Abstract
Objectives
A substantial proportion of trauma survivors with posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) continue to experience symptoms even after trauma-focused therapies. Internet-based interventions could facilitate access to treatment for PTSD and CPTSD. The current pilot study aimed to investigate the effects of mindfulness-based internet intervention on PTSD and CPTSD symptoms.
Methods
A randomized controlled trial (RCT) design with two measurement points (pre-test and post-test) was used to investigate the effects of a structured mindfulness-based internet intervention on PTSD and CPTSD symptoms as well as anxiety, depression, and positive mental health. In total, 70 university students with high levels of PTSD and CPTSD symptoms based on ICD-11 criteria participated in the study: 31 in the intervention group and 39 in the waiting list control group.
Results
We found that the mindfulness-based internet intervention reduced CPTSD disturbances in self-organization (DSO) symptoms (ES = − 0.48 [− 0.96; 0.00]), particularly negative self-concept (ES = − 0.72 [− 1.21; − 0.24]) and disturbances in relationships (ES = − 0.55 [− 1.03; − 0.07]). Moreover, the intervention reduced the symptoms of PTSD sense of threat (ES = − 0.48 [− 0.96; − 0.01]) and promoted positive mental health (ES = 0.51 [0.03; 0.99]). High user satisfaction and good usability of the intervention were reported.
Conclusions
Promising treatment effects were found, indicating that mindfulness-based internet intervention can reduce CPTSD symptoms and have a positive effect on mental health among youth in general. The findings of the current study contribute to the further development of trauma care using internet-delivered interventions.
Trial registration: ClinicalTrials.gov NTC04333667 (3 April 2020)
Similar content being viewed by others
Posttraumatic stress disorder (PTSD) is among the most often diagnosed mental disorders worldwide (Maercker et al., 2013), resulting in a high burden and high costs for society. Effective treatments for PTSD have been developed over the last decade (Bisson & Olff, 2021). Currently, American Psychological Association (APA, 2017) and International Society for Traumatic Stress Studies (ISTSS, 2018) include cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), cognitive therapy (CT), prolonged exposure therapy (PE), eye movement and desensitization therapy (EMDR). However, a substantial proportion of persons with PTSD continue to experience symptoms even after trauma-focused therapies (Bradley et al., 2005). In addition, high dropout rates have been associated with trauma-focused PTSD treatments (Lewis et al., 2020b).
The World Health Organization (2018) has included a new diagnosis of complex posttraumatic stress disorder (CPTSD) in the International Classification of Diseases (ICD-11) in addition to PTSD. According to the ICD-11, PTSD can be diagnosed if a person was exposed to traumatic experiences and meets all PTSD diagnostic criteria (symptoms of re-experiencing, avoidance, sense of threat, and functional impairment associated with these symptoms). CPTSD can be diagnosed if all criteria for PTSD and additional criteria for symptoms of disturbances in self-organization (DSO) (affect dysregulation, negative self-concept, disturbances in relationships) and functional impairment associated with these DSO symptoms are met (World Health Organization, 2018).
However, the new CPTSD diagnosis raises a lot of questions regarding treatment approaches of complex trauma. There is an ongoing debate over whether CPTSD requires a different kind of treatment to PTSD (Brewin, 2020), and there is an urgent need to research the effects of available and new psychological therapies for treatment of CPTSD. The current debate is also focused on the question of whether traditional exposure-based treatments are feasible for CPTSD. It has been suggested that an alternative phased approach, which starts with stabilization techniques helping trauma survivors to deal with affect regulation symptoms, should be applied in CPTSD treatment (Brewin, 2020). After reviewing two meta-analyses of recent treatment outcome studies, Karatzias and Cloitre (2019) suggested that although current PTSD therapies are effective, they have fewer benefits for individuals who are likely to have CPTSD, and thus multicomponent therapies might be an approach by which outcomes could be improved.
Mindfulness-based therapies have recently received attention as having the potential to treat various mental health problems, including PTSD (Colgan et al., 2016; Jasbi et al., 2018; Valenstein-Mah et al., 2019). Mindfulness can be described as the awareness that emerges through purposefully paying attention to the present moment and nonjudgmentally experiencing the unfolding moments (Kabat-Zinn, 2003). It is hypothesized that practicing mindfulness diminishes physiological arousal, increases attention control, and fosters acceptance of unwanted experiences, each of which addresses processes that maintain PTSD (Lang et al., 2012). Empirical evidence supports the view that mindfulness-based interventions may reduce PTSD symptoms in various populations (Colgan et al., 2016; Jasbi et al., 2018; Valenstein-Mah et al., 2019). Moreover, mindfulness-based treatments may reduce comorbid symptoms of depression and anxiety (Jasbi et al., 2018), as well as improve positive mental health aspects, such as resilience (Reyes et al., 2020) after traumatic experiences. Although a more detailed investigation is needed, dropout rates for existing mindfulness treatments for PTSD seem to be low (from none to 13.3%; Jasbi et al., 2018; Valenstein-Mah et al., 2019). Additionally, mindfulness-based therapies have potential to regulate affect (Guendelman et al., 2017), improve self-concept (Crescentini & Capurso, 2015) and relationships (Karremans et al., 2017). Each of these constitutes CPTSD DSO symptoms and, therefore, indicates that mindfulness could be delivered as an approach to reduce CPTSD symptoms. Thus, mindfulness-based treatments could be used in the initial stabilization phase of CPTSD treatment before the application of exposure-based treatments, particularly among individuals with high levels of DSO symptoms, such as emotional dysregulation. Alternatively, mindfulness could be integrated into CPTSD multicomponent trauma treatment which targets specific CPTSD symptoms.
