Abstract
Objectives
Mindfulness-based programs (MBPs) at the workplace have attracted increasing interest due to their positive effects on health and work-related outcomes. However, it is unclear whether these effects translate into reductions in cost-related and objectively assessed outcomes, such as sick days. The aim of this study was to evaluate the effectiveness of an MBP for supervisors on reduction of sick days of both supervisors and their employees.
Method
We conducted a quasi-experimental study comparing the effects of a 3-day MBP for supervisors to a passive control cohort based on propensity score matching. Sick days for supervisors (n = 13 in the MBP group; n = 269 in the control group) and their employees (n = 196 in the MBP group; n = 1352 in the control group) were drawn directly from their health insurance records over 4 years; 2 years before (pre) and 2 years after (post) the start of the intervention. A generalized linear model was used to analyze sick days after the intervention, adjusted for pre-intervention sick days.
Results
Supervisors in the MBP condition showed significantly lower nonspecific (general) sick days (M = 13.9 days) compared to their matched controls at post-intervention (M = 32.9 days, χ2[1] = 4.38, p = 0.036, d=0.47). Sensitivity analyses showed that this effect was driven mainly by an increase in sick days in the control group. At the employee level, both specific and nonspecific sick days did not differ significantly between the MBP and control conditions.
Conclusions
Our results indicate that MBPs for supervisors at the workplace have the potential to positively affect their nonspecific sick days. Although these effects did not occur at the employee level, the data provide a first indication that MBPs offered at the workplace might be cost-effective.
Preregistration
The study was preregistered at the German Register of Clinical Studies (DRKS-ID: DRKS00013635).
Similar content being viewed by others
Workplace characteristics have a strong impact on individuals’ mental health (Demerouti et al., 2001). While resources and positive experiences at work contribute to strengthening mental health (e.g., Bono et al., 2013), workplace demands and work stress lead to increased mental distress and long-term health impairments (e.g., Almroth et al., 2022). Such elevated levels of mental distress are associated with high individual suffering and reduced work performance (Ford et al., 2011), as well as increased absence days and societal costs (Darr & Johns, 2008; Hassard et al., 2018; Müller et al., 2021; Schmidt et al., 2019). Population-based estimates for Germany show a steady 53% increase in days absent from work due to mental illness from 2011 to 2021 (Meyer et al., 2022). In addition, 11.4% of the German labor force reported sick days due to mental disorders in 2021, with an average duration of incapacity of 29.7 days (Meyer et al., 2022). According to current projections, the economic burden of mental disorders will continue to increase in the coming years, direct and indirect medical costs due to mental illness are expected to more than double (by a factor of 2.4) between 2010 and 2030, and the global loss in economic output (lost workdays) during this period is expected to be US$16.3 trillion worldwide (Bloom et al., 2011; Eaton et al., 2018).
Thus, the development and implementation of workplace health promotion programs have been proposed to have beneficial effects for employees, organizations, and society. Accordingly, the WHO has suggested that a workplace mental health policy for organizations “will benefit the health of employees, increase productivity for the company and will contribute to the wellbeing of the community at large” (World Health Organization, 2005, p. 7).
Supervisors play a key role in promoting mental health in the workplace (Inceoglu et al., 2021). They design aspects of the work environment, act as role models for their employees, and interact directly with them through their leadership behavior and leadership style (e.g., Kranabetter & Niessen, 2017; Montano et al., 2017). In addition, previous research has shown that supportive leadership behavior has the potential to reduce absenteeism, presenteeism, and associated costs (Schmid et al., 2017). Thus, supervisory training has been suggested as an important measure to promote workplace health (Kelloway & Barling, 2010).
Among workplace health promotion programs, mindfulness-based programs (MBPs) have taken a prominent position (e.g., Jamieson & Tuckey, 2017). This is reflected in a significant increase of empirical studies examining MBPs in the workplace setting (Vonderlin et al., 2020). Current meta-analyses indicate positive effects on participants’ health and well-being, as well as positive effects on work-related outcomes, such as job satisfaction and work engagement (Bartlett et al., 2019; Lomas et al., 2019; Vonderlin et al., 2020). Given these results, mindfulness has also been discussed as improving leadership capacities (Baron et al., 2018; Donaldson-Feilder et al., 2019; Vonderlin et al., 2021). Both components of mindfulness, as defined by Bishop et al. (2004), have been discussed with regard to improve supervisors’ orientation toward themselves and their orientation toward their employees (Vonderlin et al., 2021; Zhang et al., 2020).
The self-regulation of attention to the present moment has been discussed to increase supervisors’ awareness to own thoughts, feelings, and bodily sensations and how they change over time (Nübold et al., 2020). This should improve supervisors’ intrapersonal skills to observe current stressors and strains as well as own limits, opening the opportunity to engage in effective coping (e.g., Roche et al., 2014). In addition, this component has been discussed to reduce rumination and to improve detachment from work thereby fostering effective recovery (Hülsheger et al., 2015).
The orientation to one’s experiences with curiosity, openness, and acceptance has been proposed to enhance problem-solving and facilitate coping with uncertainty (Jacobs & Blustein, 2008; Ostafin & Kassman, 2012). This could improve not only supervisors’ intrapersonal skills to effectively cope with their own workplace stressors, but also their interpersonal skills to support their employees’ in effectively coping with stressful work events (i.e., supportive leadership; Pinck & Sonnentag, 2018).
Although mindfulness has been viewed as having a positive impact on leadership capacities, the implementation of MBPs is associated with substantial financial costs that have been estimated at between US$515 and $1217 per participant, including opportunity costs associated with employees’ participation, program-required costs related to coordination, facilitation, and supplies for the program, as well as ancillary costs related to facilitator travel, room rental, and food for the program implementation (Doyle et al., 2019). When implementing MBPs in workplaces with high workloads and limited financial resources in particular (e.g., health sector), the cost-effectiveness of MBPs is of special interest (van Dongen et al., 2016).
To explore potential win-win situations for MBPs at the workplace, it is important to analyze outcomes that reflect both workforce health and cost-saving effects for organizations. One outcome of particular interest here is to focus on sickness absenteeism, defined as health-related absence days from work (Johns, 2010) since they reflect on both individual health status and financial impact due to productivity loss for employers and society (Müller et al., 2021).
Previous research findings relating trait mindfulness to health-related absenteeism show promising results. Accordingly, trait mindfulness has been shown to enhance participants’ quality of life and is, in turn, positively related to their work ability and their return to work after sickness (Vindholmen et al., 2014). Thus, supervisor mindfulness could also have a positive impact on their own sickness-related absenteeism. In addition, we would assume that supervisor mindfulness could also have a positive impact on their employees’ sickness-related absenteeism for two major reasons. First, supervisor mindfulness has been positively associated with employee health in the workplace, which could preventively reduce sick days before they occur (Reb et al., 2014). Second, supervisor mindfulness has been associated with a compassionate communication style and a trustful relationship (Arendt et al., 2019; Stedham & Skaar, 2019), which could help supervisors appropriately guide return to work after illness and facilitate a faster return.
