Abstract
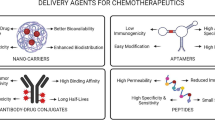
The global burden of cancer, which constitutes approximately one-sixth of all worldwide mortalities, poses a significant challenge for scientific researchers in their pursuit of effective therapeutic interventions. This discourse delves into the potential of idarubicin (IDA), an anthracycline antibiotic with pronounced lipophilicity, known for its accelerated nuclear sequestration, enhanced cellular permeability, and potent cytotoxicity. Despite IDA’s demonstrated effectiveness in combating a spectrum of cancers, its therapeutic utility is significantly hampered by the onset of deleterious side effects such as cardiotoxicity and myelosuppression. The manuscript provides an exhaustive analysis of novel methodologies that have been developed to circumvent the impediments associated with IDA delivery, encompassing lipid-based nanoparticles (NPs), polymeric nanocarriers, carbonaceous nanostructures, and inorganic NPs. It examines key parameters such as drug release, encapsulation efficacy, loading proficiency, zeta potential, along with in vivo and in vitro characterizations, offering a comprehensive assessment of the advancements in disparate delivery systems for IDA. Furthermore, the manuscript probes into co-delivery formulations of IDA in conjunction with other anti-cancer agents, underscoring their promising implications for future oncological therapy. The discourse also highlights the paucity of empirical research in this domain. The revelations gleaned from this review are anticipated to make a substantial contribution to the genesis of innovative strategies for future oncological treatment.











Similar content being viewed by others
Data Availability
No datasets were generated or analyzed during the current study.
Abbreviations
- 4-DMDR:
-
4-Demethoxydaunorubicin
- A549:
-
Lung carcinoma epithelial cells
- AF9:
-
5-[2,4-Bis(azanyl)pyrimidin-5-yl]oxy-2-methoxy-4-propan-2-yl-benzenesulfonamide
- AML:
-
Acute myeloid leukemia
- AuMPn:
-
Gold shell-coated magnetic polyester nanoparticles
- BILM:
-
Biodegradable idarubicin-loaded microsphere
- BuCy:
-
Busulphan and cyclophosphamide combination
- C57BL/6:
-
C57 black 6
- Caco-2:
-
Cancer coli-2
- CD:
-
β-Cyclodextrin
- CD8:
-
Cluster of differentiation 8
- CR:
-
Complete remission
- CNT:
-
Carbon nanotube
- DDC:
-
Dual drug conjugate
- DLS :
-
Dynamic light scattering
- DNA:
-
Deoxyribonucleic acid
- DNR:
-
Daunorubicin
- DSPC:
-
Distearoylphosphatidylcholine
- DPPC:
-
1,2-Dipalmitoyl-sn-glycero-3-phosphocholine
- DPV:
-
Differential pulse voltammetry
- DXR:
-
Doxorubicin
- D-pen:
-
D-penicillamine
- DFT:
-
Density functional theory
- DL:
-
Drug loading
- EDTA:
-
Ethylenediaminetetraacetic acid
- EE:
-
Encapsulation efficiency
- eNOS:
-
Endothelial nitric oxide synthase
- FA:
-
Folic acid
- GDY:
-
Graphydine
- GDYO:
-
Graphydine oxide
- GFP:
-
Green fluorescent protein
- h:
-
Hour
- HBR:
-
Hyperbranched resin
- HCC:
-
Hepatocellular carcinoma
- HER:
-
Human epidermal growth factor receptor
- HPLC:
-
High-performance liquid chromatography
- HT:
-
Hyperthermia
- HsAFr:
-
Horse spleen apoferritin
- IC50:
-
Half maximal inhibitory concentration
- IDA:
-
Idarubicin
- IgG4:
-
Immunoglobulin G4
- M:
-
Molar
- MCF-7:
-
Michigan Cancer Foundation-7
- MD:
-
Molecular dynamics
- MDR:
-
Multi-drug resistance
- MLL:
-
Mixed lineage leukemia
- MMA:
-
Methyl methacrylate
- MNP:
-