To tackle the barriers of accessing PTSD treatments, internet-based interventions have been suggested as an alternative (Kazlauskas, 2017). The widespread availability of digital technology has caused a significant change in the delivery of the psychological treatments for mental health problems (Fairburn & Patel, 2017). The COVID-19 pandemic has highlighted that internet-delivered interventions may be necessary to consider not only as an alternative but also as the only possible intervention strategy (Wind et al., 2020). A narrative umbrella review of recent meta-analyses examining the effects of internet-based interventions for various mental health outcomes suggested that internet-delivered cognitive behavior therapy can be effective for a range of mental health problems, including panic disorder, social anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder (based on DSM-IV criteria), and major depression (Andersson et al., 2019). Likewise, a meta-analysis of internet-delivered cognitive behavioral therapy for PTSD showed beneficial effects of internet-based interventions for PTSD, based on DSM and ICD (Lewis et al., 2018). However, to the best of our knowledge, no studies have explored internet-delivered interventions based both on cognitive behavioral therapy or mindfulness principles for the treatment of PTSD and CPTSD symptoms based on ICD-11 criteria. With the recent inclusion of CPTSD in the ICD-11 empirical evidence is needed for using it in a clinical setting (Karatzias & Cloitre, 2019).
The lack of knowledge about ICD-11 PTSD and CPTSD treatments highlights the need for identifying feasible treatments for these clinical conditions. Mindfulness-based treatments could be a promising option as an internet-based intervention. Therefore, the primary aim of the current pilot study was to investigate the effects of a mindfulness-based internet intervention on PTSD and DSO symptoms (prerequisite criteria to diagnose CPTSD) in a randomized controlled trial which compared an intervention group with a waiting list control group of young adults experiencing high levels of ICD-11 PTSD, CPTSD, or DSO symptoms. The secondary aim was to investigate the effects of the intervention on depression and anxiety symptoms, and positive mental health. Finally, we sought to evaluate user satisfaction and program usability of the newly developed mindfulness-based internet intervention.
Method
Participants
In total, 70 university students (Mage = 23.34, SDage = 3.11; 87.1% female) exposed to various traumatic experiences were included in the trial and were randomly allocated to intervention (n = 31) or control (n = 39) group. The power analysis revealed that the total sample of 66 participants was sufficient to detect the effect sizes of 0.25, indicating the differences between the two groups by using the multivariate two-measures data analytic approach (given a significance level of .05 and a power of 80%). Descriptive data on study participants at the pre-test are presented in Table 1. No differences were observed in terms of demographic characteristics between the groups, except for gender. There were significantly more male participants in the intervention group as compared to the control group (see Table 1).
We included participants who met the following criteria: (1) were 18 years old or older; (2) were fluent in the Lithuanian language; (3) had access to a device with an internet connection; (4) had experienced at least one traumatic event in their lifetime; (5) met the clinical significance criteria for PTSD, CPTSD, or DSO only with or without functional impairment as measured with the International Trauma Questionnaire (Cloitre et al., 2018). Participants without functional impairment were included in the study regardless, given the fact that the study was carried out during the beginning of the COVID-19 pandemic, and therefore, functional impairment in social, occupational, and other areas might have been affected significantly due to the context of the pandemic. The pre-defined exclusion criteria were as follows: (1) current acute case of psychiatric care; (2) currently experienced ongoing interpersonal violence; (3) current abuse of alcohol or drugs. None of the participants met the exclusion criteria. In addition, a suicidal crisis intervention plan was prepared, which included contacting study participants via phone call and directing them to crisis assistance services in a community. However, there were no participants with suicidal risk in the study.
Participants’ Exposure to Traumatic Events. The exposure to traumatic events at the pre-test is presented in Table 2. No differences were found between the intervention and waiting list control groups regarding the mean score of experienced traumatic events. Also, there were no differences in exposure to specific traumatic events, except for life-threatening illness or injury, which was significantly more often reported in the intervention group than in the control group. The most prevalent traumatic event types both in the intervention and control groups were severe human suffering (exposure rate over 70%) and childhood physical abuse (exposure rate over 50%). The index trauma of the participants from the intervention and control groups were as follows: death of someone close (25.8% vs. 17.9%), sexual trauma (16.1% vs. 12.8%), physical abuse (12.9% vs. 20.5%), serious illness (9.7% vs. 7.7%), psychological abuse (9.7% vs. 17.9%), transportation accident (0% vs. 2.6%), several traumatic events (0% vs. 2.6%), and other traumatic events (25.8% vs. 17.9%). The time when the traumatic event occurred varied both in the intervention and control groups: exposure less than 6 months ago (16.1% vs. 23.1%), 6–12 months ago (12.9% vs. 12.8%), 1–5 years ago (29.0% vs. 28.2%), 5–10 years ago (12.9% vs. 15.4%), 10–20 years ago (22.6% vs. 17.9%), and more than 20 years ago (6.5% vs. 2.6%).