However, empirical evidence on the intervention effects of MBPs on absence days is scarce, showing considerable limitations and mixed results. Anderson (2021) investigated the sickness and absence rates of nurses in critical care in a pre- and post-intervention design containing a sample of n = 25 nurses. Results showed no significant change in sickness rates from pre- to post-intervention. Levett et al. (2019) investigated the effects of an MBP on sick days on an organizational level. They looked at sick days over a 2-year period at an organization that has offered an MBP for its employees. Results demonstrate a significant reduction in sick leave, with a standardized mean difference of d = 0.49. However, they did not include a control group, and sick days were not analyzed on an individual level taking into account whether and how often employees have participated in an MBP. Netterstrøm et al. (2013) investigated whether a mindfulness-based program in general care contributes to the return to work after sickness. Compared to a wait-list (WL) control group and a treatment as usual (TAU) group, the MBP group showed significantly higher rates of participants returning to full-time work after treatment (MBP: 67%; TAU: 36%; WL: 24%). Last, Roeser et al. (2013) found that an MBP for teachers had a positive effect on participants’ blood pressure; however, sick-day absenteeism from work showed no significant reduction. Given this limited and heterogeneous empirical evidence, it has been suggested that investigating the intervention effects of MBPs on objectively assessed health measures, like sick days, is an important issue for future research to explore (Chin et al., 2019).
At the supervisor level, empirical evidence on MBPs on absence days show mixed results. Żołnierczyk-Zreda et al. (2016) investigated the effects of an MBP for middle-level managers in a controlled study design. They found a significant reduction in sickness absence in the MBP compared to the control group.
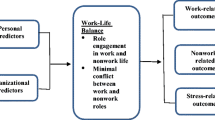
These results suggest that MBPs might be effective for reducing sick days among supervisors by helping them to effectively cope with their own workplace stressors and improve their overall health status (e.g., Vonderlin et al., 2020). However, it remains unclear whether these positive effects translate to the employee level. According to the theoretical model of health-oriented leadership (HoL; Franke et al., 2014), improving supervisors’ health awareness, their value for health, and their health-related behavior should also affect outcomes at the employee level. HoL distinguishes between health-oriented self-care and staff care, assuming that both orientations influence the health of employees. Self-care is considered to have an indirect effect, as supervisors act as role models for their employees. Staff care is thought to have a direct impact on employee health. This would suggest that a health-oriented leadership intervention should also have beneficial effects at the employee level.
Regarding leadership literature, a recent meta-analysis identified two studies investigating the effect of a health-oriented leadership intervention on employees’ sick days (Dannheim et al., 2022). The two studies show marginally (Stansfeld et al., 2015) and statistically significant effects (Milligan-Saville et al., 2017), respectively, of the leadership intervention on the employee level. However, these interventions were not based on mindfulness training.
Given the limited empirical evidence of mindfulness-based leadership interventions on the sickness-related absenteeism of supervisors and their staff, our study aims to investigate whether a systematic organizational mindfulness-based leadership program offered at the workplace has the potential to lower supervisors’ and employees’ sickness-related absenteeism compared to a control group not receiving the intervention.
For the intervention, a mindfulness-based program for supervisors aimed at improving their mental health as well as their leadership style was developed and has been investigated on both the supervisor and employee levels. Through self-report questionnaires, the intervention showed significant effects on supervisors’ health-oriented staff care as well as self-care and mental health, with small to medium effect sizes. In addition, this significant effect on supervisors’ mental health was moderated by the amount of their mindfulness practice and mediated by an increase in their health-oriented self-care. No significant effects were obtained on the employee level mental distress and their evaluation of supervisors’ staff-care. Results of psychometric assessments are published elsewhere (Vonderlin et al., 2021). The present study aimed to extend these findings by examining whether these intervention effects on psychometric outcomes also affect objectively assessed cost-relevant measures, i.e., sickness-related absenteeism. These findings inform decision makers in organizations who are considering implementing MBPs for their staff and have a special interest in the cost-effectiveness of such interventions. In particular, in sectors with limited financial resources, such as the healthcare system or other non-profit organizations, this represents an important prerequisite for large-scale implementation of MBPs (Doyle et al., 2019).
Method
Data were used from a large intervention study to promote workplace health, which was conducted between August 2017 and February 2019 in Germany (Vonderlin et al., 2021). The study project aimed to assess the effectiveness of a mindfulness- and skill-based health-promoting leadership intervention at the supervisor and employee levels on multiple outcomes. While the effects on psychometric questionnaire data have been published elsewhere (Vonderlin et al., 2021), the present work goes beyond these previously published data by focusing on objectively assessed sickness absence data. Power calculations were conducted prior to the start of the study based on a pilot trial to estimate the sample size needed. Based on the results, we aimed to include at least 198 supervisors (99 per group) and 1381 employees (691 per group) to detect medium effect sizes at the supervisor level and small effect sizes at the employee level in the psychometric analyses. The power analysis was conducted using the software G-Power 3.1 (Faul et al., 2007). Of the 12 companies that participated in the study, five companies consented to participate in an additional analysis to examine potential intervention effects on work sick days.
Participants
Participants in the intervention group (IG) were recruited from organizations participating in the study. Inclusion criteria for the organizations to take part were that (a) they carried out at least one complete series of seminars (see below for a description of the intervention), each with 10 to 13 supervisors from the same hierarchical level; (b) they agreed to conduct surveys of supervisors and employees; and (c) they provided the opportunity for an information event to be offered at their workplace before the start of the study. A total of 12 organizations registered for the IG (N = 147 supervisors and N = 1731 employees). Five of these companies from two branches (science and healthcare) consented to participate in the analysis of work disability data (n = 55 supervisors and n = 349 employees). Work disability data could be collected only from participants who were insured through the cooperating health insurance company (n = 14 supervisors and n = 255 employees). In addition, we had to exclude certain participants because (i) work disability data were incomplete (n = 1 supervisor, n = 21 employees), or (ii) data on variables included as covariates in the statistical model were missing or incorrect (n = 38 employees). Finally, data from a total of n = 13 supervisors and n = 196 employees in the IG could be analyzed.
Study participants in the control group (CG) included adult healthcare insurance holders who did not take part in the intervention program. To achieve the highest possible level of comparability, we recruited study participants in the CG in two steps using propensity score matching (PSM)—a statistical method to build comparable CGs in observational studies (Austin, 2011). During the first step, a cohort of N = 59,846 participants were selected via PSM, including their potentially relevant covariates that are routinely recorded for all healthcare insurance holders (age, sex, supervisor (yes/no), employment (full-/part-time), branch) and invited to participate in the study. By mail, they received a cover letter with information about the study, including a questionnaire for psychometric evaluation of the intervention, and an informed consent form asking them to provide written consent for analysis of their work disability data for scientific purposes, which were routinely collected by their health insurer. Participants were asked to return their signed consent form by mail to participate in the study. A total of n = 848 supervisors and 5546 employees consented to participate in the CG of the evaluation study. Of those, n = 297 supervisors and n = 1532 employees were insured by the cooperating health insurance company and gave their consent to analyze their work disability data. In addition, we had to exclude some participants because (i) work disability data were incomplete (n = 3 supervisors, n = 14 employees), or (ii) data on variables included as covariates in the statistical model were missing or incorrect (n = 166 supervisors, n = 25 employees). This led us to a final sample of n = 269 supervisors and n = 1352 employees in the CG that could be analyzed (Fig. 1).
Procedure
The mindfulness and skill-based leadership intervention was developed by the authors of this study in collaboration with a German health insurance company based on the HoL concept of Franke et al. (2014). It consisted of 3 full-day courses and two 3-hr booster sessions: (a) health-promoting self-care, (b) health-promoting staff care, and (c) addressing employees under stress. The aim of the intervention was to promote supervisors’ health-related awareness and their value of health, as well as their health-behavior (Franke et al., 2014). To address the dimension corresponding to “value of health,” all the courses included information transfers, demonstrating their scientific backgrounds and emphasizing the importance of each topic. To address the dimension corresponding to “health behavior,” all the courses focused on teaching practical everyday skills to foster behavioral change. To address the dimension corresponding to “health awareness,” all the courses were based on mindfulness practices.
