had a BMI of less than or equal to 24.0 kg/m2. About half of the patients are menopausal (53.6%). 87.2% patients had history of delivery. There were only 2 (1.6%) patients had ovarian cancer family history and only 4 (3.2%) patients had breast cancer history. The most common clinical symptom of OCCC in our study was pelvic mass (56.8%). Pelvic masses are adnexal masses of undetermined origin, benign or malignant, found by the patient or by clinical examination or by imaging tests such as ultrasound, CT, MRI, PET/CT. Of these patients, 52 (41.6%) had a previous history of endometriosis disease. Followed by the most common ovarian endometriotic cyst, 4 patients had peritoneal endometriosis and no one had deep infiltrating endometriosis in the series. Preoperative CA-125 values elevated (≥ 35U/ml) in 83 (66.4%) cases. And among them, 38 cases had normal levels of CA-125. Neutrophil and lymphocyte percentages in pretreatment blood tests were in the normal range in most patients, but the neutrophil percentage tended to rise and the lymphocyte percentage tended to decline. Positive imaging findings account for almost all cases (99.2%). Further, a detailed description of the surgical and pathological characteristics is shown in Table 2. 102 (81.6%) patients with OCCC undergone the primary surgery at our institution and only 23 of them referred after incomplete surgery. Most cases (88.8%) had gone through complete surgical staging procedures and only 2 of them had fertility sparing surgery in hopes of preserving fertility, other patients underwent conservative surgery due to severe complications that excluded them from complete surgical staging. Lymphadenectomy was omitted or replaced by lymph node biopsy in 6 cases because of advanced stage or patient morbidity, and in addition, those who only undergone lymph node biopsy or para-aortic lymphadenectomy without undergoing pelvic lymphadenectomy were not included in the lymphadenectomy group, but a negative biopsy was considered as no lymph node metastasis, a positive para-aortic lymph node was regarded as positive lymph node metastasis. Seventy-four women were treated by laparoscopy, fifty had laparotomy. Upon the surgery, ascites were present in 46 cases and peritoneal cytology was positive in 25 (20.0%) cases while 56 (44.8%) records were unavailable. Tumor diameter with ≤ 50 mm took up 12.8%, 50–100 mm in 46 (36.8%) and > 100 mm in 60 (48.0%) cases. Debulking surgery with residual tumor ≤ 1.0 cm (R0) was achieved in 98.4% of cases. During the procedure, 78.4% of patients received intraoperative chemotherapy, mainly cisplatin. Early-stage disease predominated, the surgical stage was I/II in 100 (80.0%) and III/IV in 23 (18.4%) patients. Among stage I patients, stage IC accounted for the majority (69/89). After reviewing the pathological records of these patients, a total of 70 (56.0%) tumors arose from endometriosis based on the criteria of Sampson and Scott [37] [the criteria include: (1) the coexistence of benign and malignant tissue in the same ovary which have the same histologic relationship to each other as in endometrial carcinoma of the uterine corpus; (2) the carcinoma must actually be seen to arise in this tissue, and not to be invading it from some other source; (3) and additional supportive evidence includes the finding of tissue resembling endometrial stroma surrounding characteristic epithelial glands, and the finding of old hemorrhage rather than fresh, since the latter can be the result of trauma resulting from surgical manipulation. (4) a microscopic section must show the benign endometriosis running into and continuous with the malignant epithelium]. 12 (9.6%) patients had positive lymph node metastases. Twelve of 125 women had omentum metastasis. Peritoneum metastasis occurred in 20 (16.0%) patients. Endometriosis progressed to OCCC within 5 years in 21 patients, representing 30% of the total number. Only 9 patients received neoadjuvant chemotherapy as assessed by their general condition and preoperative Suidan’s CT score [38]. After surgery, 119 (95.2%) patients received a first-line combined chemotherapy with a platinum-based regimen. 58.4% of patients received at least 6 courses of chemotherapy, while 47 (37.6%) patients received lesser courses because of intolerance of side effects or uncomplaisance. Intravenous chemotherapy alone or intravenous combined with intraperitoneal chemotherapy each accounts for approximately half of the postoperative chemotherapy population. The main chemotherapy-related side-effects were manifested as different degrees of myelosuppression (77.6% of the patients). Through our follow-up, we found that 30.4% of the patients received post-operative herbal treatments to regulate their bodies and achieved certain results. Of all patients, only 11 (8.8%) patients received molecular target therapy (mainly with bevacizumab treatment), and they were mainly patients with advanced and relapsed disease. Only one patient received immunotherapy by joining the clinical trial, but stopped the therapy due to the serious side effects and is still alive. None underwent postoperative radiotherapy.