Intervention-Control Comparison. Descriptive information on participants’ PTSD and DSO symptom scores as well as depression symptom scores, anxiety symptom scores, and positive mental health scores at the pre-test are presented in Table 3. The t-tests showed no significant differences between the intervention and waiting list control groups at pre-test for any primary or secondary outcomes. No differences were found on PTSD symptoms (t(68) = 1.55, p = .125) or DSO symptoms (t(68) = − 0.02, p = .983). Also, no differences were found between the two groups for depression symptoms (t(68) = 0.62, p = .538), anxiety symptoms (t(68) = 0.35, p = .724), and positive mental health (t(68) = 0.94, p = .350). In the intervention group, 9.7% (n = 3) of the participants met criteria for diagnostic status of PTSD, and 38.7% (n = 12) of the participants met criteria for diagnostic status of CPTSD. In the control group, 25.6% (n = 10) of the participants met criteria for diagnostic status of PTSD, and 46.2% (n = 18) of the participants met criteria for diagnostic status of CPTSD. There were no differences between the intervention and control groups in terms of current mindfulness practices (3.2% vs. 5.1%; χ2(1) = 0.15, p = .696), current visits to a psychologist (19.4% vs. 12.8%; χ2(1) = 0.56, p = .456), and current use of medicine due to mental health problems (19.4% vs. 30.8%; χ2(1) = 1.18, p = .278). In the context of the COVID-19 pandemic, participants were also asked about their experiences related to COVID-19. None of the participants were or had been infected with coronavirus. None of the participants from the control group had a close family member or friend infected; there was one such case in the intervention group.
Procedure
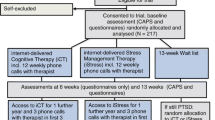
Data were collected at two timepoints, March to April (pre-test/T1) and June to July (post-test/T2) 2020. Information about the study and the invitation to participate was sent by academic e-mail to all students at one of the largest research-oriented comprehensive Lithuanian universities and posted on the University’s Facebook page. In addition, information was announced via University Students’ Representation which posted information on separate faculties’ Facebook pages and encouraged students to participate in the study by sending them additional e-mails. Individuals interested in participation registered on the study website (www.stillme.lt) and completed the pre-test measures. After registration, individuals who had completed all the required measures were contacted for a structured phone interview. Inclusion was finalized after the phone interviews. A flowchart of the inclusion in the study is presented in Fig. 1.
Participants who met all inclusion criteria and had completed the pre-test measures were randomly assigned to either the intervention or waiting list control group. Randomization was based on a computer-generated randomization list (www.random.org) and was performed by an independent researcher. No stratification was applied. Participants were informed that they would be randomly allocated to either the intervention or waiting list control group. Participants assigned to the intervention group started using the program right after the randomization, whereas participants assigned to the waiting list control group were informed that they would get access to the program in 5 months.
All data reported in the trial were collected online, and participants were given standardized reminders to complete the assessments using the online assessment system. The study was approved by Vilnius University Psychology Research Ethics Committee (Reference No. 27-02-2020/36). All participants gave their informed consent for participation before filling the pre-test questionnaires. In the current study, the data are reported following the CONSORT statement for reporting parallel group trials (Schulz et al., 2011).
Intervention. A mindfulness-based internet intervention was developed specifically for the current study. It was aimed at university students who had been exposed to traumatic life events and experienced PTSD or CPTSD symptoms. The intervention was designed as a self-help program with the possibility of sending messages to a psychologist. The program was delivered through a secure online platform Iterapi (Vlaescu et al., 2016), which had been used in many previous studies, and translated into Lithuanian. The content of the intervention was developed by a team of psychologists, based on mindfulness principles with a focus on psychoeducation (which explicitly addressed traumatic experiences as well as PTSD and CPTSD symptoms followed by mindfulness benefits) and mindfulness techniques training. Eight modules included: (1) Introduction, (2) Awareness and nonjudgment of physical senses, (3) Physical senses in everyday life, (4) Awareness and nonjudgment of thoughts, (5) Thoughts in everyday life, (6) Awareness and nonjudgment of emotions, (7) Emotions in everyday life, and (8) Summary. The content of the program is presented in Table 4. Each module consisted of psychoeducation, two or three mindfulness exercises, and a reminder of the possibility to contact the psychologist. The mindfulness exercises were provided as audio recordings. The length of the audio recordings was approximately 2 to 7 minutes. Participants had the possibility to download each of the audio recordings to their devices. Participants could choose the intensity of the program according to their personal needs but were encouraged to practice at least one exercise every day. Access to a new module was provided every week on the same weekday over the 8 weeks. Once accessible, modules remained available throughout the intervention.
Two clinical psychologists and one Master’s student in the Clinical psychology program were involved as psychologists in the study. They received special training according to the guidelines developed specifically for the study. Weekly supervision meetings were scheduled, and extra supervisions were provided on request. The psychologist’s role included supporting the participants, offering feedback, and answering questions. The psychologist’s feedback was largely standardized, but individualization was encouraged to fit specific questions of the participants. Participants communicated with the psychologists asynchronously by writing and uploading their texts within a secure platform (Vlaescu et al., 2016), while psychologists provided feedback subsequently within 24 h. In total, psychologists wrote 15 texts of feedback to 8 participants of the study; other participants did not contact psychologists. Each feedback from psychologists took from 10 to 60 min.
Measures
Exposure to Traumatic Experiences. The DSM-5 Life Events Checklist (LEC-5) (Weathers et al., 2013) was used to assess the lifetime exposure to 18 traumatic experiences such as physical or sexual assault, life-threatening illness, or injury with one additional item assessing any other extremely stressful life event. The type of exposure to traumatic events was assessed with five possible response options: 1 (= “happened to me”), 2 (= “witnessed it”), 3 (= “learned about it”), 4 (= “not sure”), and 5 (= “does not apply”). In the current study, exposure to traumatic experience was considered if participants reported that traumatic experience either happened to them (1) or they witnessed it (2). The Lithuanian version of the measure has been used in previous research (Kazlauskas et al., 2018).