Mindfulness training was delivered according to the mindfulness concept developed in dialectical behavior therapy (Linehan, 2014). This concept focuses on mindfulness practice under daily life conditions and on mindfulness as a skills-based approach rather than on long meditation exercises (Baer, 2015). Meanwhile, this skills-based approach is also being used in healthy populations to facilitate the application of mindfulness in participants’ daily lives (e.g., Lothes et al., 2021; Lyssenko et al., 2015). Various short mindfulness exercises were practiced in which participants learned to focus and open their minds nonjudgmentally, effectively, and one-mindfully (i.e., doing one thing at a time) toward the present moment (How-Skills) to observe what is going on inside and outside without doing anything to change; to describe their thoughts, feelings, and sensations by adding words to their observations; and to participate and immerse themselves in the present moment of their daily life (What-Skills). Exemplary mindfulness exercises were short breathing-meditations, body scans, or mindful body movements.
In module (a) health-promoting self-care, supervisors received information on the stress-process and their current stressors and strains were identified using Pennebaker’s expressive writing technique (Pennebaker & Chung, 2007). They learned how they can use mindfulness skills to control their attention, be aware of their own thoughts, emotions, and bodily sensations, and recognize their own stressors and limits. To select and use suitable coping strategies, the participants learned to distinguish between changeable and unchangeable stressors. The participants practiced acceptance-based techniques based on mindfulness to address unchangeable stressors. Changeable stressors were addressed by means of an evidence-based problem-solving technique to foster active coping. In addition, the participants learned how to use mindfulness skills to effectively recover from work and to develop and plan regenerative activities (e.g., physical activity).
In module (b) health-promoting staff care, supervisors were sensitized to the importance of health for the efficacy and satisfaction of working teams and educated about basic psychological needs (Grawe, 2004). Mindfulness exercises were deepened and the ways in which mindfulness can contribute to health-promoting staff care were discussed. Supervisors learned how they can improve healthy working conditions and promote a cooperative team climate (organizational leadership). On the level of personal leadership, the participants determined how they could specifically address the individual needs and competencies of their employees, e.g., by formulating specific tasks. Finally, appreciation, as a central leadership element, was trained with numerous communication role-playing exercises.
In module (c) addressing employees under stress, mindfulness practice was further deepened and the possibilities and limits of leadership were discussed. In order to reduce uncertainties, participants were familiarized with the development and symptoms of stress-related mental illnesses and their recognition by means of case studies. Using a guide that supervisors can apply in response to observed stress, supervisors learned how to address mental distress in communication settings and practiced this in role plays. Further conversation settings such as regular check-ins, return interviews, and operational reintegration discussions were discussed.
The two 3-hr booster sessions aimed to enhance the sustainability of the intervention and to support participants in implementing the intervention content to their daily lives. The two 3-hr booster sessions were divided into three parts: a reflection on the implementation of the goals, an analysis of the unimplemented goals with a focus on barriers, and planning the next steps.
All modules were delivered at intervals of 4 weeks. Courses were led by health coaches and psychologists from the health insurance company, who had at least 5 years of experience in delivering preventive health interventions and received several days of training and continuous supervision. The total training time was 30 hr over a period of 6 months. A more detailed description of the intervention can be found in Vonderlin et al. (2021).
Measures
All data were selected from routine health-insurance statistics. For data protection reasons, all analyses were conducted independently of the psychometric assessments in the evaluation study; i.e., questionnaire and work disability data were not merged.
Sociodemographic Data
Data on age, gender, education, insurance type, branch of employer, and degree of work complexity (which describes the need for specialized knowledge, degree of decision latitude and responsibility, and ranges from apprenticeship activities to highly complex jobs) were selected from the routine health insurance data.
Sickness Absence Days
Nonspecific (due to any disorder) and specific sick days (due to a mental disorder) were selected from the routine health insurance data for all study participants as follows: For the recording of specific sick days, the sick days of the main diagnostic group “mental and behavioral disorders” (ICD 10, F00-F99) and “problems related to difficulties in coping with life” (Z73, including accentuation of personality traits, being burnt out, burnout) were selected. Nonspecific sick days represent all sick days due to any diagnosis according to ICD 10 (also including the specific sick days selected in this study). The cumulated sick days 2 years before the intervention (pre) and 2 years after the intervention (post) were used to investigate potential intervention effects in the IG. In the CG, the date of giving consent was used to separate the two time periods.
Data Analyses
Many individuals do not generate any single sick days. Therefore, sick day data are usually not normally distributed but represent a probability distribution, with a positive mass at 0 (discrete distribution) and a continuous distribution above 0. This type of distribution is called a compound Poisson-gamma distribution, which belongs to the broader statistical family of Tweedie distributions that describe semi-continuous data with a positive mass at 0 (Hasan & Dunn, 2011). This type of distribution can be modeled in generalized linear models and has been shown to be a good fit healthcare cost data, which are typically non-negative, right-skewed, and have excess zeros for non-users or people with no sick days (Kurz, 2017). After examining the distribution of sick day data visually, we decided to conduct a generalized linear model with Tweedie log-link function to analyze the nonspecific and specific sick days as the dependent variable. Sickness absence days post-intervention (up to 24 months after the intervention starts) were adjusted for sickness absence days prior to the intervention (24 months before the start of the intervention). As control variables, gender, age, and branch were included. Education was not included in the model because it would have resulted in high dropout of participants in the intervention group due to missing data (Table 1). Instead, we decided to enter the covariate complexity of work into the model, as it was significantly correlated with school education (r = 0.36, p < 0.001). Because of the small sample size in the intervention group and the high heterogeneity in sick day data, we performed sensitivity analyses in addition to the statistical model. In doing so, we first calculated descriptive mean scores, analyzed them visually, and used a bootstrapping t-test (5000 samples) to compare post-intervention scores between groups. In addition, we calculated pre–post median scores in each group, which are more robust to outliers. To handle outliers, we decided to conduct robust sensitivity analyses and to not exclude them, since there was no evidence that outliers were caused by systematic error. All analyses were performed using SPSS 26.0.
Results
The sample of 1830 study participants consisted of 78% women and averaged 43.5 years of age (SD = 12.1). The percentage of participants holding an A-Level degree (13 years of school education) was 34.3%, whereas only 0.1% had no school-leaving certificate. Most participants (88%) worked in the healthcare sector (e.g., hospitals, nursing homes). Socio-demographics of the sample are depicted in Table 1.
For nonspecific sick days at post-intervention, supervisors in the MBP had a significantly lower number of sick days than their matched controls (χ2[1] = 4.38, p = 0.036, d = 0.47). On average, supervisors in the MBP showed an adjusted M = 13.9 (SE = 5.64) nonspecific sickness absence days in the 2 years after the intervention, whereas participants in the control group showed an adjusted M = 32.9 (SE = 2.46) nonspecific absence days during this time period. At the employee level, no significant differences were obtained between participants in the experimental and control groups (χ2[1] = 0.45, p = 0.50, d= –0.28). On average, employees in the experimental group showed an adjusted M = 33.6 (SE = 2.78) nonspecific sickness absence days in the 2 years after the intervention, whereas participants in the control group showed an adjusted M = 31.6 (SE = 1.04) nonspecific absence days during this time period (see Table 2, Table 3, and Fig. 2).