As is shown in Table 3, of the women with follow-up, 38 (30.4%) OCCC patients presented with disease relapse. And among them, 11 (28.9%) had refractory disease, 12 (31.6%) had chemo-resistant disease, and 22 (57.9%) met the criteria for chemo-sensitive disease. 60.5% of recurrent patients were of non-endometriosis origin. The most common manifestation of recurrent disease was imaging-indicated metastases lesions or pathological evidence of metastases (31.6%), followed by elevated tumor markers (26.3%) and local mass based on imaging (23.7%). These patients were also followed for treatment after relapse, chemotherapy remained the mainstay of treatment after relapse (60.5%). A significant number of women (15.8%) had undergone surgical procedure again, primarily to relieve tumor load and remove isolated lesions. It was noted that among the relapsed patients, 11 of them received chemotherapy and molecular target therapy (mainly with bevacizumab treatment) at the same time.
Survival analysis was retrospectively performed to identify the significant outcome predictors that affect disease relapse and survival in patients with OCCC. In the overall patients’ population, the 5 year overall survival was 84.8%, the mean overall survival was 85.9 months (95% CI 79.7–92.1). The median follow-up time from the initial surgery was 58.0 months (range, 10–102 months) (Fig. 1a). We also performed survival analysis for early (stage I-II) and advanced (stage III-IV) stage OCCC respectively, and the results are shown in Fig. 1b and Fig. 1c. Early stage OCCC had a good prognosis, the mean overall survival was 91.9 months (95% CI 86.5–97.2). In comparison, the mean overall survival of advanced OCCC was 51.8 months (95% CI 32.7–71.0), the median overall survival for advanced OCCC was 48 months. A detailed description of the results of univariate analyses on overall survival (p1) and progression-free survival (p2) is shown in Tables 1, 2, it indicated that a statistically significant relationship between survival probability and FIGO stage (p = 0.001), lymph node metastasis (p = 0.002), peritoneum metastasis (p = 0.01), chemotherapy administration methods (p = 0.044), Chinese herbal treatment (p = 0.012), molecular target therapy (p = 0.001), the survival curves of these factors affecting OS are shown in Fig. 2(a, b, c, d, e, f). Among the many characteristics, peritoneal cytology, tumor origin are two clinical factors, which had p values less than 0.1 for univariate analysis of OS, then, we also included these two clinical data in the subsequent multivariate analyses. For analysis of the correlation between clinical data and PFS, a significant relationship between PFS and child-bearing history (p = 0.024), largest residual tumor size (p = 0.014), FIGO stage (p = 0.001), tumor maximum diameter (p = 0.029), lymph node metastasis (p = 0.01) was found, respectively (Fig. 3a, b, c, d, e). The results of multivariate analyses carried out to determine the effect of demographic characteristics and clinical features on overall survival are provided in Table 4
Through our analyses, it revealed that FIGO stage and lymph node metastasis are common poor prognostic factors affecting OS and PFS. Overall survival decreased in patients who developed peritoneum metastases (p = 0.01; HR, 3.453; 95% CI 1.343–8.877), but there was no significant difference in the effect on PFS. Patients treated with intravenous combined with intraperitoneal chemotherapy have a worse prognosis than those treated with intravenous chemotherapy alone (p = 0.044; HR, 2.381; 95% CI 1.025–5.533). Interestingly, in terms of treatment, in addition to post-operative chemotherapy, patients treated with herbal remedies have a better OS (p = 0.012; HR, 0.154; 95% CI 0.036–0.663). However, patients receiving bevacizumab-based molecular target therapy have a poorer prognosis (p = 0.001; HR, 4.819; 95% CI 1.862–12.477). In our analysis, women who have given birth to offspring have a lower risk of disease recurrence (p = 0.024; HR, 0.313; 95% CI 0.114–0.855). Larger tumor diameter was associated with prolonged PFS (p = 0.029; HR, 0.559; 95% CI 0.332–0.943). Whether surgery achieved R0 was associated with recurrence and did not affect OS. A subsequent multivariate regression analysis revealed that FIGO stage (p = 0.028; HR, 1.944; 95% CI 1.073–3.52) and treatment by Chinese herbs (p = 0.018; HR, 0.141; 95% CI 0.028–0.716) were identified as risk factors with regard to survival. Patients who received molecular target therapy were mainly patients with advanced and relapsed disease as mentioned above, so we ignored this factor even though the p value is less than 0.05.