Symptoms of PTSD and CPTSD. The International Trauma Questionnaire (ITQ) (Cloitre et al., 2018), based on the WHO ICD-11 principles for PTSD and CPTSD diagnosis, was used to measure PTSD and CPTSD symptoms. Participants were instructed to indicate an experience based on DSM-5 Life Events Checklist (LEC-5; Weathers et al., 2013) that affected them the most, to briefly describe it, and provide responses to the ITQ regarding that traumatic experience. The ITQ is comprised of 18 items. Six items, two for assessment of each of the three PTSD symptom clusters in the past month, are divided into three subscales: two items for re-experiencing, two items for avoidance, and two items for a sense of threat symptoms. The score of the ITQ PTSD symptom part has a range from 0 to 24. The DSO symptoms in the past month are also measured with the six symptom items on the three subscales, in particular, affective dysregulation, negative self-concept, and disturbances in relationships symptoms, with two items for each of the DSO symptom clusters. The score of the ITQ DSO part has a range from 0 to 24. Additional six functional impairment items of the ITQ assess how PTSD (three items) and DSO (three items) symptoms impaired functioning in the past month. Participants rate the ITQ items on a 5-point Likert scale ranging from 0 (= “not at all”) to 4 (= “extremely”). A score of ≥ 2 for at least one of the two items representing a particular PTSD and DSO symptom cluster indicates clinical significance based on the diagnostic algorithm proposed by the authors of the ITQ (Cloitre et al., 2018). A probable PTSD diagnosis is given when all three PTSD symptoms are clinically significant and if they significantly impair their functioning in at least one area of life. Diagnosis of CPTSD requires that the diagnostic criteria for PTSD are met, all three symptom clusters of DSO are clinically significant, and DSO symptom-related significant functional impairment in at least one area in life is reported. In the current sample, the internal consistency was high for the full ITQ scale (Cronbach’s alpha, α = .82) and acceptable for the subscales of PTSD symptoms (α = .75) and DSO symptoms (α = .68).
Depression. Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001) was used to measure symptoms of depression. The Lithuanian version of PHQ-9 was used (Montvidas, 2018). Participants rate the statements on a 4-point Likert scale ranging from 0 (= “not at all”) to 3 (= “nearly every day”) by assessing whether they have been bothered by the loss of interest in doing things, fatigue, appetite problems, negative depressive thoughts within the last 2 weeks. The total score of PHQ-9 has a range from 0 to 27. The 10th item assesses how these problems impede work (from 0 = “not difficult at all” to 3 = “extremely difficult”). In the current study, good internal consistency of the PHQ-9 (α = .80) was found.
Anxiety. The Generalized Anxiety Disorder Scale‐7 (GAD-7) (Spitzer et al., 2006) was used to measure anxiety symptoms. The Lithuanian version of GAD-7 was used (Butkutė-Šliuožienė, 2019). GAD-7 measures general anxiety symptoms over the past two weeks. Seven statements (such as “Not being able to stop or control worrying”) are scored on a Likert scale from 0 (= “not at all”) to 3 (= “nearly every day”). The total score of GAD-7 has a range from 0 to 21. In the current study, Cronbach’s alpha of the full scale was high (α = .90).
Positive Mental Health. Positive Mental Health Scale (PMH) (Lukat et al., 2016) was used to assess positive mental health. The PMH comprises nine items measuring the emotional, cognitive, and social aspects of positive mental health. Participants rated statements such as “In general, I am confident,” “Much of what I do brings me joy,” on a Likert scale from 0 (= “do not agree”) to 3 (= “agree”). The total score of PMH has a range from 0 to 27. The Lithuanian version of the scale has been used in previous research and demonstrated good psychometric characteristics (Truskauskaite-Kuneviciene et al., 2020). In the current study, Cronbach’s alpha of the full scale was high (α = .84).
User Satisfaction and Program Usability. Six items were used to assess satisfaction with using the program and program usability. The participants in the intervention group were asked to rate how useful (from 1 = “not useful at all” to 5 = “very useful”), satisfactory (from 1 = “I didn’t like it at all” to 5 = “I liked it a lot”), and easy to use (from 1 = “it was not easy at all” to 5 = “it was very easy”) the program was. They were also asked to report their subjective impression regarding the improvement of mental well-being (from 1 = “worsened a lot” to 5 = “improved a lot”), general understanding of oneself and one’s well-being (from 1 = “not at all” to 5 = “definitely yes”), and recommending the program to a person who had experienced a traumatic event in their lifetime (from 1 = “not at all” to 5 = “definitely yes”).
Data Analyses
Since we aimed to capture the possible change in used constructs, we performed a series of multivariate repeated measures ANOVAs with time (pre-test and post-test) as a within-subject factor and group (intervention vs. control) as a between-subject factor. First, we tested the intervention effects on PTSD and DSO symptoms using the sum scores for each measure. Then, we separately tested the PTSD symptoms subscales of re-experiencing, avoidance, and sense of threat. We also performed an analysis of the DSO symptoms subscales of affective dysregulation, negative self-concept, and disturbances in relationships. Finally, we tested the secondary outcomes (depression, anxiety, and positive mental health) using the sum scores of the respective measures.
We calculated both within-group and between-group effect sizes. The between-group effect sizes were calculated using the mean difference from pre-test to post-test in the intervention and control groups and the standard deviations of each group at pre-test (Morris, 2008). The within-group effect sizes were calculated using the means in each group at pre-test and post-test and standard deviations at each measurement point. Bias-corrected effect sizes (Fritz et al., 2012) were reported. The magnitude of the effect expressed in d was interpreted according to Cohen (1988), that is, 0.50 = medium effect, and 0.80 = large effect.