Adjusted nonspecific (left) and specific (right) sick days 2 years after the intervention in the intervention (IG) and control (CG) groups on the supervisor and employee levels. *p < 0.05. Error bars represent standard errors. Adjusted model controlled for the covariates age, gender, work complexity, branches and (non) specific sick days 2 years before the intervention (pre). Covariates included in this model: age, gender, work-complexity, branch, absence days (pre-intervention)
For specific sick days (due to mental illness) at post-intervention, no significant between-group effects were found on the supervisor and employee levels. Whereas supervisors in the MBP group showed an average of M = 5.6 (SE = 6.81) specific sickness absence days, supervisors in the control group showed a similar amount of M = 5.2 (SE = 1.38) specific sickness absence days in the 2-year period after the intervention. On the employee level, employees in the experimental group showed an average of M = 8.9 (SE = 1.20) specific sickness absence days, and employees in the control group showed an average of M = 8.12 (SE = 0.71) specific sickness absence days in the 2-year period after the intervention (see Table 2, Table 3, and Fig. 2).
Regarding our control variables assessed, we found a significant effect of age on employees’ non-specific sick-days (ß = 0.015, p < 0.001) with a larger number of sick days for older employees. There was no significant effect of age on other sick-day outcomes. Gender showed a significant effect on supervisors’ non-specific sick days (ß = 0.348, p < 0.033) with a larger number of sick days for female supervisors. There was no significant effect of gender on other sick day outcomes. Work complexity showed a significant effect on employees’ non-specific sick days (ß = –0.129, p < 0.001) with lower complexity showing a larger number of sick days. Supervisors’ work complexity showed a significant effect on their specific sick days (ß = 0.688, p = 0.002) with a higher work complexity associated with a larger number of specific sick days. Working branch showed a significant effect on employees non-specific and specific sick days (non-specific: ß = 0.437, p < 0.001; specific: ß = 0.673, p < 0.001) with a larger number of sick days for employees working in the healthcare sector.
Due to the low sample size of supervisors in the IG (n = 13), we conducted sensitivity analyses to explore the nature of the significant between-group effect in our generalized linear model on supervisors’ nonspecific sick days. The descriptive mean scores showed a decrease in values from 27.77 (SD = 76.11) to 17.54 (SD = 28.45) sick days in the intervention group, as well as an increase in values from 29.06 (SD = 59.94) to 38.90 (SD = 78.30) sick days in the control group. Raw data of participants are depicted in Fig. 3. The bootstrapping t-test remained significant, with a mean difference of 21.36 sick days (SE = 9.11, p = 0.027). However, visual inspection of the plot revealed that the decrease in sick days in the intervention group was mainly affected by one outlying case with a decrease of 215 sick days. Therefore, we calculated median scores, which are more robust to outliers. Median scores in the IG showed a slight increase in values, from 6.33 to 7.00 sick days, whereas median scores in the CG showed a stronger increase in values, from 8.84 to 11.40 sick days. Thus, the incremental increase of the median sick days was 1.93 sick days higher in the CG compared to the IG.
Discussion
In this study, we examined the effect of a workplace MBP for supervisors on their sick days. We also examined a possible effect of the intervention on employees’ sick days at work, although they did not participate actively in the program. Results showed that supervisors in the MBP program had significantly fewer nonspecific absence days in the 2 years after the intervention compared to their matched controls. Sensitivity analyses revealed that this effect was mainly driven by an increase in sick days in the control group. In addition, this effect did not reflect on specific absence days due to mental illness. No intervention effects were detected on the employee level.
Our results indicate that the effects of our MBP showing significant improvements of supervisors’ health-oriented self-care and mental health were also reflected in more objective measures like their sickness absence days (see Vonderlin et al., 2021). This is in line with previous findings, showing significant effects of an MBP on the supervisors’ subjectively perceived stress levels as well as their sick days (Żołnierczyk-Zreda et al., 2016). These results indicate that MBPs do not only reduce individual suffering of individuals but also might have (financial) benefits for organizations and the societal health system. Whereas supervisors in the control group showed an average of 33 sick days in the 2-year period after the intervention, supervisors in the MBP group showed only 14 sick days during this period. When taking into account the average costs due to production loss in 2014 of 105 EUR per sick day in Germany, our results indicate that an organization could save 1995 EUR per participant in 2 years when offering MBPs for their supervisors (German Federal Institute for Occupational Safety and Health [Bundesanstalt für Arbeitsschutz und Arbeitsmedizin], 2014).
However, considering that the costs of supervisors’ sick days tend to be above average, the amount of money that could be saved could be even higher. In addition, our analyses focus on the official sick days recorded by the participants’ health insurers. On the one hand, this assessment has advantages because it is carried out by general practitioners, making it more objective than assessments by organizations. On the other hand, we are probably underestimating the considerable number of unreported sick days, since in Germany a medical sickness certificate is required and recorded by the health insurance providers only after three consecutive days of sickness. Thus, we might probably still underestimate the beneficial cost effects in our analyses. Last but not least, our results reflect only the costs due to sickness-related absenteeism. Presenteeism, which refers to attending work while ill, has been estimated to produce four times as many costs compared to being absent from work (Goetzel et al., 2004; Johns, 2010; Schmid et al., 2017). Taking this into account, offering MBPs for the workforce could be good value for money for organizations.
Due to the low sample size in our intervention group of n = 13 supervisors, we conducted sensitivity analyses to explore the significant between-group effect on supervisors’ sick days in more detail. A visual inspection of data showed that the decrease of sick days in the intervention group was mainly affected by one outlying case. Nevertheless, we decided not to completely remove the outliers from our analyses and to perform our main analyses based on generalized linear models with Tweedie distribution and log-link function, as these take into account the specific distribution of sick days, which are not normally distributed but follow a Tweedie distribution. Instead, we additionally analyzed median scores to compare both groups as sensitivity analysis because median scores are more robust to outliers. Median scores showed that the effect was mainly driven by an increase of sick days in the control group, whereas sick days in the IG remained stable. The median increase of sick days in the control group was 1.93 days higher compared to the IG. This increase of sick days in the control group is in line with current epidemiological data from Germany, showing a steady increase of nonspecific sick days in the last decade of 10.2% from 2010 to 2020 (Meyer et al., 2021). This raises the question of whether a stabilization of sick days in times of increased psychological distress in the modern world of work can also be seen as an intervention effect. Future studies addressing this question should replicate our findings by assessing sick days in larger and representative samples and longer time periods.
Interestingly, our results showed intervention effects only on nonspecific sick days of supervisors but not on specific sick days due to mental disorders. At first glance, this seems counterintuitive, since MBPs primarily address psychological outcomes. However, there is also a somatic experience of increased mental distress, and it might be that early mental distress in primary care might be first described by somatic symptoms like headache, tension, or back pain and not diagnosed as a mental disorder (e.g., Toft et al., 2005). This also points to the importance of community-based promotion programs for mental health that raise awareness about the prevalence of mental health problems (World Health Organization, 2002).
In addition to the intervention effects on supervisor level, our covariates in the model included to control for important confounding variables showed a significant effect of supervisor gender (higher nonspecific sick days for women) and a significant effect of work complexity (higher specific sick days for supervisors with highly complex tasks) on supervisor sick days. This is consistent with epidemiological data from Germany, which show a slightly higher sick leave rate for women (5.5%) than for men (5.3%; Meyer et al., 2022). These results may indicate which vulnerable groups could benefit most from MBPs. Nevertheless, further research is urgently needed to investigate the reasons for these gender differences in sick days. For example, gender inequalities in the labor market have been shown to influence absenteeism and presenteeism rates across 26 OECD countries (Kwon, 2020). This may explain our finding that gender significantly affects sick days at the supervisor level but not at the employee level, as leadership roles are still often associated with male stereotypes, which may lead to prejudice against female leaders (Eagly & Karau, 2002). Future research should shed light on these processes to overcome stereotypes in leadership, promote gender equality, and prepare the ground for potential change (Eagly & Karau, 2002).
