Abstract
Background and Objectives
Achalasia has several treatment modalities. We aim to compare the efficacy and safety of laparoscopic Heller myotomy (LHM) with those of pneumatic dilatation (PD) in adult patients suffering from achalasia.
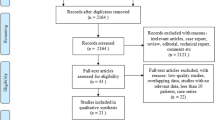
Methods
We searched Cochrane CENTRAL, PubMed, Web of Science, SCOPUS and Embase for related clinical trials about patients suffering from achalasia. The quality appraisal and assessment of risk of bias were conducted with GRADE and Cochrane’s risk of bias tool, respectively. Homogeneous and heterogeneous data was analyzed under fixed and random-effects models, respectively.
Results
The pooled analysis of 10 studies showed that PD was associated with a higher rate of remission at three months, one year, three years and five years (RR = 1.25 [1.09, 1.42] (p = 0.001); RR = 1.13 [1.05, 1.20] (p = 0.0004); RR = 1.48 [1.19, 1.82] (p = 0.0003); RR = 1.49 [1.18, 1.89] (p = 0.001)), respectively. LHM was associated with lower number of cases suffering from adverse events, dysphagia and relapses (RR = 0.50 [0.25, 0.98] (p = 0.04); RR = 0.33 [0.16, 0.71] (p = 0.004); RR = 0.38 [0.15, 0.97] (p = 0.04)), respectively. There is no significant difference between both groups regarding the lower esophageal pressure, perforations, remission rate at two years, Eckardt score after one year and reflux.
Conclusion
PD had higher remission rates than LHM at three months, one year and three years, but not at two years or five years. More research is needed to determine whether PD has a significant advantage over LHM in terms of long-term remission rates.
Graphical abstract







Similar content being viewed by others
Data availability
Data is available upon contacting the corresponding author.
References
Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–14. https://doi.org/10.1111/j.1572-0241.2005.41775.
Ott DJ. Motility disorders of the esophagus. Radiol Clin North Am. 1994;32:1117–34.
Shaker R, Staff D. Esophageal disorders in the elderly. Gastroenterol Clin North Am. 2001;30:335–61, vii−viii. https://doi.org/10.1016/s0889-8553(05)70185-0.
Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015 May 12;313:1841–52. https://doi.org/10.1001/jama.2015.2996
Hirano I, Tatum RP, Shi G, Sang Q, Joehl RJ, Kahrilas PJ. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology. 2001;120:789–98. https://doi.org/10.1053/gast.2001.22539.
Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut. 1992;33:1011–5. https://doi.org/10.1136/gut.33.8.1011.
Stefanidis D, Richardson W, Farrell TM, et al. SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc. 2012;26:296–311. https://doi.org/10.1007/s00464-011-2017-2.
Karamanolis G, Sgouros S, Karatzias G, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol. 2005;100:270–4. https://doi.org/10.1111/j.1572-0241.2005.40093.
Hulselmans M, Vanuytsel T, Degreef T, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol. 2010;8:30–5. https://doi.org/10.1016/j.cgh.2009.09.020.
Von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411–7. https://doi.org/10.1038/ajg.2011.388.
Borhan-Manesh F, Kaviani MJ, Taghavi AR. The efficacy of balloon dilation in achalasia is the result of stretching of the lower esophageal sphincter, not muscular disruption. Dis Esophagus. 2016;29:262–6. https://doi.org/10.1111/dote.12314.
Kostic S, Johnsson E, Kjellin A, et al. Health economic evaluation of therapeutic strategies in patients with idiopathic achalasia: results of a randomized trial comparing pneumatic dilatation with laparoscopic cardiomyotomy. Surg Endosc. 2007;21:1184–9. https://doi.org/10.1007/s00464-007-9310-0.
Zaninotto G, Costantini M, Portale G, et al. Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg. 2002;235:186–92. https://doi.org/10.1097/00000658-200202000-00005.
Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg. 2003;138:490–5; discussion 495–7. https://doi.org/10.1001/archsurg.138.5.490.
Perrone JM, Frisella MM, Desai KM, Soper NJ. Results of laparoscopic Heller-Toupet operation for achalasia. Surg Endosc. 2004;18:1565–71. https://doi.org/10.1007/s00464-004-8912-z.
Rossetti G, Brusciano L, Amato G, et al. A total fundoplication is not an obstacle to esophageal emptying after Heller myotomy for achalasia: results of a long-term follow up. Ann Surg. 2005;241:614–21. https://doi.org/10.1097/01.sla.0000157271.69192.96.
Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H. Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol. 2006;101:692–7. https://doi.org/10.1111/j.1572-0241.2006.00385.
Vela MF, Richter JE, Khandwala F, et al. The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol. 2006;4:580–7. https://doi.org/10.1016/s1542-3565(05)00986-9.
Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–4. https://doi.org/10.1055/s-2007-966764.
Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91:213–227.e6. https://doi.org/10.1016/j.gie.2019.04.231.
Lois AW, Oelschlager BK, Wright AS, Templeton AW, Flum DR, Farjah F. Use and safety of per-oral endoscopic myotomy for achalasia in the US. JAMA Surg. 2022;157:490–7. https://doi.org/10.1001/jamasurg.2022.0807.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
Katz A. Microsoft Excel 2010. Style (DeKalb, IL). 2010.
Lebowitz F. Endnote. Aperture. 2021. https://endnote.com
Munder T, Barth J. Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychother Res. 2018;28:347–55. https://doi.org/10.1080/10503307.2017.1411628.
Borges AA, de Oliveira Lemme EM, Abrahao LJ, et al. Pneumatic dilation versus laparoscopic Heller myotomy for the treatment of achalasia: variables related to a good response. Dis Esophagus. 2014;27:18–23.
Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. https://doi.org/10.1002/14651858.ED000142.
Moonen A, Annese V, Belmans A, et al. Long-term results of the European Achalasia Trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut. 2016;65:732–9.
Kostic S, Kjellin A, Ruth M, et al. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia: results of a randomized controlled trial. World J Surg. 2007;31:470–8.
Hamdy E, El Nakeeb A, El Hanfy E, et al. Comparative study between laparoscopic Heller myotomy versus pneumatic dilatation for treatment of early achalasia: a prospective randomized study. J Laparoendosc Adv Surg Tech. 2015;25:460–4.
Chrystoja CC, Darling GE, Diamant NE, et al. Achalasia-specific quality of life after pneumatic dilation or laparoscopic Heller myotomy with partial fundoplication: a multicenter, randomized clinical trial. Am J Gastroenterol. 2016;111:1536–45.https://doi.org/10.1038/ajg.2016.402.
Wu JCY. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. J Neurogastroenterol Motil. 2011;17:324–6.
Tabola R, Grabowski K, Lewandowski A, Augof K, Markocka-Maczka K. Achalasia - balloon dilation or surgery? Med Sci Monit. 2013;19:1089–94.
Sediqi E, Tsoposidis A, Wallenius V, et al. Laparoscopic Heller myotomy or pneumatic dilatation in achalasia: results of a prospective, randomized study with at least a decade of follow-up. Surg Endosc. 2021;35:1618–25. https://doi.org/10.1007/s00464-020-07541-4.
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U. Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg. 2015;39:713–20.
Novais PA, Lemme EMO. 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther. 2010;32:1257–65.
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–16. https://doi.org/10.1056/NEJMoa1010502.
Illés A, Farkas N, Hegyi P, et al. Is Heller myotomy better than balloon dilation? A meta-analysis. J Gastrointest Liver Dis. 2017;26:121–7.
Cheng J-W, Li Y, Xing W-Q, Lv H-W, Wang H-R. Laparoscopic Heller myotomy is not superior to pneumatic dilation in the management of primary achalasia. Medicine (Baltimore). 2017;96:e5525.
Tan S, Zhong C, Ren Y, et al. Efficacy and safety of peroral endoscopic myotomy in achalasia patients with failed previous intervention: a systematic review and meta-analysis. Gut Liver. 2021;15:153–67.
Liu ZQ, Li QL, Chen WF, et al. The effect of prior treatment on clinical outcomes in patients with achalasia undergoing peroral endoscopic myotomy. Endoscopy. 2019;51:307–16.
Author information
Authors and Affiliations
Contributions
AM: conceptualization, methodology, formal analysis, writing original draft, methodology and review and editing. SQ: formal analysis, methodology and writing original draft. AN: methodology, writing, editing and data curation. MIM: methodology, writing original manuscript and review and editing. DGA: supervision, writing and editing the manuscript
Corresponding author
Ethics declarations
Conflict of interest
AM, SQ, AN, MIM and DGA declare no competing interests.
Human ethics
No applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent to publish the manuscript and the study results.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Malik, A., Qureshi, S., Nadir, A. et al. Efficacy and safety of laparoscopic Heller’s myotomy versus pneumatic dilatation for achalasia: A systematic review and meta-analysis of randomized controlled trials. Indian J Gastroenterol (2024). https://doi.org/10.1007/s12664-023-01497-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12664-023-01497-8