We used the Reliable change index (RCI) to calculate clinically significant changes (Iverson, 2019). For RCI calculations, we used the PTSD and CPTSD sum scores, standard deviations of the pre-test in the intervention group, and test-retest reliability of the respective scale. Independent samples t-test and χ2-test were used to test for between-group differences on demographic characteristics, trauma exposure prevalence, primary and secondary outcomes. Data analyses were performed using IBM SPSS Statistics version 26.
Results
Engagement and Dropout
Participants from the intervention group were considered engaged in the current study if they had logged in to the intervention site at least once. All intervention group participants met this criterion. Of those who provided post-test assessments, 35.5% logged in < 5 times, 12.9% logged in 5–10 times, 19.4% logged in 11–20 times, and 32.3% logged in > 20 times. A majority (77.5%) of participants from the intervention group and 95.1% from the waiting list control group provided post-test assessments. Participants who provided post-test assessments were considered completers, while the remaining were considered dropouts.
There were no differences in terms of demographic characteristics between completers and dropouts at pre-test including gender (χ2(1) = 0.03, p = .864), age (t(39) = - 0.04, p = .972), nationality (χ2(1) = 0.33, p = .565), partnership status (χ2(1) = 2.27, p = .132), employment status (χ2(1) = 3.66, p = .056), and financial situation (χ2(3) = 2.68, p = .444). Also, completers and dropouts did not differ in their current mindfulness practices (χ2(1) = 0.33, p = .565), current visits to a psychologist (χ2(1) = 2.27, p = .132), current use of medicine due to mental health problems (χ2(1) = 2.27, p = .132) as well as COVID-19 experiences. Completers and dropouts did not significantly differ in terms of any primary or secondary outcomes. No differences were observed between completers and dropouts for PTSD symptoms (t(39) = − 0.24, p = .816), DSO symptoms (t(39) = − 0.14, p = .888), depression symptoms (t(39) = − 0.35, p = .730), anxiety symptoms (t(39) = − 0.52, p = .606), and positive mental health (t(39) = 0.55, p = .586) at pre-test.
Intervention Effects on Primary and Secondary Outcomes
The results of the repeated measures MANOVA analyses and the between-group, as well as within-group effect sizes, are presented in Table 3. At the multivariate level, the analyses revealed a significant difference in change of PTSD and DSO symptoms sum scores over time between the intervention and control groups (Wilks’ λ = 0.91). At the univariate level, we found a significantly higher decrease in the DSO score in the intervention group compared to the control group. No significant differences in the change of PTSD scores were found between the groups. The between-group effect size indicated a small intervention effect on the reduction of DSO score. The within-group effect sizes indicated a large decrease in the PTSD score and a moderate decrease in the DSO score in the intervention group.
Separate repeated measures MANOVA analyses of the PTSD symptom clusters (re-experiencing, avoidance, and sense of threat) and DSO symptom clusters (affective dysregulation, negative self-concept, and disturbances in relationships) were performed. At the multivariate level, the analyses revealed no significant difference in change of the PTSD symptom clusters over time between the intervention and control groups (Wilks’ λ = 0.94). Likewise, no significant differences in change of the PTSD symptom clusters were found among the two groups at the univariate level. The between-group effect sizes showed a small intervention effect on the reduction of the PTSD sense of threat symptoms. The within-group effect sizes indicated a moderate decrease in PTSD avoidance symptoms and a large decrease in sense of threat symptoms in the intervention group.
The repeated measures MANOVA analyses showed a significant difference in change of DSO symptom clusters over time between the intervention and control groups (Wilks‘ λ = 0.83). At the univariate level, we observed a significantly higher decrease of DSO negative self-concept and disturbances in relationships symptoms in the intervention group compared to the control group. No significant differences in change of affective dysregulation were found among the two groups. Between-group effect sizes indicated moderate intervention effects on the reduction of negative self-concept and disturbances in relationships. The within-group effect sizes showed a moderate decrease in negative self-concept and disturbances in relationships in the intervention group.
Finally, the repeated measures MANOVA analyses of change in depression, anxiety, and positive mental health revealed a significant difference between the intervention and control groups (Wilks’ λ = 0.88). At the univariate level, we found a significantly higher increase of positive mental health in the intervention group compared to the control group. No significant differences in change of depression and anxiety were found among the two groups. Likewise, the between-group effect size indicated a moderate intervention effect on the increase of the positive mental health (see Table 3).
Clinical Significance of the Intervention Effects
The results of the RCI analyses by using PTSD and CPTSD symptoms sum scores indicated that 32.3% (n = 10) of the participants in the treatment group experienced a clinically significant decrease in their PTSD symptoms from pre-test to post-test. In the control group, 2.6% (n = 1) experienced a clinically significant reduction in their PTSD symptoms over time. Similarly, 52.6% (n = 16) of the treatment group experienced a clinically significant decrease in their CPTSD symptoms from pre-test to post-test. In the control group, 23.1% (n = 9) of participants experienced a clinically significant reduction in their CPTSD symptoms.
User Satisfaction and Program Usability
At the end of the intervention, a majority of the intervention group participants reported that the program had been useful (80.7%), satisfactory (83.9%), and easy to use (93.6%). Also, more than half of the participants reported that the program improved their mental well-being (61.3%) as well as general understanding of themselves and their well-being (64.6%). Finally, a greater part of participants indicated that they would recommend the program to a person who had experienced a traumatic event in their lifetime (77.5%).