Our results show that no significant effects of the supervisors’ MBP were obtained on the employee level. This is in line with results from the psychometric analyses, in which no significant indirect effects from our leadership intervention emerged on the employees’ mental health (Vonderlin et al., 2021). To our knowledge, this is one of the first studies investigating the effects of an MBP for supervisors on their employees’ sick days. Previous studies on leadership interventions showed a (marginally) significant effect on employees’ sick days; however, these interventions were not mindfulness-based (Dannheim et al., 2022; Stansfeld et al., 2015). Therefore, our results add important empirical evidence on whether effects at the employee level can be obtained through mindfulness-based interventions.
Several factors should be taken into account to explain these non-significant results, which also provide an indication of how interventions and research designs could be improved in future research to investigate such indirect effects. First, the intervention was designed so that only supervisors attended the sessions; i.e., employees did not participate in the intervention. Future research should develop and investigate team interventions or content-related interventions for supervisors and their staff (e.g., Ward et al., 2018). At a minimum, however, supervisors should be encouraged to establish mindfulness-based approaches in their team as well (e.g., short mindfulness exercises at the beginning of each team meeting) in order to integrate the content of the training into employees’ daily lives also. Data assessments should not only collect health-related variables of the employees, but also assess concrete measures that supervisors implement in everyday life as well as the employees’ perception of these concrete measures (e.g., mindfulness practices, addressing mental distress issues). In addition, moderator and mediator analyses should be used to investigate the process of when and how MBPs affect sick days in more detail to gain a better understanding of this process.
In addition to the intervention effects on employee level, our covariates in the model included to control for important confounding variables showed a significant effect of employee age (higher nonspecific sick days among older employees), a significant effect of work complexity (higher nonspecific sick days among employees with less complex tasks), and a significant effect of working branch on employee nonspecific and specific sick days (higher sick days in the healthcare sector). This is consistent with epidemiological data in Germany, which show an overall sickness rate of 6.2% in the healthcare sector, which is higher than average compared to other industries (5.4%), as well as a clear increase in sick days with increasing age (Meyer et al., 2022). These findings may indicate which vulnerable groups could benefit most from MBPs. However, it is important to note that we are not able to draw conclusions about possible differential effects for different groups of people based on our results. Future research should address this question in order to target MBPs in the workplace (e.g., Krick & Felfe, 2020).
Previous research has critically discussed whether mindfulness-based programs should be judged regarding their cost-effectiveness at workplaces, since this seems to contradict the original nature of mindfulness as being undirected and not aiming to increase productivity (e.g., Segall, 2021). However, empirical evidence on its cost-effectiveness is important to ensure a large-scale implementation in organizations, especially those with moderate financial resources like the healthcare system or other non-profit organizations (Doyle et al., 2019).
Limitations and Future Research
This research has far-reaching implications. Our findings support that MBPs at the workplace not only affect subjectively assessed health-related outcomes, but they also reflect on supervisors’ sick days. This might result in (financial) benefits for organizations and the healthcare system. These results could contribute to further expanding the range of MBPs in promoting mental health in the work context and provide important information for organizations thinking about implementing MBPs for their workforce. The major strength of our study relates to its longitudinal and multilevel intervention design by also including objective health data like sickness absence days to investigate the effectiveness of the program. However, there are some limitations that should be taken into account when interpreting the results.
First, our intervention is not only a pure mindfulness intervention but also includes other elements based on behavioral change and psychoeducation. Thus, a causal interpretation regarding the mechanism of change is not possible. In addition to mindfulness training, other intervention elements may have contributed to the impact on sick days, particularly from the self-care module (e.g., improved problem-solving skills). However, all courses were based on mindfulness practice as the major conceptual framework, and this reflects the naturally occurring heterogeneity of mindfulness-based intervention in workplaces (Vonderlin et al., 2020). Interestingly, the results of the psychometric analyses showed that the effect of the intervention on supervisors’ mental health was moderated by the extent of their mindfulness practice at home (Vonderlin et al., 2021). Thus, we hypothesize that mindfulness training is at least one important mechanism that leads to improved health and, in turn, affects sick days. However, future studies should attempt to replicate our findings with pure mindfulness interventions to shed more light on the processes involved.
Second, due to data protection issues, we were not able to merge the data on sick days with questionnaire data from the evaluation study (Vonderlin et al., 2021). Therefore, we were not able to examine possible mechanisms of change in more detail. The results of the psychometric evaluation of the intervention suggest that the impact of the intervention on supervisors’ mental health was mediated by an improvement in their health-oriented self-care (Vonderlin et al., 2021). We therefore assume that this increased self-care and improvement in their mental health is also the process by which the intervention may have affected sick days. However, it would have been interesting to explore this assumption further and demonstrate whether a decrease in sick days also translates into increased mindfulness and self-care or decreased subjectively perceived psychological distress among supervisors.
Third, assignment to the groups was not randomized, and the control group was a passive control cohort recruited outside the organizations. This could have led to systematic biases between groups (e.g., due to organizational culture). To address this limitation, we used propensity score matching to control for key confounding variables (e.g., age, gender). However, future research should replicate our findings using randomized controlled trials and active control cohorts.
Fourth, our final sample size was smaller than planned in the a priori power analyses, reducing the power to detect significant changes. Especially on the supervisor level in the intervention group, the sample size with n = 13 supervisors was lower than the aimed sample size of 99 supervisors. The reduced sample size is for two major reasons. First, we could only evaluate data from the cooperating health insurance company. Therefore, we had to exclude participants who were covered by other health insurers. Second, only five of the 12 organizations participating in the study gave their informed consent to analyze their sickness absence data. This could be due to the fact that at the time the study was conducted, new data protection regulations were coming into force in Europe, causing uncertainty among the organizations’ executive boards and works councils. To address this limitation and to reduce the risk of systematic biases, we conducted sensitivity analyses to describe the significant between-group effect on supervisors’ nonspecific sick days in detail. However, our findings should be interpreted with caution, and future research is urgently needed to replicate our results with larger sample sizes.
Finally, our results on decreased sick days give a first indication of possible financial benefits for organizations. However, our analysis does not represent a full cost-effectiveness analysis. This would also require analyzing the costs associated with implementing the intervention, which were not available in this study. However, Doyle et al. (2019) estimated average costs of US$515 and $1217 per participant to implement an MBP, which is lower than our estimated potential benefit of EUR 1995 per participant over 2 years.
Against the background of the current COVID-19 pandemic, this study points out several implications. It is important to note that the intervention was conducted before the onset of the spread of COVID-19 in Germany. However, the recording of sick days after the intervention (2 years after the intervention until 02/2021) showed an overlap with the onset of the COVID pandemic in Germany (02/2020). Although data from Germany show that sick days remained stable during the pandemic (2019: 10.9 days per employee, 2020: 11.2 days per employee, 2021: 11.2 days per employee; German Federal Statistical Office [Statistisches Bundesamt], 2023), this indicates the importance of our control group to account for potential systematic bias due to COVID. Nevertheless, practitioners and researchers agree that the COVID-19 pandemic represents a profound crisis in workplace health, and the resulting stressors will continue to affect mental health in the workplace (Shoss, 2021). Thus, it will continue to be a major challenge for supervisors to manage COVID-specific stressors and strains on their employees (e.g., telecommunications and loneliness; Andel et al., 2021). Previous research has shown that MBPs can help buffer COVID-related psychological stress (Al Ozairi et al., 2023; Bossi et al., 2022). The present study adds to these findings by suggesting that a mindfulness- and skill-based program for supervisors could help improve their health and stabilize their nonspecific sick days at work. Given that the COVID-19 pandemic is estimated by most to be one of many crises that society will face in the near future (Boin, 2019) and the central role of supervisors in managing workplace crises (Klebe et al., 2021), our study suggests that mindfulness-based interventions for supervisors could help stabilize sick days during times of increased psychological stress.