Magnetic nanoparticle
- m-PEG-PLGA:
-
Methoxy poly(ethylene glycol)-b-poly(L-lactide-co-glycolide)
- MPBH:
-
4-(4-N-maleimidophenyl)butyric acid hydrazide
- MPE:
-
Maleate-polyester
- mTHPP:
-
5,10,15,20-Tetrakis(meso-hydroxyphenyl)porphyrin
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- NCI-H460:
-
Human non-small cell lung carcinoma
- NP:
-
Nanoparticle
- NLCs:
-
Nanostructured lipid carriers
- NHL:
-
Non-Hodgkin’s lymphoma
- NT:
-
Normothermia
- PBS:
-
Phosphate buffered saline
- PD1:
-
Programmed cell death protein 1
- PEG :
-
Polyethylene glycol
- PGA:
-
Poly(glycolic acid)
- PSS:
-
Poly(styrene sulfonate)
- POPC:
-
Glycerolphospholipid 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine
- ptPVA:
-
Pteroic acid enhanced polyvinyl alcohol
- PDT:
-
Photodynamic therapy
- PTT:
-
Photothermal therapy
- PGA:
-
Poly (α) L-glutamic acid
- SCARA5:
-
Scavenger receptor class A member 5
- SDDS:
-
Smart drug delivery system
- SLNs:
-
Solid-lipid NPs
- TACE:
-
Transarterial chemoembolization
- TAM:
-
Tamoxifen
- TfR1:
-
Transferrin receptor protein 1
- TGI:
-
Tumor growth inhibition
- tBA:
-
Tert-butyl acrylate
- TEM:
-
Transmission electron microscopy
- UV:
-
Ultraviolet
- vdW:
-
Van der Waals
References
La Vecchia, S. and C. Sebastián. Metabolic pathways regulating colorectal cancer initiation and progression. in Seminars in cell & developmental biology. 2020. Elsevier.
Sathishkumar, K., et al. (2022). Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India. The Indian Journal of Medical Research, 156(4&5), 598–607.
Wang, W., et al. (2023). Curcumin in cancer therapy: Exploring molecular mechanisms and overcoming clinical challenges. Cancer Letters, 570, 216332.
Lazarus, E., & Bays, H. E. (2022). Cancer and obesity: An obesity medicine association (OMA) clinical practice statement (CPS) 2022. Obesity Pillars, 3, 100026.
Ali, H., et al. (2023). Emergence of nanohybrids in hormonal cancer-targeted therapy. Hormone related cancer mechanistic and nanomedicines: Challenges and prospects (pp. 71–88). Springer.
Bhattacharya, S., et al. (2023). Advances and challenges in thyroid cancer: The interplay of genetic modulators, targeted therapies, and AI-driven approaches. Life Sciences, 332, 122110.
Qi, K., Sun, B., Liu, S.-Y., & Zhang, M. (2023). Research progress on carbon materials in tumor photothermal therapy. Biomedicine & Pharmacotherapy, 165, 115070.
Lu, Y., Bai, X., & Pan, C. (2024). Impact of exercise interventions on quality of life and depression in lung cancer patients: A systematic review and meta-analysis. International Journal of Psychiatry in Medicine, 59(2), 199–217.
Cheville, A., Smith, S., Barksdale, T., & Asher, A. (2020). Cancer Rehabilitation. In Braddom's Physical Medicine and Rehabilitation (pp. 568–593.e7). Elsevier.
Mengarda, A. C., Iles, B., Longo, J. P. F., & de Moraes, J. (2023). Recent approaches in nanocarrier-based therapies for neglected tropical diseases. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 15(2), e1852.
Craig, M., et al. (2020). Engineering in medicine to address the challenge of cancer drug resistance: From micro-and nanotechnologies to computational and mathematical modeling. Chemical Reviews, 121(6), 3352–3389.
Fathi Karkan, S., Davaran, S., & Akbarzadeh, A. (2019). Cisplatin-loaded superparamagnetic nanoparticles modified with PCL-PEG copolymers as a treatment of A549 lung cancer cells. Nanomedicine Research Journal, 4(4), 209–219.