Discussion
The current study investigated the effects of a mindfulness-based internet intervention on ICD-11 PTSD and CPTSD symptoms. We found promising treatment effects indicating that mindfulness-based internet intervention can reduce CPTSD symptoms of negative self-concept and disturbances in relationships, as well as have positive effects on positive mental health. Our study also revealed that participant user satisfaction was high, and the usability of our intervention was perceived as very good.
The PTSD symptom changes in the present study were not in line with the other studies on mindfulness-based interventions for PTSD. We did not find significant changes in overall PTSD symptoms in our study, except for the sense of threat symptoms. Previous randomized clinical trials provided promising initial findings that various PTSD experiencing samples could benefit from mindfulness-based PTSD treatments (Colgan et al., 2016; Jasbi et al., 2018; Valenstein-Mah et al., 2019). Furthermore, our findings are different from a recent study on internet-delivered mindfulness intervention for PTSD (Reyes et al., 2020). Possibly, the best treatments for PTSD are trauma-focused PTSD therapies that explicitly address previous traumatic experiences and traumatic memories (APA, 2017; ISTSS, 2018; Lewis, et al., 2020a). In contrast, mindfulness-based therapies focus on the present, and thus, traumatic experiences can be avoided during the mindfulness intervention process, and therefore no treatment effects on PTSD symptoms may occur.
However, the present study revealed the potential of a mindfulness-based intervention for a new ICD-11 diagnosis of CPTSD. Overall, the intervention was effective for DSO symptoms which are required for the diagnosis of CPTSD in addition to the three core PTSD symptom clusters. In particular, participants who received mindfulness-based internet intervention reported positive changes in the DSO negative self-concept, meaning that beliefs about oneself as diminished, defeated, and worthless were reduced. In addition, feelings of shame, guilt, and failure, which commonly accompany negative beliefs about oneself, were reduced in the intervention group. Also, trauma-exposed young adults seemed to encounter fewer difficulties in sustaining relationships and feeling close to other people after using an 8-week mindfulness-based internet intervention.
The findings of the present study suggest that mindfulness-based interventions could have a significant positive impact on DSO symptoms, which accompany PTSD symptoms when CPTSD is diagnosed. There is an ongoing debate among experts on trauma treatment whether trauma-focused interventions such as exposure should be offered to clients with CPTSD, or if a phased trauma treatment approach should be used instead which would imply starting the CPTSD treatment with stabilization techniques to aid better coping skills of the emotional regulation (Brewin, 2020). The current study indicates that mindfulness can be an important first step for survivors of prolonged or severe trauma exposure with CPTSD, as an effective technique for reducing DSO symptoms during the first stabilization phase. Alternatively, based on our findings, mindfulness could be integrated into CPTSD multicomponent trauma treatment targeted for specific CPTSD symptoms in clinical practice. In particular, clients suffering from negative self-concept and disturbances in relationships could benefit from mindfulness-based interventions.
Recent theoretical conceptualizations aimed to explain potential mechanisms of change on how mindfulness-based interventions could reduce PTSD symptoms. It has been hypothesized that mindfulness diminishes physiological arousal, increases attentional control, and fosters acceptance of unwanted experiences, each of which addresses processes that maintain PTSD (Lang et al., 2012). We assume that this could also be applied to the DSO symptoms, as mindfulness could increase self-regulation capacity, which could positively impact self-concept and relationships. While this pilot study could not reveal the mechanisms underlying the identified therapeutic changes, further studies could explore the factors contributing to DSO symptoms changes. The DSO symptoms change observed in our study is a promising finding that is valuable for the future development of CPTSD interventions, as it indicates that mindfulness could be beneficial in DSO symptoms reduction and could be potentially used as an integral part of CPTSD intervention to reduce DSO symptoms, and exposure-based or cognitive therapies could be used to tackle PTSD symptoms.
Limitations and Future Research
Several limitations of the present study should be considered when interpreting the findings. To begin with, it was a pilot study and therefore, the sample size was relatively small, which may have resulted in less statistical power to detect smaller differences between the two conditions. As the study provided promising initial findings, future studies with larger samples would allow testing the differences between two conditions with more confidence. Furthermore, the study was conducted with a waiting list as a control condition. The results could be replicated with an active control condition using treatment as usual or alternative trauma-focused evidence-based treatment protocol in future trials. This would allow testing whether mindfulness-based PTSD and CPTSD treatments have unique benefits compared to other treatments. In addition, the focus of the study was the reduction in PTSD and CPTSD symptoms. We included participants who reported clinically significant PTSD or CPTSD symptoms, and participants with subclinical levels of PTSD and CPTSD, which could have affected non-significant changes in PTSD symptoms. The results should be replicated in a sample of participants with full PTSD or CPTSD diagnosis. The participants in the study had the possibility to download mindfulness exercises to their devices to aid usability; however, this restricted the possibility of monitoring the use of the downloaded intervention exercises. We have chosen an operationalization of engagement to the study as logging in to the intervention site at least once. However, more accurate measures of engagement such as exercise completion should be used in future studies.
Regarding the measurement of the outcomes, participants’ trauma exposure and PTSD and CPTSD symptoms were assessed using self-reported measures without a clinical interview, which could have led to an inaccurate estimation of PTSD and CPTSD symptomatology. In future trials, the clinician’s administered assessment could be implemented to facilitate a more accurate evaluation of PTSD or CPTSD symptoms as experienced by the participants. However, at the time of the study, ICD-11 CPTSD diagnostic interviews were not yet available. Additionally, the ITQ DSO scale’s Cronbach alpha was low compared to other studies (Murphy et al., 2020) possibly due to the relatively small sample size.