In conclusion, our data show that our mindfulness-based leadership intervention not only was effective in reducing mental distress among supervisors but also showed significant effects on their sickness absences. Sensitivity analyses showed that this effect was mainly driven by stabilization of supervisors’ sick days in the MBP group compared to an increase of sick days in the control group. In addition to reducing individual suffering, this can also have (financial) benefits for organizations and society. Overall, these findings could make an important contribution to the large-scale implementation of MBPs in the work context and inform decision makers in organizations that are considering implementing MBPs for their workforce.
Data Availability
The raw data supporting the conclusions of this article will be made available by the authors, upon request.
References
Almroth, M., Hemmingsson, T., Sörberg Wallin, A., Kjellberg, K., Burström, B., & Falkstedt, D. (2022). Psychosocial working conditions and the risk of diagnosed depression: a Swedish register-based study. Psychological Medicine, 25(15), 3730–3738. https://doi.org/10.1017/s003329172100060x
Al Ozairi, A., Alsaeed, D., Al-Ozairi, E., Irshad, M., Crane, R. S., & Almoula, A. (2023). Effectiveness of virtual mindfulness-based interventions on perceived anxiety and depression of physicians during the COVID-19 pandemic: a pre-post experimental study. Frontiers in Psychiatry, 13, 1089147. https://doi.org/10.3389/fpsyt.2022.1089147
Andel, S. A., Shen, W., & Arvan, M. L. (2021). Depending on your own kindness: the moderating role of self-compassion on the within-person consequences of work loneliness during the COVID-19 pandemic. Journal of Occupational Health Psychology, 26(4), 276–290. https://doi.org/10.1037/ocp0000271
Anderson, N. (2021). An evaluation of a mindfulness-based stress reduction intervention for critical care nursing staff: a quality improvement project. Nursing in Critical Care, 26(6), 441–448. https://doi.org/10.1111/nicc.12552
Arendt, J. F. W., Pircher Verdorfer, A., & Kugler, K. G. (2019). Mindfulness and leadership: communication as a behavioral correlate of leader mindfulness and its effect on follower satisfaction. Frontiers in Psychology, 10, 667. https://doi.org/10.3389/fpsyg.2019.00667
Austin, P. C. (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46(3), 399–424. https://doi.org/10.1080/00273171.2011.568786
Baer, R. A. (2015). Mindfulness-based treatment approaches: clinician's guide to evidence base and applications. Elsevier.
Baron, L., Rouleau, V., Grégoire, S., & Baron, C. (2018). Mindfulness and leadership flexibility. Journal of Management Development, 37(2), 165–177. https://doi.org/10.1108/JMD-06-2017-0213
Bartlett, L., Martin, A., Neil, A. L., Memish, K., Otahal, P., Kilpatrick, M., & Sanderson, K. (2019). A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. Journal of Occupational Health Psychology, 24(1), 108–126. https://doi.org/10.1037/ocp0000146
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: a proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. https://doi.org/10.1093/clipsy.bph077
Bloom, D. E., Cafiero, E. T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L. R., Fathima, S., Feigl, A. B., Gaziano, T., Mowafi, M., Pandya, A., Prettner, K., Rosenberg, L., Seligman, B., Stein, A. Z., & Weinstein, C. (2011). The global economic burden of noncommunicable diseases. World Economic Forum Geneva. http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf
Boin, A. (2019). The transboundary crisis: why we are unprepared and the road ahead. Journal of Contingencies and Crisis Management, 27(1), 94–99. https://doi.org/10.1111/1468-5973.12241
Bono, J. E., Glomb, T. M., Shen, W., Kim, E., & Koch, A. (2013). Building positive resources: effects of positive events and positive reflection on work stress and health. Academy of Management Journal, 56(6), 1601–1627. https://doi.org/10.5465/AMJ.2011.0272
Bossi, F., Zaninotto, F., D’Arcangelo, S., Lattanzi, N., Malizia, A. P., & Ricciardi, E. (2022). Mindfulness-based online intervention increases well-being and decreases stress after COVID-19 lockdown. Scientific Reports, 12, 6483. https://doi.org/10.1038/s41598-022-10361-2
Chin, B., Slutsky, J., Raye, J., & Creswell, J. D. (2019). Mindfulness training reduces stress at work: a randomized controlled trial. Mindfulness, 10(4), 627–638. https://doi.org/10.1007/s12671-018-1022-0
Dannheim, I., Ludwig-Walz, H., Buyken, A. E., Grimm, V., & Kroke, A. (2022). Effectiveness of health-oriented leadership interventions for improving health and wellbeing of employees: a systematic review. Journal of Public Health, 30, 2777–2789. https://doi.org/10.1007/s10389-021-01664-1
Darr, W., & Johns, G. (2008). Work strain, health, and absenteeism: a meta-analysis. Journal of Occupational Health Psychology, 13(4), 293–318. https://doi.org/10.1037/a0012639
Demerouti, E., Nachreiner, F., Bakker, A. B., & Schaufeli, W. B. (2001). The job demands-resources model of burnout. Journal of Applied Psychology, 86(3), 499–512. https://doi.org/10.1037/0021-9010.86.3.499
Donaldson-Feilder, E., Lewis, R., & Yarker, J. (2019). What outcomes have mindfulness and meditation interventions for managers and leaders achieved? A systematic review. European Journal of Work and Organizational Psychology, 28(1), 11–29. https://doi.org/10.1080/1359432X.2018.1542379
Doyle, S. L., Brown, J. L., Rasheed, D., Jones, D. E., & Jennings, P. A. (2019). Cost analysis of ingredients for successful implementation of a mindfulness-based professional development program for teachers. Mindfulness, 10(1), 122–130. https://doi.org/10.1007/s12671-018-0958-4
Eagly, A. H., & Karau, S. J. (2002). Role congruity theory of prejudice toward female leaders. Psychological Review, 109(3), 573–598. https://doi.org/10.1037/0033-295X.109.3.573
Eaton, J., Qureshi, O., Salaria, N., & Ryan, G. (2018). The Lancet Commission on Mental Health and Sustainable Development: evidence for action on mental health and global development. London School of Hygiene and Tropical Medicine. https://www.mhinnovation.net/sites/default/files/downloads/resource/Lancet%20Commission_policy%20brief_MHIN2.v3.pdf
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
Ford, M. T., Cerasoli, C. P., Higgins, J. A., & Decesare, A. L. (2011). Relationships between psychological, physical, and behavioural health and work performance: a review and meta-analysis. Work & Stress, 25(3), 185–204. https://doi.org/10.1080/02678373.2011.609035
Franke, F., Felfe, J., & Pundt, A. (2014). The impact of health-oriented leadership on follower health: development and test of a new instrument measuring health-promoting leadership. German Journal of Human Resource Management, 28(2), 139–161. https://doi.org/10.1177/239700221402800108
German Federal Institute for Occupational Safety and Health [Bundesanstalt für Arbeitsschutz und Arbeitsmedizin]. (2014). Sicherheit und Gesundheit bei der Arbeit 2014: Unfallverhütungsbericht Arbeit [Safety and health at work 2014: Accident prevention report on work]. Druck & Verlag Kettler. https://www.baua.de/DE/Angebote/Publikationen/Berichte/Suga-2014.pdf?__blob=publicationFile&v=17
German Federal Statistical Office [Statistisches Bundesamt] (2023). Quality of work: sickness rate [Qualität der Arbeit: Krankenstand]. https://www.destatis.de/DE/Themen/Arbeit/Arbeitsmarkt/Qualitaet-Arbeit/Dimension-2/krankenstand.html
Grawe, K. (2004). Psychological therapy. Hogrefe Publishing.