Kumar, M., et al. (2023). Micro and nano-carriers-based pulmonary drug delivery system: Their current updates, challenges, and limitations – A review. JCIS Open. 12. 100095.
Fatima Qizilbash, F., et al. (2023). Nanotechnology revolutionises breast cancer treatment: Harnessing lipid-based nanocarriers to combat cancer cells. Journal of Drug Targeting, 31(8), 794–816.
Rabiee, N., et al. (2020). Nanotechnology-assisted microfluidic systems: From bench to bedside. Nanomedicine, 16(3), 237–258.
Kong, X., et al. (2023). Advances of medical nanorobots for future cancer treatments. Journal of Hematology & Oncology, 16(1), 74.
Abdelkader, H., et al. (2021). Polymeric long-acting drug delivery systems (LADDS) for treatment of chronic diseases: Inserts, patches, wafers, and implants. Advanced Drug Delivery Reviews, 177, 113957.
Azizi, M., et al. (2023). Multifunctional plant virus nanoparticles: An emerging strategy for therapy of cancer. Wiley interdisciplinary reviews. Nanomedicine and Nanobiotechnology, 15(6), e1872.
Handa, M., et al. (2021). Recent advances in lipid-engineered multifunctional nanophytomedicines for cancer targeting. Journal of Controlled Release, 340, 48–59.
Wang, G., et al. (2020). Advances in nanotechnology-based strategies for the treatments of amyotrophic lateral sclerosis. Materials Today Bio, 6, 100055.
Delbreil, P., Rabanel, J.-M., Banquy, X., & Brambilla, D. (2022). Therapeutic nanotechnologies for Alzheimer’s disease: A critical analysis of recent trends and findings. Advanced Drug Delivery Reviews, 187, 114397.
Zhou, F., Peterson, T., Fan, Z., & Wang, S. (2023). The commonly used stabilizers for phytochemical-based nanoparticles: Stabilization effects, mechanisms, and applications. Nutrients, 15(18), 3881.
Fathi-Karkan, S., et al. (2023). Recent advancements in the targeted delivery of etoposide nanomedicine for cancer therapy: A comprehensive review. European Journal of Medicinal Chemistry, 259, 115676.
Fathi-Karkan, S., Ghavidel-Kenarsari, F., & Maleki-Baladi, R. (2022). Pullulan as promoting endothelialization capacity of electrospun PCL-PU scaffold. The International Journal of Artificial Organs, 45(12), 1013–1020.
Sahu, T., et al. (2021). Nanotechnology based drug delivery system: Current strategies and emerging therapeutic potential for medical science. Journal of Drug Delivery Science and Technology, 63, 102487.
Leso, V., et al. (2022). Exposure to antineoplastic drugs in occupational settings: A systematic review of biological monitoring data. International Journal of Environmental Research and Public Health, 19(6), 3737.
Abbas, A. A., & AlAzmi, A. A. M. (2019). Anthracycline-induced cardiac toxicity: A clinical review. Indian Journal of Medical and Paediatric Oncology, 40(04), 465–475.
Zheng, Z., et al. (2023). Idarubicin-loaded biodegradable microspheres enhance sensitivity to anti-PD1 immunotherapy in transcatheter arterial chemoembolization of hepatocellular carcinoma. Acta Biomaterialia, 157, 337–351.
Arcamone, F., et al. (1976). Synthesis and antitumor activity of 4-demethoxydaunorubicin, 4-demethoxy-7, 9-diepidaunorubicin, and their anomers. Cancer Treatment Reports, 60, 829–834.
Borchmann, P., Hübel, K., Schnell, R., & Engert, A. (1997). Idarubicin: A brief overview on pharmacology and clinical use. International Journal of Clinical Pharmacology and Therapeutics, 35(2), 80–83.
Gotzhein, F. (2021). Tracking clonal composition of stem cell transplants by genetic barcoding and implementation of a targeted barcoding procedure [Doctoral dissertation, University of Hamburg]. ediss.sub.hamburg.