Besides, as is shown in Fig. 4a, we can see that even there was no significant difference between tumor origin and OS, a trend towards a better prognosis for patients with OCCC of endometriosis origin than those with OCCC of non-endometriosis origin (p = 0.062; HR, 0.432; 95% CI 0.179–1.045). To further evaluate the significance of endometriosis origin on the recurrence and prognosis of ovarian clear cell carcinoma (OCCC) and its relationship with other clinical parameters, we divided patients into 2 groups according to the association between ovarian endometriosis and OCCC on pathology. The patients were classified as Group 1 (non-endometriosis origin) if the tumor was not originated from endometriosis. The patients were classified as Group 2 (endometriosis origin) if clear cell carcinoma arose from ovarian endometriosis or if ovarian endometriosis was present and found elsewhere in the ovary. Clinicopathological characteristics and survival outcomes were compared between the 2 groups. The two groups differed with respect to clinicopathological factors, such as age, menopause status, endometriosis disease history, manifestations of endometriosis, pretreatment CA-125 level, referred after incomplete surgery, peritoneal cytology and disease relapse. Of 125 OCCC patients at OB/GYN Hospital of Fudan University during the study period, 70 (56%) patients had OCCC arising from ovarian endometriosis or coexisting ovarian endometriosis elsewhere in the ovary, and 55 (44%) of these patients had OCCC of non-endometriosis origin. The patients’ baseline characteristics and clinico-surgical pathological characteristics between the two groups are presented in Table 5. Group 1 patients were older than Group 2 (p < 0.001), and most OCCC in postmenopausal patients did not have endometriosis origin (Group1), while those with endometriosis origin (Group 2) often appear before menopause (p < 0.001). Having analyzed our data, we have concluded that the majority of patients in Group 2 (70%, p < 0.001) have a history of endometriosis and their presentation mainly appeared as ovarian endometriotic cysts (75.7%, p < 0.001). There were more abnormal CA-125 levels in Group 1 patients than in Group 2 patients prior to surgery (80% vs 55.7%). No differences were found between the two groups in the number of patients underwent complete staging surgery. However, more patients in Group 2 referred after incomplete surgery (p = 0.004). Optimal debulking surgery, which was defined as the size of the largest residual tumor less than or equal to 1.0 cm, was performed in both groups, with 98.2% of patients in Group 1 and 98.6% of patients in Group 2 (p = 0.357). A higher percentage of patients in Group 1 had positive ascites cytology compared to Group 2 (42.1% vs 29.0%). More patients with OCCC of endometriosis origin (Group 2) were in the early stage of cancer (stage I and II, 87.1% vs 73.6%) than patients with OCCC of non-endometriosis origin, advanced-stage diseases (stage III and IV) were more frequent in Group 1 (26.4% vs 12.9%), but among stage I patients, stage IC patients accounted for a greater proportion of Group 2 patients (84.2% vs 65.6%). As for the data on other clinical-surgical pathological features, no differences were observed between the two groups in BMI, parity, symptom, pretreatment neutrophil and lymphocyte percentage, surgery mode, tumor maximum diameter, ascites presence, lymph node metastasis, omentum metastasis, peritoneal metastasis. After surgery, 53 patients (96.4%) in Group 1 and 66 patients (94.3%) in Group 2 received adjuvant chemotherapy (p = 0.59). No differences in chemotherapy cycles, chemotherapy administration methods, chemotherapy-related side-effects, Chinese herbs’ treatment and molecular target therapy were observed between the two group. It is worth noting that the proportion of patients with disease relapse was higher in Group 1 (46.9%) than in Group 2 (25.0%), with a statistically significant difference (p = 0.048), and as is depicted in Fig. 4b, this result is consistent with the previously mentioned the trend of higher 5-year OS in endometriosis origin OCCC patients (Group 2) compared with non-endometriosis origin patients (Group 1) (Fig. 4a), even though there was no statistically significant difference between the two groups in terms of PFS (p = 0.341). And, there were no significant differences in progression/ relapse time, progression/relapse manifestations, chemo-resistance and treatment after progression/relapse demonstrates Table 6 the results of spearman correlation analysis between endometriosis origin of OCCC and clinical indicators of each parameter.