Goetzel, R. Z., Long, S. R., Ozminkowski, R. J., Hawkins, K., Wang, S., & Lynch, W. (2004). Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. Journal of Occupational and Environmental Medicine, 46(4), 398–412. https://doi.org/10.1097/01.jom.0000121151.40413.bd
Hasan, M. M., & Dunn, P. K. (2011). Two tweedie distributions that are near-optimal for modelling monthly rainfall in Australia. International Journal of Climatology, 31(9), 1389–1397. https://doi.org/10.1002/joc.2162
Hassard, J., Teoh, K. R. H., Visockaite, G., Dewe, P., & Cox, T. (2018). The cost of work-related stress to society: a systematic review. Journal of Occupational Health Psychology, 23(1), 1–17. https://doi.org/10.1037/ocp0000069
Hülsheger, U. R., Feinholdt, A., & Nübold, A. (2015). A low-dose mindfulness intervention and recovery from work: effects on psychological detachment, sleep quality, and sleep duration. Journal of Occupational and Organizational Psychology, 88(3), 464–489. https://doi.org/10.1111/joop.12115
Inceoglu, I., Arnold, K. A., Leroy, H., Lang, J. W. B., & Stephan, U. (2021). From microscopic to macroscopic perspectives and back: the study of leadership and health/well-being. Journal of Occupational Health Psychology, 26(6), 459–468. https://doi.org/10.1037/ocp0000316
Jacobs, S. J., & Blustein, D. L. (2008). Mindfulness as a coping mechanism for employment uncertainty. The Career Development Quarterly, 57(2), 174–180. https://doi.org/10.1002/j.2161-0045.2008.tb00045.x
Jamieson, S. D., & Tuckey, M. R. (2017). Mindfulness interventions in the workplace: a critique of the current state of the literature. Journal of Occupational Health Psychology, 22(2), 180–193. https://doi.org/10.1037/ocp0000048
Johns, G. (2010). Presenteeism in the workplace: a review and research agenda. Journal of Organizational Behavior, 31(4), 519–542. https://doi.org/10.1002/job.630
Kelloway, E. K., & Barling, J. (2010). Leadership development as an intervention in occupational health psychology. Work & Stress, 24(3), 260–279. https://doi.org/10.1080/02678373.2010.518441
Klebe, L., Felfe, J., & Klug, K. (2021). Healthy leadership in turbulent times: the effectiveness of health-oriented leadership in crisis. British Journal of Management, 32(4), 1203–1218. https://doi.org/10.1111/1467-8551.12498
Kranabetter, C., & Niessen, C. (2017). Managers as role models for health: moderators of the relationship of transformational leadership with employee exhaustion and cynicism. Journal of Occupational Health Psychology, 22(4), 492–502. https://doi.org/10.1037/ocp0000044
Krick, A., & Felfe, J. (2020). Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. Journal of Occupational Health Psychology, 25(2), 99–112. https://doi.org/10.1037/ocp0000159
Kurz, C. F. (2017). Tweedie distributions for fitting semicontinuous health care utilization cost data. BMC Medical Research Methodology, 17, 171. https://doi.org/10.1186/s12874-017-0445-y
Kwon, M. J. (2020). Occupational health inequalities by issues on gender and social class in labor market: absenteeism and presenteeism across 26 OECD countries. Frontiers in Public Health, 8, 84. https://doi.org/10.3389/fpubh.2020.00084
Levett, K. M., Coughlan, S., Longridge, S., Roumeliotis, V., & Adams, J. (2019). Be well: a systems-based wellness intervention using mindfulness in the workplace – a case study. Journal of Management & Organization, 25(5), 613–634. https://doi.org/10.1017/jmo.2017.41
Linehan, M. M. (2014). DBT? Skills training manual. Guilford Publication.
Lomas, T., Medina, J. C., Ivtzan, I., Rupprecht, S., & Eiroa-Orosa, F. J. (2019). Mindfulness-based interventions in the workplace: an inclusive systematic review and meta-analysis of their impact upon wellbeing. The Journal of Positive Psychology, 14(5), 625–640. https://doi.org/10.1080/17439760.2018.1519588
Lothes, J., Mochrie, K., Wilson, M., & Hakan, R. (2021). The effect of DBT-informed mindfulness skills (what and how skills) and mindfulness-based stress reduction practices on test anxiety in college students: a mixed design study. Current Psychology, 40(6), 2764–2777. https://doi.org/10.1007/s12144-019-00207-y
Lyssenko, L., Müller, G., Kleindienst, N., Schmahl, C., Berger, M., Eifert, G., Kölle, A., Nesch, S., Ommer-Hohl, J., Wenner, M., & Bohus, M. (2015). Life balance – a mindfulness-based mental health promotion program: conceptualization, implementation, compliance and user satisfaction in a field setting. BMC Public Health, 15(1), 740. https://doi.org/10.1186/s12889-015-2100-z
Meyer, M., Wing, L., Schenkel, A., & Meschede, M. (2021). Krankheitsbedingte Fehlzeiten in der deutschen Wirtschaft im Jahr 2020 [Sickness-related absenteeism in the German economy in 2020]. In B. Badura, A. Ducki, M. Meyer, & H. Schröder (Eds.), Fehlzeiten-Report 2021 [Absenteeism Report 2021] (pp. 441–539). Springer.
Meyer, M., Wing, L., Schenkel, A., & Meschede, M. (2022). Krankheitsbedingte Fehlzeiten in der deutschen Wirtschaft im Jahr 2021 [Sickness-related absenteeism in the German economy in 2021]. In B. Badura, A. Ducki, M. Meyer, & H. Schröder (Eds.), Fehlzeiten-Report 2022 [Absenteeism Report 2022] (pp. 289–368). Springer.
Milligan-Saville, J. S., Tan, L., Gayed, A., Barnes, C., Madan, I., Dobson, M., Bryant, R. A., Christensen, H., Mykletun, A., & Harvey, S. B. (2017). Workplace mental health training for managers and its effect on sick leave in employees: a cluster randomised controlled trial. The Lancet Psychiatry, 4(11), 850–858. https://doi.org/10.1016/S2215-0366(17)30372-3
Montano, D., Reeske, A., Franke, F., & Hüffmeier, J. (2017). Leadership, followers' mental health and job performance in organizations: a comprehensive meta-analysis from an occupational health perspective. Journal of Organizational Behavior, 38(3), 327–350. https://doi.org/10.1002/job.2124
Müller, G., Bombana, M., Heinzel-Gutenbrenner, M., Kleindienst, N., Bohus, M., Lyssenko, L., & Vonderlin, R. (2021). Socio-economic consequences of mental distress: quantifying the impact of self-reported mental distress on the days of incapacity to work and medical costs in a two-year period: a longitudinal study in Germany. BMC Public Health, 21(1), 625. https://doi.org/10.1186/s12889-021-10637-8
Netterstrøm, B., Friebel, L., & Ladegaard, Y. (2013). Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: results from a randomised, wait-list controlled trial. Psychotherapy and Psychosomatics, 82(3), 177–186. https://doi.org/10.1159/000346369
Nübold, A., Van Quaquebeke, N., & Hülsheger, U. R. (2020). Be(com)ing real: a multi-source and an intervention study on mindfulness and authentic leadership. Journal of Business and Psychology, 35(4), 469–488. https://doi.org/10.1007/s10869-019-09633-y
Ostafin, B. D., & Kassman, K. T. (2012). Stepping out of history: mindfulness improves insight problem solving. Consciousness and Cognition, 21(2), 1031–1036. https://doi.org/10.1016/j.concog.2012.02.014
Pennebaker, J. W., & Chung, C. K. (2007). Expressive writing, emotional upheavals, and health. In H. S. Friedman & R. C. Silver (Eds.), Foundations of health psychology (pp. 263–284). Oxford University Press.