Li, X., Xu, S., Tan, Y., & Chen, J. (2015). The effects of idarubicin versus other anthracyclines for induction therapy of patients with newly diagnosed leukaemia. The Cochrane Database of Systematic Reviews, (6), CD010432.
McGowan, J. V., et al. (2017). Anthracycline chemotherapy and cardiotoxicity. Cardiovascular Drugs and Therapy, 31, 63–75.
Das, S., et al. (2022). Aptamers functionalized biomolecular nano-vehicles for applications in cancer diagnostics & therapeutics. Applied NanoMedicine, 2(2), 360–360.
Tsuruo, T., Oh-Hara, T., Sudo, Y., & Naito, M. (1993). Antitumor activity of idarubicin, a derivative of daunorubicin, against drug sensitive and resistant P388 leukemia. Anticancer Research, 13(2), 357–361.
Kim, J. S., et al. (2022). Anthracycline derivatives inhibit cardiac CYP2J2. Journal of Inorganic Biochemistry, 229, 111722.
Jerjis, S., et al. (1998). Idarubicin to intensify the conditioning regimens of autologous bone marrow transplantation for patients with acute myeloid leukemia in first complete remission. Bone Marrow Transplantation, 22(1), 13–19.
Ravandi, F., et al. (2019). Idarubicin, cytarabine, and nivolumab in patients with newly diagnosed acute myeloid leukaemia or high-risk myelodysplastic syndrome: A single-arm, phase 2 study. The Lancet Haematology, 6(9), e480–e488.
Sherif, H. A., et al. (2021). Treatment outcome of doxorubicin versus idarubicin in adult acute myeloid leukemia. Leukemia Research Reports, 16, 100272.
Foroughi, M. M., & Jahani, S. (2022). Investigation of a high-sensitive electrochemical DNA biosensor for determination of idarubicin and studies of DNA-binding properties. Microchemical Journal, 179, 107546.
Rauf, S., et al. (2005). Electrochemical approach of anticancer drugs–DNA interaction. Journal of Pharmaceutical and Biomedical Analysis, 37(2), 205–217.
Lachatre, F., et al. (2000). Simultaneous determination of four anthracyclines and three metabolites in human serum by liquid chromatography–electrospray mass spectrometry. Journal of Chromatography B: Biomedical Sciences and Applications, 738(2), 281–291.
Hu, Q., Hu, G., Zhou, T., & Fang, Y. (2003). Determination of dissociation constants of anthrocycline by capillary zone electrophoresis with amperometric detection. Journal of Pharmaceutical and Biomedical Analysis, 31(4), 679–684.
Kuhlmann, O., Hofmann, S., & Weiss, M. (1999). Determination of idarubicin and idarubicinol in rat plasma using reversed-phase high-performance liquid chromatography and fluorescence detection. Journal of Chromatography B: Biomedical Sciences and Applications, 728(2), 279–282.
Badea, I., et al. (2005). A HPLC method for the simultaneous determination of seven anthracyclines. Journal of Pharmaceutical and Biomedical Analysis, 39(1–2), 305–309.
Kurbanoglu, S., et al. (2013). Electrochemical investigations of the anticancer drug idarubicin using multiwalled carbon nanotubes modified glassy carbon and pyrolytic graphite electrodes. Electroanalysis, 25(6), 1473–1482.
Li, W., Jiang, Y., & Lu, J. (2023). Nanotechnology-enabled immunogenic cell death for improved cancer immunotherapy. International Journal of Pharmaceutics, 634, 122655.
Behravan, N., et al. (2022). Lipid-based nanoparticulate delivery systems for HER2-positive breast cancer immunotherapy. Life Sciences, 291, 120294.
Liang, B., et al. (2019). Idarubicin-loaded methoxy poly(ethylene glycol)-b-poly(l-lactide-co-glycolide) nanoparticles for enhancing cellular uptake and promoting antileukemia activity. International Journal of Nanomedicine, 14, 543–556.
Najafi, F., Pourali, S., & Kamran, A. (2021). Comparison of thermodynamic functions of idarubicin cancer drug interaction with carbon nanotube: QM/MM studies. International Journal of New Chemistry, 8(1), 30–40.