4 Discussion
Many factors can influence and indicate the prognosis of OCCC. With the development of technologies of proteomics, such as mass spectrometry (MS) and protein array analysis, the available novel biomarkers, namely, targeted proteomics, is a key technique that enables the validation and verification of biomarkers that have been discovered. It works with untargeted proteomics to complete the cycle of biomarker discovery and validation. Peptidomics, is the second new sub-division of proteomics and can, also, be used to shed light on new biomarkers. Further, exosomes, play a critical role in intercellular communication and they have emerged as a compelling diagnostic and prognostic biomarkers for OCCC, as they may transport some tumour-associated proteins [39]. And many studies have shown that the clinicopathological stage of the tumor is the most important prognostic factor for OCCC [10, 40]. Other poor prognostic factors include lymphatic vascular invasion, blocked p16 expression, deletion of BAF250a expression, β-catenin nuclear expression, abnormal p53 staining patterns, expression of IMP3, CBX7, Emi1, CXCR4, HOXA10, Glypican 3, MET gene amplification, CCNE1 copy number gain, MDM2 amplification in TP53 wild type cases and multiple somatic copy number variants [41,42,43,44,45].Our studies have suggested important roles of surgical staging and treatment by Chinese herbs postoperatively as two independent prognostic factors. Efficacy and safety of Chinese herbal medicine on ovarian cancer after surgery have been discussed in these years [46]. Researchers found that Chinese herbal medicine treatments significantly improved symptoms and enhanced curative effects. It also showed the unique superior chemotherapy tolerance in quality of patient’s life and minimal toxic and adverse effects due to chemotherapy [47]. Specifically, Chinese herbal medicine combined with chemotherapy after surgery may reduce incidences of gastrointestinal reactions, marrow depression, urinary system symptoms and regulate even boost the immune system [48, 49]. Therefore, when we are keep thinking ovarian cancer for improving outcomes, we should consider proper treatments that are truly palliative and improve symptom control [50]. And treatment should be stratified in accordance not only to prognosis, but also with more emphasis being placed on patients’ experience and on minimizing side effects, for all these reasons, Chinese herbal medicine combined with chemotherapy postoperatively may be a good choice.
What deserved our attention is that among the early stage (FIGO stage I/II) OCCC patients in our study, 97% (97/100) of them underwent lymphadenectomy and 1 patient had lymph node biopsy. And after the confirmation of the final pathology report, we found that of the 23 recurrent patients in early stage, 22 patients who underwent lymphadenectomy did not develop lymph node metastasis. Moreover, the presence or absence of lymphadenectomy did not affect OS of 125 OCCC patients (p = 0.851; HR, 0.825; 95% CI 0.111–6.153) by our data analysis. A prospective randomized controlled study of the effect of lymphadenectomy on survival in early-stage ovarian cancer found that although more positive lymph nodes were detected with systematic lymphadenectomy than with lymph node sampling, the study was not statistically valid enough to analyze the effect of systematic lymphadenectomy on PFS and OS in early-stage ovarian cancer due to the small sample size, and perioperative morbidity and postoperative complications were significantly higher in the systematic lymphadenectomy group than in the lymph node sampling group [51]. According to the previous literature [52], the complication rate of retroperitoneal systematic lymphadenectomy ranges from 5.9% to 24%, with the more serious recent complications occurring in 5.9% to 18.1% of these. Common recent complications include vascular injury, lymphatic cysts, small bowel obstruction and deep vein thrombosis, and possibly urinary fistula and postoperative infection, etc. The main long-term complication is lymphoedema of the lower limbs, which sometimes seriously affects the patient’s quality of life. In addition, lymph nodes are peripheral immune organs located on the way of lymphatic vessels, and their main function is to filter lymphatic fluid and produce immune cells, which participate in the immune response of the body. Although removal of regional lymph nodes blocks one of the metastatic pathways of tumors, it also weakens the anti-tumor immunity of the body. Besides, the functional protection of the immune organs contributes to the immunotherapy of tumors. The role of regional lymph nodes in the tumor immune cycle is crucial, as it is the site of initiation and maintenance of the body’s anti-tumor immune response, and its lack of function will cause a disconnect in the tumor immune cycle, bringing about a failure of immune supervision [53]. Whether systematic lymphadenectomy provides a survival benefit for patients with early-stage ovarian cancer, including those with early-stage OCCC, remains controversial. As mentioned previously in this study, patients with early stage OCCC have a good prognosis which is consistent with previous studies [7, 11, 13]. All these suggest that we may be able to omit lymphadenectomy in early stage OCCC patients, thereby reducing the risk of intraoperative injury, shortening the operative time and reducing the risk of postoperative complications associated with lymphadenectomy itself, and ultimately improving the patients’ postoperative quality of life to some extent. As the results of the various retrospective studies were inconsistent [54,55,56,57] and retrospective studies are vulnerable to the effects of bias from confounding factors, in China, there is an ongoing prospective multicenter randomized controlled study on “the Exemption of early-stage epithelial ovarian cancer from systemic lymphadenectomy”, and our institution, as one of the subcenters, is actively enrolling suitable patients for this clinical study. This multicenter clinical study aims to optimize treatment strategies in the future for early-stage ovarian cancer (including early-stage OCCC) and to provide a new evidence-based basis for updating clinical guidelines. In our study, all 12 patients with positive lymph nodes were advanced stage (FIGO stage III/IV) patients. The rate of positive lymph node metastases is approximately 52.2% (12/23). Even though patients with lymph node metastases had shorter OS (Fig. 2b) and PFS (Fig. 3e) among the 125 OCCC patients. After our stratified analysis of advanced stage OCCC, we found that lymph node metastasis had no significant effect on OS and PFS in patients with advanced disease, and the difference was not statistically significant (OS: p = 0.311; HR, 1.922; 95% CI 0.544–6.792; PFS: p = 0.937; HR, 1.058; 95% CI 0.261–4.287). We also analyzed whether lymphadenectomy affected OS in patients with advanced disease as well, and found that lymph node dissection did not affect OS in these advanced OCCC patients (p = 0.636; HR, 1.666; 95% CI 0.201–13.808). Here, our findings are consistent with those of the LION study [58] recently published in the New England Journal. The LION study suggested that lymphadenectomy did not result in longer PFS or OS in patients with advanced ovarian cancer when there were no clinically suspicious abnormal lymph nodes. According to LION, systemic lymphadenectomy does not provide a survival benefit for patients with advanced ovarian cancer whose lymph nodes are visual normal, but increases the risks and complications of surgery; Systematic lymphadenectomy should not be routinely performed in these patients and international guidelines have been rewritten as a result [22].