Conclusions about the generalizability of our findings in treating ICD-11 PTSD and CPTSD using mindfulness in other populations across the lifespan are limited. Thus, it would be valuable to test whether this intervention is only helpful for young adults or could also be beneficial in other samples. Finally, the study was conducted in the context of the COVID-19 pandemic. Pandemic-related stressors could have contributed to participants’ mental health and potentially could have played a role in the study outcomes. It has been hypothesized that PTSD and CPTSD symptoms can increase during such circumstances (Liu et al., 2020). Therefore, it would be useful to evaluate whether mindfulness-based internet intervention effects would be the same in regular conditions after the end of the coronavirus pandemic.
The current study showed the potential of internet-based mindfulness interventions to alleviate disturbances in self-organization symptoms which are prerequisites to a new ICD-11 diagnosis of CPTSD in a sample of young adults. A mindfulness-based approach could broaden the perspective of treatments for CPTSD as an integral part of multicomponent modular CPTSD therapy in addition to trauma-focused treatment. Also, our study revealed that internet-delivered interventions could be beneficial for adults who experience CPTSD symptoms. In the context of existing barriers for the delivery of face-to-face treatments, internet-based interventions for traumatized individuals should be further explored. Moreover, it is of great importance to explore in future trials whether the effects of mindfulness-based internet interventions in traumatized populations sustain over time.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
American Psychological Association. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. https://doi.org/10.1162/jocn
Andersson, G., Carlbring, P., Titov, N., & Lindefors, N. (2019). Internet interventions for adults with anxiety and mood disorders: A narrative umbrella review of recent meta-analyses. Canadian Journal of Psychiatry, 64(7), 465–470. https://doi.org/10.1177/0706743719839381
Bisson, J. I., & Olff, M. (2021). Prevention and treatment of PTSD: The current evidence base. European Journal of Psychotraumatology, 12(1). https://doi.org/10.1080/20008198.2020.1824381
Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 162(2), 214–227. https://doi.org/10.1177/153476560501100304
Brewin, C. R. (2020). Complex post-traumatic stress disorder: A new diagnosis in ICD-11. Bjpsych Advances, 26(3), 145–152. https://doi.org/10.1192/bja.2019.48
Butkutė-Šliuožienė, K. (2019). Generalizuoto nerimo sutrikimo skalė-7. Biological Psychiatry and Psychopharmacology, 21(1), 21–22. http://biological-psychiatry.eu/wp-content/uploads/2019/07/BPP_2019_21to22.pdf
Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., Karatzias, T., & Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. https://doi.org/10.1111/acps.12956
Cohen, J. (1988). Statistical power analysis for the behavoral sciences (2nd ed.). Lawrence Erlbaum Accociates.
Colgan, D. D., Christopher, M., Michael, P., & Wahbeh, H. (2016). The body scan and mindful breathing among veterans with PTSD: Type of intervention moderates the relationship between changes in mindfulness and post-treatment depression. Mindfulness, 7(2), 372–383. https://doi.org/10.1007/s12671-015-0453-0
Crescentini, C., & Capurso, V. (2015). Mindfulness meditation and explicit and implicit indicators of personality and self-concept changes. Frontiers in Psychology, 6, 1–6. https://doi.org/10.3389/fpsyg.2015.00044
Fairburn, C. G., & Patel, V. (2017). The impact of digital technology on psychological treatments and their dissemination. Behaviour Research and Therapy, 88, 19–25. https://doi.org/10.1016/j.brat.2016.08.012
Fritz, C. O., Morris, P. E., & Richler, J. J. (2012). Effect size estimates: Current use, calculations, and interpretation. Journal of Experimental Psychology: General, 141(1), 2–18. https://doi.org/10.1037/a0024338
Guendelman, S., Medeiros, S., & Rampes, H. (2017). Mindfulness and emotion regulation: Insights from neurobiological, psychological, and clinical studies. Frontiers in Psychology, 8, 1–23. https://doi.org/10.3389/fpsyg.2017.00220
ISTSS. (2018). Posttraumatic stress disorder prevention and treatment guidelines. Methodology and recommendations. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_PreventionTreatmentGuidelines_FNL.pdf.aspx
Iverson, G. L. (2019). Reliable Change Index. In J. Kreutzer, J. DeLuca, & B. Caplan (Eds.), Encyclopedia of Clinical Neuropsychology. Springer, Cham. https://doi.org/10.1007/978-3-319-56782-2_1242-3
Jasbi, M., Sadeghi Bahmani, D., Karami, G., Omidbeygi, M., Peyravi, M., Panahi, A., Mirzaee, J., Holsboer-Trachsler, E., & Brand, S. (2018). Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of post-traumatic stress disorder (PTSD) in veterans–results from a randomized control study. Cognitive Behaviour Therapy, 47(5), 431–446. https://doi.org/10.1080/16506073.2018.1445773
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10(2), 144–156. https://doi.org/10.1093/clipsy/bpg016
Karatzias, T., & Cloitre, M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. https://doi.org/10.1002/jts.22457
Karremans, J. C., Schellekens, M. P. J., & Kappen, G. (2017). Bridging the sciences of mindfulness and romantic relationships: A theoretical model and research agenda. Personality and Social Psychology Review, 21(1), 29–49. https://doi.org/10.1177/1088868315615450
Kazlauskas, E. (2017). Challenges for providing health care in traumatized populations: Barriers for PTSD treatments and the need for new developments. Global Health Action, 10(1). https://doi.org/10.1080/16549716.2017.1322399