Alavi, M., & Varma, R. S. (2020). Overview of novel strategies for the delivery of anthracyclines to cancer cells by liposomal and polymeric nanoformulations. International Journal of Biological Macromolecules, 164, 2197–2203.
Ashrafizadeh, M., et al. (2021). Hyaluronic acid-based nanoplatforms for doxorubicin: A review of stimuli-responsive carriers, co-delivery and resistance suppression. Carbohydrate Polymers, 272, 118491.
Tapeinos, C., Battaglini, M., & Ciofani, G. (2017). Advances in the design of solid lipid nanoparticles and nanostructured lipid carriers for targeting brain diseases. Journal of Controlled Release, 264, 306–332.
Yingchoncharoen, P., Kalinowski, D. S., & Richardson, D. R. (2016). Lipid-based drug delivery systems in cancer therapy: What is available and what is yet to come. Pharmacological Reviews, 68(3), 701–787.
Sheoran, S., Arora, S., Samsonraj, R., & Govindaiah, P. (2022). Lipid-based nanoparticles for treatment of cancer. Heliyon, 8(5), e09403.
Mitchell, M. J., et al. (2021). Engineering precision nanoparticles for drug delivery. Nature Reviews Drug Discovery, 20(2), 101–124.
Xu, Q., et al. (2023). Tumor microenvironment-regulating nanomedicine design to fight multi-drug resistant tumors. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 15(1), e1842.
Sarangi, B., et al. (2019). Solid lipid nanoparticles: A potential approach for drug delivery system. Nanoscience & Nanotechnology-Asia, 9(2), 142–156.
Zara, G. P., et al. (2002). Pharmacokinetics and tissue distribution of idarubicin-loaded solid lipid nanoparticles after duodenal administration to rats. Journal of Pharmaceutical Sciences, 91(5), 1324–1333.
Sermsappasuk, P., Hrynyk, R., Gubernator, J., & Weiss, M. (2008). Reduced uptake of liposomal idarubicin in the perfused rat heart. Anti-cancer Drugs, 19(7), 729–732.
Iqbal, N., & Iqbal, N. (2014). Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Molecular Biology International, 2014, 852748.
Amin, M., et al. (2018). Specific delivery of idarubicin to HER2-positive breast cancerous cell line by trastuzumab-conjugated liposomes. Journal of Drug Delivery Science and Technology, 47, 209–214.
Ma, P., et al. (2009). Development of idarubicin and doxorubicin solid lipid nanoparticles to overcome Pgp-mediated multiple drug resistance in leukemia. Journal of Biomedical Nanotechnology, 5(2), 151–161.
Tang, Q., et al. (2018). Stimuli responsive nanoparticles for controlled anti-cancer drug release. Current Medicinal Chemistry, 25(16), 1837–1866.
Lu, T., et al. (2015). Formulation and optimization of idarubicin thermosensitive liposomes provides ultrafast triggered release at mild hyperthermia and improves tumor response. Journal of Controlled Release, 220, 425–437.
Wang, Y., Chen, L., Ding, Y., & Yan, W. (2012). Oxidized phospholipid based pH sensitive micelles for delivery of anthracyclines to resistant leukemia cells in vitro. International Journal of Pharmaceutics, 422(1–2), 409–417.
Dos Santos, N., et al. (2005). Substantial increases in idarubicin plasma concentration by liposome encapsulation mediates improved antitumor activity. Journal of Controlled Release, 105(1–2), 89–105.
Gubernator, J., et al. (2010). The encapsulation of idarubicin within liposomes using the novel EDTA ion gradient method ensures improved drug retention in vitro and in vivo. Journal of Controlled Release, 146(1), 68–75.
Dos Santos, N., et al. (2002). Improved retention of idarubicin after intravenous injection obtained for cholesterol-free liposomes. Biochimica et Biophysica Acta (BBA)-Biomembranes, 1561(2), 188–201.
Caro, C., et al. (2022). Nanomaterials loaded with Quercetin as an advanced tool for cancer treatment. Journal of Drug Delivery Science and Technology, 78, 103938.