Previous studies have reported conflicting outcomes regarding the prognostic role of endometriosis in OCCC [40, 59,60,61,62,63]. In our study, OCCC with endometriosis origin showed a trend toward improved survival outcomes. OCCC with endometriosis was found younger, more in early stage, more referred after incomplete surgery due to its unexpectedly diagnosis during surgery for young women with presumed endometrioma, more presented with intraoperative tumor rupture while had a lower incidence of positive ascites cytology, which is in line with previous studies [30, 60]. There may be a difference in the pathogenesis and underlying biology of OCCC in patients with endometriosis origin. Therefore, further studies are required to explore the molecular mechanisms of pathogenesis, molecular genetic features of OCCC derived from endometriosis.
5 Conclusions
In conclusion, patients with ovarian clear cell carcinoma are younger, tend to present at an early stage, tumors with or without endometriosis origin have different clinical features in many aspects. Genetic, epigenetic, metabolic and immunological factors interact or combine with each other and are induced or directly influenced by specific microenvironments to lead to the development of OCCC. The early stage and proper Chinese herbal medicine treatment postoperatively are important independent factors to improve patients’ prognosis. While the non-necessity of lymphadenectomy in advanced ovarian cancer has been proven, we here again question the necessity of lymphadenectomy in the early stage ovarian cancer. A multi-center clinical trial is currently underway in China and its results will be used to guide gynecologic surgeon in deciding the scope of surgery and selecting proper regimen for their patients. Surely, our study in the present has several limitations, which include the potential inherited unmeasured biases associated with its retrospective nature, the small sample size, single-institution study and variable follow-up length. Hence, larger-scale, prospective, randomized and well-controlled studies are required to confirmed the findings presented herein.
Data availability
The original contributions presented in the study are included in the article material. Further inquiries can be directed to the corresponding author.
Abbreviations
- OCCC:
-
Ovarian clear cell carcinoma
- FIGO:
-
The International Federation of Obstetrics and Gynecology
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- EOCs:
-
Epithelial ovarian cancers
- HGSOC:
-
High-grade serous ovarian cancer
- WHO:
-
World Health Organization
- CNV:
-
Copy number variation
- PD-L1:
-
Programmed cell death-ligand 1
- BMI:
-
Body mass index
- MRI:
-
Magnetic resonance imaging
- PET-CT:
-
Positron emission tomography-computed tomography
- CA-125:
-
Carbohydrate antigen 125
- SPSS:
-
Statistical Program for Social Sciences
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- OB/GYN:
-
Obstetrics and gynecology
- PARP:
-
Poly(ADP-ribose) polymerase
References
Shah S, Cheung A, Kutka M, Sheriff M, Boussios S. Epithelial ovarian cancer: providing evidence of predisposition genes. Int J Environ Res Public Health. 2022;19(13):8113.
Kurman RJ, Shih IM. The dualistic model of ovarian carcinogenesis: revisited, revised, and expanded. Am J Pathol. 2016;186(4):733–47.
Peres LC, Cushing-Haugen KL, Kobel M, Harris HR, Berchuck A, Rossing MA, et al. Invasive epithelial ovarian cancer survival by histotype and disease stage. J Natl Cancer Inst. 2019;111(1):60–8.
Fadare O, Parkash V. Pathology of endometrioid and clear cell carcinoma of the ovary. Surg Pathol Clin. 2019;12(2):529–64.
Scully RE, Barlow JF. “Mesonephroma” of ovary tumor of müllerian nature related to the endometrioid carcinoma. Cancer. 1967;20(9):1405–17.
Scully RE. World Health Organization classification and nomenclature of ovarian cancer. Natl Cancer Inst Monogr. 1975;42:5–7.