Pinck, A. S., & Sonnentag, S. (2018). Leader mindfulness and employee well-being: the mediating role of transformational leadership. Mindfulness, 9, 884–896. https://doi.org/10.1007/s12671-017-0828-5
Reb, J., Narayanan, J., & Chaturvedi, S. (2014). Leading mindfully: two studies on the influence of supervisor trait mindfulness on employee well-being and performance. Mindfulness, 5, 36–45. https://doi.org/10.1007/s12671-012-0144-z
Roche, M., Haar, J. M., & Luthans, F. (2014). The role of mindfulness and psychological capital on the well-being of leaders. Journal of Occupational Health Psychology, 19(4), 476–489. https://doi.org/10.1037/a0037183
Roeser, R. W., Schonert-Reichl, K. A., Jha, A., Cullen, M., Wallace, L., Wilensky, R., Oberle, E., Thomson, K., Taylor, C., & Harrison, J. (2013). Mindfulness training and reductions in teacher stress and burnout: results from two randomized, waitlist-control field trials. Journal of Educational Psychology, 105(3), 787–804. https://doi.org/10.1037/a0032093
Schmidt, B., Schneider, M., Seeger, P., van Vianen, A., Loerbroks, A., & Herr, R. M. (2019). A comparison of job stress models: associations with employee well-being, absenteeism, presenteeism, and resulting costs. Journal of Occupational and Environmental Medicine, 61(7), 535–544. https://doi.org/10.1097/jom.0000000000001582
Schmid, J. A., Jarczok, M. N., Sonntag, D., Herr, R. M., Fischer, J. E., & Schmidt, B. (2017). Associations between supportive leadership behavior and the costs of absenteeism and presenteeism: an epidemiological and economic approach. Journal of Occupational and Environmental Medicine, 59(2), 141–147. https://doi.org/10.1097/jom.0000000000000919
Segall, S. Z. (2021). Mindfulness in and out of the context of western Buddhist modernism. The Humanistic Psychologist, 49(1), 40–55. https://doi.org/10.1037/hum0000159
Shoss, M. (2021). Occupational health psychology research and the COVID-19 pandemic. Journal of Occupational Health Psychology, 26(4), 259–260. https://doi.org/10.1037/ocp0000292
Stansfeld, S. A., Kerry, S., Chandola, T., Russell, J., Berney, L., Hounsome, N., Lanz, D., Costelloe, C., Smuk, M., & Bhui, K. (2015). Pilot study of a cluster randomised trial of a guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: GEM Study. BMJ Open, 5, e007981. https://doi.org/10.1136/bmjopen-2015-007981
Stedham, Y., & Skaar, T. B. (2019). Mindfulness, trust, and leader effectiveness: a conceptual framework. Frontiers in Psychology, 10, 1588. https://doi.org/10.3389/fpsyg.2019.01588
Toft, T., Fink, P. E. R., Oernboel, E. V. A., Christensen, K. A. J., Frostholm, L., & Olesen, F. (2005). Mental disorders in primary care: prevalence and co-morbidity among disorders. Results from the functional illness in primary care (FIP) study. Psychological Medicine, 35(8), 1175–1184. https://doi.org/10.1017/S0033291705004459
van Dongen, J. M., van Berkel, J., Boot, C. R. L., Bosmans, J. E., Proper, K. I., Bongers, P. M., van der Beek, A. J., van Tulder, M. W., & van Wier, M. F. (2016). Long-term cost-effectiveness and return-on-investment of a mindfulness-based worksite intervention results of a randomized controlled trial. Journal of Occupational and Environmental Medicine, 58(6), 550–560. https://www.jstor.org/stable/48501319
Vindholmen, S., Høigaard, R., Espnes, G. A., & Seiler, S. (2014). Return to work after vocational rehabilitation: does mindfulness matter? Psychology Research and Behavior Management, 7, 77–88. https://doi.org/10.2147/prbm.S56013
Vonderlin, R., Biermann, M., Bohus, M., & Lyssenko, L. (2020). Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mindfulness, 11(7), 1579–1598. https://doi.org/10.1007/s12671-020-01328-3
Vonderlin, R., Müller, G., Schmidt, B., Biermann, M., Kleindienst, N., Bohus, M., & Lyssenko, L. (2021). Effectiveness of a mindfulness- and skill-based health-promoting leadership intervention on supervisor and employee levels: a quasi-experimental multisite field study. Journal of Occupational Health Psychology, 26(6), 613–628. https://doi.org/10.1037/ocp0000301
Ward, M. E., De Brún, A., Beirne, D., Conway, C., Cunningham, U., English, A., Fitzsimons, J., Furlong, E., Kane, Y., Kelly, A., McDonnell, S., McGinley, S., Monaghan, B., Myler, A., Nolan, E., O’Donovan, R., O’Shea, M., Shuhaiber, A., & McAuliffe, E. (2018). Using co-design to develop a collective leadership intervention for healthcare teams to improve safety culture. International Journal of Environmental Research and Public Health, 15(6), 1182. https://doi.org/10.3390/ijerph15061182
World Health Organization. (2002). Prevention and promotion in mental health. World Health Organization Press.
World Health Organization. (2005). Mental health policies and programmes in the workplace. World Health Organization Press.
Zhang, J., Song, L. J., Ni, D., & Zheng, X. (2020). Follower mindfulness and well-being: the mediating role of perceived authentic leadership and the moderating role of leader mindfulness. Frontiers in Psychology, 11, 879. https://doi.org/10.3389/fpsyg.2020.00879
Żołnierczyk-Zreda, D., Sanderson, M., & Bedyńska, S. (2016). Mindfulness-based stress reduction for managers: a randomized controlled study. Occupational Medicine, 66(8), 630–635. https://doi.org/10.1093/occmed/kqw091
Acknowledgements
This project was awarded the Best Intervention Award by the American Psychological Association, the Society of Occupational Health Psychology, and the National Institute of Occupational Safety and Health at the Work, Stress, and Health Conference 2019 in Philadelphia, PA, USA.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research was supported by grants from a German health insurance company (AOK BW). LL and MB received fees for treatment development and providing training. GM is an employee of the sponsor. None of the authors has any financial interest in this research.
Author information
Authors and Affiliations
Contributions
Ruben Vonderlin: conceptualization, data assessment, assisting in analyzing and interpretation of data, writing – original draft preparation, editing. Burkhard Schmidt: conceptualization, supervision, editing. Miriam Biermann: data assessment, editing. Lisa Lyssenko: conceptualization, supervision, editing. Monika Heinzel-Gutenbrunner: supervision of analyzing data, editing. Nikolaus Kleindienst: supervision of analyzing data, editing. Martin Bohus: conceptualization, supervision, editing. Gerhard Müller: conceptualization, analyzing and interpretation of data, writing – original draft preparation, editing.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the ethical review committee at the University of Heidelberg, Medical Faculty Mannheim (2017-562N-MA).
Informed Consent
The works council and executive boards of the companies were informed about the research program and gave their consent. Participants in the experimental and control group were provided with an information sheet and a consent form and afterward gave their written informed consent.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vonderlin, R., Schmidt, B., Biermann, M. et al. Improving Health and Reducing Absence Days at Work: Effects of a Mindfulness- and Skill-Based Leadership Intervention on Supervisor and Employee Sick Days. Mindfulness 14, 1751–1766 (2023). https://doi.org/10.1007/s12671-023-02172-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02172-x