Cheng, R., et al. (2013). Dual and multi-stimuli responsive polymeric nanoparticles for programmed site-specific drug delivery. Biomaterials, 34(14), 3647–3657.
Prabhu, R. H., Patravale, V. B., & Joshi, M. D. (2015). Polymeric nanoparticles for targeted treatment in oncology: current insights. International Journal of Nanomedicine, 10, 1001–1018.
Abad, F., et al. (2023). Chitosan-Carbon nanotube Composite: An approach for controlled release of Quercetin, Modified with carboxymethyl Cellulose, for potential Anti-Cancer therapy. Inorganic Chemistry Communications, 158, 111621.
Jain, R., et al. (2011). Enhanced cellular delivery of idarubicin by surface modification of propyl starch nanoparticles employing pteroic acid conjugated polyvinyl alcohol. International Journal of Pharmaceutics, 420(1), 147–155.
Güç, E., Gündüz, G., & Gündüz, U. (2010). Fatty acid based hyperbranched polymeric nanoparticles for hydrophobic drug delivery. Drug Development and Industrial Pharmacy, 36(10), 1139–1148.
Minotti, G., et al. (2004). Anthracyclines: Molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacological reviews, 56(2), 185–229.
Zhang, Y., Li, J., & Pu, K. (2022). Recent advances in dual- and multi-responsive nanomedicines for precision cancer therapy. Biomaterials, 291, 121906.
Das, B. C., et al. (2023). Stimuli-responsive boron-based materials in drug delivery. International Journal of Molecular Sciences, 24(3), 2757.
Wadhwa, S., & Mumper, R. J. (2012). Polypeptide conjugates of d-penicillamine and idarubicin for anticancer therapy. Journal of Controlled Release, 158(2), 215–223.
Blaudszun, A.-R., et al. (2014). Polyester-idarubicin nanoparticles and a polymer-photosensitizer complex as potential drug formulations for cell-mediated drug delivery. International Journal of Pharmaceutics, 474(1–2), 70–79.
Nafee, N., et al. (2015). Cyclodextrin-based star polymers as a versatile platform for nanochemotherapeutics: Enhanced entrapment and uptake of idarubicin. Colloids and Surfaces B: Biointerfaces, 129, 30–38.
Gunduz, U., et al. (2014). Idarubicin-loaded folic acid conjugated magnetic nanoparticles as a targetable drug delivery system for breast cancer. Biomedicine & Pharmacotherapy, 68(6), 729–736.
Rafipour, R., Mousavi, A., & Mansouri, K. (2022). Apoferritin nanocages for targeted delivery of idarubicin against breast cancer cells. Biotechnology and Applied Biochemistry, 69(3), 1061–1067.
Tang, L., et al. (2021). Insights on functionalized carbon nanotubes for cancer theranostics. Journal of Nanobiotechnology, 19, 1–28.
Dehdashtian, S., Behbahanian, N., Mohammadi Taherzadeh, K., & Hashemi, B. (2019). Development of electrochemical sensor based on multiwall carbon nanotube for determination of anticancer drug idarubicin in biological samples. Advances in Nanochemistry, 1(1), 22–28.
Chandra, K., Dutta, S., Kolya, H., & Kang, C.-W. (2023). Structural aspect of hydroxyethyl-starch–anticancer-drug-conjugates as state-of-the-art drug carriers. Scientia Pharmaceutica, 91(3), 32.
Matyszewska, D. (2020). The influence of charge and lipophilicity of daunorubicin and idarubicin on their penetration of model biological membranes–Langmuir monolayer and electrochemical studies. Biochimica et Biophysica Acta (BBA)-Biomembranes, 1862(2), 183104.
Shahabi, M., & Raissi, H. (2021). The transport of idarubicin therapeutic agent using a novel graphene sheet as a drug delivery platform through a biomembrane. Journal of Molecular Liquids, 323, 115050.
Lu, T., et al. (2021). Externally triggered smart drug delivery system encapsulating idarubicin shows superior kinetics and enhances tumoral drug uptake and response. Theranostics, 11(12), 5700.