Mabuchi S, Sugiyama T, Kimura T. Clear cell carcinoma of the ovary: molecular insights and future therapeutic perspectives. J Gynecol Oncol. 2016;27(3): e31.
Shimizu D, Sato N, Sato T, Makino K, Kito M, Shirasawa H, et al. Impact of adjuvant chemotherapy for stage I ovarian carcinoma with intraoperative tumor capsule rupture. J Obstet Gynaecol Res. 2015;41(3):432–9.
Matsuzaki S, Yoshino K, Ueda Y, Matsuzaki S, Kakuda M, Okazawa A, et al. Potential targets for ovarian clear cell carcinoma: a review of updates and future perspectives. Cancer Cell Int. 2015;15(1):1–13.
Iida Y, Okamoto A, Hollis RL, Gourley C, Herrington CS. Clear cell carcinoma of the ovary: a clinical and molecular perspective. Int J Gynecol Cancer. 2021;31(4):605–16.
Tang H, Liu Y, Wang X, Guan L, Chen W, Jiang H, et al. Clear cell carcinoma of the ovary: clinicopathologic features and outcomes in a Chinese cohort. Medicine (Baltimore). 2018;97(21): e10881.
Fridley BL, Dai J, Raghavan R, Li Q, Winham SJ, Hou X, et al. Transcriptomic characterization of endometrioid, clear cell, and high-grade serous epithelial ovarian carcinoma. Cancer Epidemiol Biomarkers Prev. 2018;27(9):1101–9.
Fujiwara K, Shintani D, Nishikawa T. Clear-cell carcinoma of the ovary. Ann Oncol. 2016;27(Suppl 1):i50–2.
Khalique S, Lord CJ, Banerjee S, Natrajan R. Translational genomics of ovarian clear cell carcinoma. Semin Cancer Biol. 2020;61:121–31.
Yamaguchi K, Mandai M, Oura T, Matsumura N, Hamanishi J, Baba T, et al. Identification of an ovarian clear cell carcinoma gene signature that reflects inherent disease biology and the carcinogenic processes. Oncogene. 2010;29(12):1741–52.
Winterhoff B, Hamidi H, Wang C, Kalli KR, Fridley BL, Dering J, et al. Molecular classification of high grade endometrioid and clear cell ovarian cancer using TCGA gene expression signatures. Gynecol Oncol. 2016;141(1):95–100.
Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363(16):1532–43.
Samartzis EP, Noske A, Dedes KJ, Fink D, Imesch P. ARID1A mutations and PI3K/AKT pathway alterations in endometriosis and endometriosis-associated ovarian carcinomas. Int J Mol Sci. 2013;14(9):18824–49.
Jung US, Min KW, Kim DH, Kwon MJ, Park H, Jang HS. Suppression of ARID1A associated with decreased CD8 T cells improves cell survival of ovarian clear cell carcinoma. J Gynecol Oncol. 2021;32(1): e3.
Bitler BG, Fatkhutdinov N, Zhang R. Potential therapeutic targets in ARID1A-mutated cancers. Expert Opin Ther Targets. 2015;19(11):1419–22.
Samartzis EP, Labidi-Galy SI, Moschetta M, Uccello M, Kalaitzopoulos DR, Perez-Fidalgo JA, et al. Endometriosis-associated ovarian carcinomas: insights into pathogenesis, diagnostics, and therapeutic targets-a narrative review. Ann Transl Med. 2020;8(24):1712.
Armstrong DK, Alvarez RD, Backes FJ, Bakkum-Gamez JN, Barroilhet L, Behbakht K, et al. NCCN guidelines® insights: ovarian cancer, version 3 2022. J Natl Comp Cancer Network JNCCN. 2022;20(9):972–80.
Boussios S, Rassy E, Moschetta M, Ghose A, Adeleke S, Sanchez E, et al. BRCA mutations in ovarian and prostate cancer: bench to bedside. Cancers (Basel). 2022;14(16):3888.
Nasioudis D, Mastroyannis SA, Albright BB, Haggerty AF, Ko EM, Latif NA. Adjuvant chemotherapy for stage I ovarian clear cell carcinoma: patterns of use and outcomes. Gynecol Oncol. 2018;150(1):14–8.
Sugiyama T, Okamoto A, Enomoto T, Hamano T, Aotani E, Terao Y, et al. Randomized phase III trial of irinotecan plus cisplatin compared with paclitaxel plus carboplatin as first-line chemotherapy for ovarian clear cell carcinoma: JGOG3017/GCIG trial. J Clin Oncol. 2016;34(24):2881–7.
Yamada Y, Shigetomi H, Onogi A, Haruta S, Kawaguchi R, Yoshida S, et al. Redox-active iron-induced oxidative stress in the pathogenesis of clear cell carcinoma of the ovary. Int J Gynecol Cancer. 2011;21(7):1200–7.