Kazlauskas, E., Gegieckaite, G., Hyland, P., Zelviene, P., & Cloitre, M. (2018). The structure of ICD-11 PTSD and complex PTSD in Lithuanian mental health services. European Journal of Psychotraumatology, 9(1). https://doi.org/10.1080/20008198.2017.1414559
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lang, A. J., Strauss, J. L., Bomyea, J., Bormann, J. E., Hickman, S. D., Good, R. C., & Essex, M. (2012). The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification, 36(6), 759–786. https://doi.org/10.1177/0145445512441200
Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020a). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1). https://doi.org/10.1080/20008198.2020.1729633
Lewis, C., Roberts, N. P., Bethell, A., Robertson, L., & Bisson, J. I. (2018). Internet-based cognitive and behavioural therapies for posttraumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews, 2018(12). https://doi.org/10.1002/14651858.CD011710.pub2
Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020b). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1). https://doi.org/10.1080/20008198.2019.1709709
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290. https://doi.org/10.1016/j.psychres.2020.113172
Lukat, J., Margraf, J., Lutz, R., Der Veld, W. M., & Becker, E. S. (2016). Psychometric properties of the positive mental health scale (PMH-scale). BMC Psychology, 4(1), 1–14. https://doi.org/10.1186/s40359-016-0111-x
Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Van Ommeren, M., Jones, L. M., Humayan, A., Kagee, A., Llosa, A. E., Rousseau, C., Somasundaram, D. J., Souza, R., Suzuki, Y., Weissbecker, I., Wessely, S. C., First, M. B., & Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry, 12(3), 198–206. https://doi.org/10.1002/wps.20057
Montvidas, J. (2018). Paciento sveikatos klausimynas-9. Biological Psychiatry and Psychopharmacology, 20(2), 57–59. http://biological-psychiatry.eu/wp-content/uploads/2019/01/JBPP_2018_v20_No2_57-59.pdf.
Morris, S. B. (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. https://doi.org/10.1177/1094428106291059
Murphy, D., Shevlin, M., Pearson, E., Greenberg, N., Wessely, S., Busuttil, W., & Karatzias, T. (2020). A validation study of the International Trauma Questionnaire to assess post-traumatic stress disorder in treatment-seeking veterans. British Journal of Psychiatry, 216(3), 132–137. https://doi.org/10.1192/bjp.2020.9
Reyes, A. T., Bhatta, T. R., Muthukumar, V., & Gangozo, W. J. (2020). Testing the acceptability and initial efficacy of a smartphone-app mindfulness intervention for college student veterans with PTSD. Archives of Psychiatric Nursing, 34(2), 58–66. https://doi.org/10.1016/j.apnu.2020.02.004
Schulz, K. F., Altman, D. G., & Moher, D. (2011). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. International Journal of Surgery, 9(8), 672–677. https://doi.org/10.1016/j.ijsu.2011.09.004
Spitzer, R. L., Kroenke, K., Williams, J. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Truskauskaite-Kuneviciene, I., Kazlauskas, E., Ostreikaite-Jurevice, R., Brailovskaia, J., & Margraf, J. (2020). Positive mental health and adjustment following life-stressors among young adults. Current Psychology. https://doi.org/10.1007/s12144-020-00714-3
Valenstein-Mah, H., Simpson, T. L., Bowen, S., Enkema, M. C., Bird, E. R., In Cho, H., & Larimer, M. E. (2019). Feasibility pilot of a brief mindfulness intervention for college students with posttraumatic stress symptoms and problem drinking. Mindfulness, 10(7), 1255–1268. https://doi.org/10.1007/s12671-018-1077-y
Vlaescu, G., Alasjö, A., Miloff, A., Carlbring, P., & Andersson, G. (2016). Features and functionality of the Iterapi platform for internet-based psychological treatment. Internet Interventions, 6, 107–114. https://doi.org/10.1016/j.invent.2016.09.006
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). www.ptsd.va.gov
Wind, T. R., Rijkeboer, M., Andersson, G., & Riper, H. (2020). The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet Interventions, 20. https://doi.org/10.1016/j.invent.2020.100317
World Health Organization. (2018). International classification of diseases for mortality and morbidity statistics (11th Revision). https://icd.who.int/browse11/l-m/en
Author information
Authors and Affiliations
Contributions
AD: writing—first draft, data collection, data analysis, study design; ITK: writing—review and editing, data collection, data analysis, study design; JM: data collection; GA: writing—review and editing, supervision; EK: writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethical Approval
This study was approved by the Vilnius University Psychology Research Ethics Committee (Reference No. 27-02-2020/36). All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
All participants gave their informed consent for participation prior to filling the pre-test questionnaires. An information sheet that has been formally approved by the ethics committee was available to participants when they registered for the intervention. Participants were free to decide whether to participate in the study, and they could withdraw from the study at any time.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dumarkaite, A., Truskauskaite-Kuneviciene, I., Andersson, G. et al. Effects of Mindfulness-Based Internet Intervention on ICD-11 Posttraumatic Stress Disorder and Complex Posttraumatic Stress Disorder Symptoms: a Pilot Randomized Controlled Trial. Mindfulness 12, 2754–2766 (2021). https://doi.org/10.1007/s12671-021-01739-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-021-01739-w