Shahabi, M., & Raissi, H. (2020). Two dimensional porous frameworks of graphyne family as therapeutic delivery vehicles for Idarubicin biomolecule in silico: Density functional theory and molecular dynamics simulation. Journal of Molecular Liquids, 319, 114334.
Li, C., et al. (2022). Molecular recognition-driven supramolecular nanoassembly of a hydrophobic uracil prodrug and hydrophilic cytarabine for precise combination treatment of solid and non-solid tumors. Nanoscale Horizons, 7(2), 235–245.
Pérez-Ruiz, T., Martínez-Lozano, C., Sanz, A., & Bravo, E. (2001). Simultaneous determination of doxorubicin, daunorubicin, and idarubicin by capillary electrophoresis with laser-induced fluorescence detection. Electrophoresis, 22(1), 134–138.
Iland, H. J., et al. (2012). All-trans-retinoic acid, idarubicin, and IV arsenic trioxide as initial therapy in acute promyelocytic leukemia (APML4). Blood, The Journal of the American Society of Hematology, 120(8), 1570–1580.
Iland, H., et al. (2012). Results of the APML3 trial incorporating all-trans-retinoic acid and idarubicin in both induction and consolidation as initial therapy for patients with acute promyelocytic leukemia. Haematologica, 97(2), 227.
Guiu, B., et al. (2015). Idarubicin-loaded ONCOZENE drug-eluting embolic agents for chemoembolization of hepatocellular carcinoma: In vitro loading and release and in vivo pharmacokinetics. Journal of Vascular and Interventional Radiology, 26(2), 262–270.
Meng, R. (2016). Multifunctional gold nanoshell-coated magnetic nanoparticles: preparation, characterization, two-photon optical properties and drug release exploration. Chinese Pharmaceutical Journal, 24, 1394–1404.
Ulusal, H., et al. (2022). Attachment of idarubicin to glutaraldehyde-coated magnetic nanoparticle and investigation of its effect in HL-60 cell line. International Journal of Chemistry and Technology, 6(2), 154–163.
Eftekhari, R. B., et al. (2019). Co-delivery nanosystems for cancer treatment: A review. Pharmaceutical Nanotechnology, 7(2), 90–112.
Li, Y., Thambi, T., & Lee, D. S. (2018). Co-delivery of drugs and genes using polymeric nanoparticles for synergistic cancer therapeutic effects. Advanced Healthcare Materials, 7(1), 1700886.
Aryal, S., Hu, C. M. J., & Zhang, L. (2010). Combinatorial drug conjugation enables nanoparticle dual-drug delivery. Small, 6(13), 1442–1448.
Wang, D., et al. (2022). Idarubicin/mithramycin-acridine orange combination drugs co-loaded by DNA nanostructures: Different effects of intercalation and groove binding on drug release and cytotoxicity. Journal of Molecular Liquids, 355, 118947.
Weng, S., et al. (2023). Idarubicin and IR780 co-loaded PEG-b-PTMC nanoparticle for non-Hodgkin’s lymphoma therapy by photothermal/photodynamic strategy. Materials & Design, 230, 112008.
Nia, H. T., Munn, L. L., & Jain, R. K. (2020). Physical traits of cancer. Science, 370(6516), eaaz0868.
Funding
Abbas Rahdar thanks from University of Zabol for funding (UOZ-GR-8906). The authors (Sadanand Pandey) express profound gratitude to Shoolini University for their invaluable support, which played a pivotal role in facilitating the completion of work.
Author information
Authors and Affiliations
Contributions
F.S., Y. J, H. A., M.P.: investigation, data curation. P.Z., M. A.: writing, review, and editing. A. R., S. F-k., S. P: validation, writing, review, and editing. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Safari, F., Jalalian, Y., Abdouss, H. et al. Harnessing Nanotechnology for Idarubicin Delivery in Cancer Therapy: Current Approaches and Future Perspectives. BioNanoSci. (2024). https://doi.org/10.1007/s12668-024-01376-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12668-024-01376-2