Van Gorp T, Amant F, Neven P, Vergote I, Moerman P. Endometriosis and the development of malignant tumours of the pelvis a review of literature. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):349–71.
Suda K, Cruz Diaz LA, Yoshihara K, Nakaoka H, Yachida N, Motoyama T, et al. Clonal lineage from normal endometrium to ovarian clear cell carcinoma through ovarian endometriosis. Cancer Sci. 2020;111(8):3000–9.
Oda K, Hamanishi J, Matsuo K, Hasegawa K. Genomics to immunotherapy of ovarian clear cell carcinoma: unique opportunities for management. Gynecol Oncol. 2018;151(2):381–9.
Kobayashi H, Yamada Y, Kawahara N, Ogawa K, Yoshimoto C. Integrating modern approaches to pathogenetic concepts of malignant transformation of endometriosis. Oncol Rep. 2019;41(3):1729–38.
Munksgaard PS, Blaakaer J. The association between endometriosis and ovarian cancer: a review of histological, genetic and molecular alterations. Gynecol Oncol. 2012;124(1):164–9.
Matsuzaki S, Yoshino K, Ueda Y, Matsuzaki S, Kakuda M, Okazawa A, et al. Potential targets for ovarian clear cell carcinoma: a review of updates and future perspectives. Cancer Cell Int. 2015;15:117.
Kim SI, Lee JW, Lee M, Kim HS, Chung HH, Kim JW, et al. Genomic landscape of ovarian clear cell carcinoma via whole exome sequencing. Gynecol Oncol. 2018;148(2):375–82.
Müller R, Uehara Y, Oda K, Ikeda Y, Koso T, Tsuji S, et al. Integrated copy number and expression analysis identifies profiles of whole-arm chromosomal alterations and subgroups with favorable outcome in ovarian clear cell carcinomas. Plos One. 2015;10(6):e128066.
Willis BC, Sloan EA, Atkins KA, Stoler MH, Mills AM. Mismatch repair status and PD-L1 expression in clear cell carcinomas of the ovary and endometrium. Mod Pathol. 2017;30(11):1622–32.
Hamanishi J, Mandai M, Ikeda T, Minami M, Kawaguchi A, Murayama T, et al. Safety and antitumor activity of anti-PD-1 antibody, nivolumab, in patients with platinum-resistant ovarian cancer. J Clin Oncol. 2015;33(34):4015–22.
Scott RB. Malignant changes in endometriosis. Obstet Gynecol. 1953;2(3):283–9.
Suidan RS, Ramirez PT, Sarasohn DM, Teitcher JB, Mironov S, Iyer RB, et al. A multicenter prospective trial evaluating the ability of preoperative computed tomography scan and serum CA-125 to predict suboptimal cytoreduction at primary debulking surgery for advanced ovarian, fallopian tube, and peritoneal cancer. Gynecol Oncol. 2014;134(3):455–61.
Ghose A, Gullapalli SVN, Chohan N, Bolina A, Moschetta M, Rassy E, et al. Applications of proteomics in ovarian cancer: dawn of a new era. Proteomes. 2022;10(2):16.
Scarfone G, Bergamini A, Noli S, Villa A, Cipriani S, Taccagni G, et al. Characteristics of clear cell ovarian cancer arising from endometriosis: a two center cohort study. Gynecol Oncol. 2014;133(3):480–4.
Itamochi H, Oishi T, Oumi N, Takeuchi S, Yoshihara K, Mikami M, et al. Whole-genome sequencing revealed novel prognostic biomarkers and promising targets for therapy of ovarian clear cell carcinoma. Br J Cancer. 2017;117(5):717–24.
Murakami R, Matsumura N, Brown JB, Higasa K, Tsutsumi T, Kamada M, et al. Exome sequencing landscape analysis in ovarian clear cell carcinoma shed light on key chromosomal regions and mutation gene networks. Am J Pathol. 2017;187(10):2246–58.
Ngoi NY, Heong V, Ow S, Chay WY, Kim HS, Choi CH, et al. A multicenter phase II randomized trial of durvalumab (MEDI-4736) versus physician’s choice chemotherapy in recurrent ovarian clear cell adenocarcinoma (MOCCA). Int J Gynecol Cancer. 2020;30(8):1239–42.
Yamamoto S, Tsuda H, Miyai K, Takano M, Tamai S, Matsubara O. Accumulative copy number increase of MET drives tumor development and histological progression in a subset of ovarian clear-cell adenocarcinomas. Mod Pathol. 2012;25(1):122–30.
Yamashita Y, Akatsuka S, Shinjo K, Yatabe Y, Kobayashi H, Seko H, et al. Met is the most frequently amplified gene in endometriosis-associated ovarian clear cell adenocarcinoma and correlates with worsened prognosis. PLoS ONE. 2013;8(3): e57724.
Wang R, Sun Q, Wang F, Liu Y, Li X, Chen T, et al. Efficacy and safety of Chinese herbal medicine on ovarian cancer after reduction surgery and adjuvant chemotherapy: a systematic review and meta-analysis. Front Oncol. 2019;9:730.
Xu X, Zhu L, Long L. Comparison of the effect of traditional Chinese medicine injection combined with chemotherapy and chemotherapy alone on the prognosis, quality of life and immune function in patients with ovarian carcinoma: a protocol for systematic review and network meta-analysis. Medicine (Baltimore). 2021;100(41): e27395.
Zhang B, Dan W, Zhang G, Wang X. Molecular mechanism of gleditsiae spina for the treatment of high-grade serous ovarian cancer based on network pharmacology and pharmacological experiments. Biomed Res Int. 2022;2022:5988310.
Wang KL, Yu YC, Hsia SM. Perspectives on the Role of Isoliquiritigenin in cancer. Cancers (Basel). 2021;13(1):115.
Vaughan S, Coward JI, Bast RC Jr, Berchuck A, Berek JS, Brenton JD, et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat Rev Cancer. 2011;11(10):719–25.
Maggioni A, Benedetti Panici P, Dell’Anna T, Landoni F, Lissoni A, Pellegrino A, et al. Randomised study of systematic lymphadenectomy in patients with epithelial ovarian cancer macroscopically confined to the pelvis. Br J Cancer. 2006;95(6):699–704.
Ushijima K. Management of retroperitoneal lymph nodes in the treatment of ovarian cancer. Int J Clin Oncol. 2007;12(3):181–6.
Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10.
Komiyama S, Aoki D, Tominaga E, Susumu N, Udagawa Y, Nozawa S. Prognosis of Japanese patients with ovarian clear cell carcinoma associated with pelvic endometriosis: clinicopathologic evaluation. Gynecol Oncol. 1999;72(3):342–6.
Oshita T, Itamochi H, Nishimura R, Numa F, Takehara K, Hiura M, et al. Clinical impact of systematic pelvic and para-aortic lymphadenectomy for pT1 and pT2 ovarian cancer: a retrospective survey by the Sankai gynecology study group. Int J Clin Oncol. 2013;18(6):1107–13.
Abe A, Furumoto H, Irahara M, Ino H, Kamada M, Naka O, et al. The impact of systematic para-aortic and pelvic lymphadenectomy on survival in patients with optimally debulked ovarian cancer. J Obstet Gynaecol Res. 2010;36(5):1023–30.
Ercelep O, Ozcelik M, Gumus M. Association of lymphadenectomy and survival in epithelial ovarian cancer. Curr Probl Cancer. 2019;43(2):151–9.
Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Engl J Med. 2019;380(9):822–32.
Zhao T, Shao Y, Liu Y, Wang X, Guan L, Lu Y. Endometriosis does not confer improved prognosis in ovarian clear cell carcinoma: a retrospective study at a single institute. J Ovarian Res. 2018;11(1):53.
Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT, et al. Significance of ovarian endometriosis on the prognosis of ovarian clear cell carcinoma. Int J Gynecol Cancer. 2018;28(1):11–8.
Kim HS, Kim MA, Lee M, Suh DH, Kim K, No JH, et al. Effect of Endometriosis on the prognosis of ovarian clear cell carcinoma: a two-center cohort study and meta-analysis. Ann Surg Oncol. 2015;22(8):2738–45.
Noli S, Cipriani S, Scarfone G, Villa A, Grossi E, Monti E, et al. Long term survival of ovarian endometriosis associated clear cell and endometrioid ovarian cancers. Int J Gynecol Cancer. 2013;23(2):244–8.
Orezzoli JP, Russell AH, Oliva E, Del Carmen MG, Eichhorn J, Fuller AF. Prognostic implication of endometriosis in clear cell carcinoma of the ovary. Gynecol Oncol. 2008;110(3):336–44.
Acknowledgements
The authors thank all the patients who voluntarily provided clinical information for research use.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Wei Jiang and Mingming Sun conceived the project and designed the study; Mingming Sun acquired data, performed statistical analysis and wrote the first draft of the manuscript; Wei Jiang provided critical revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was conducted following a protocol (2021–81) approved by the ethics committee of the Obstetrics and Gynecology Hospital of Fudan University in accordance with the 1964 Helsinki Declaration. Each participant gave a consent at enrolment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, M., Jiang, W. Ovarian clear cell carcinoma with or without endometriosis origin in a single institution cohort. Discov Onc 14, 39 (2023). https://doi.org/10.1007/s12672-023-00649-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-023-00649-8