Abstract
Background and Aims
While dengue infection is common in India, there is scarce information on dengue hepatitis. The aim of this study was to analyze the incidence, spectrum and outcome of dengue hepatitis.
Methods
We retrospectively analyzed consecutive patients, who had hepatitis among those with dengue infection admitted to two tertiary care hospitals in western India from January 2016 to March 2021. Diagnosis of dengue infection was made by serology. Dengue hepatitis was diagnosed and the severity of dengue was categorized by standard criteria.
Results
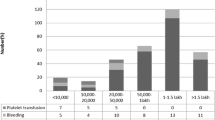
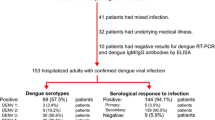
Of 1664 patients admitted with dengue fever during the study period, 199 patients had hepatitis (i.e. incidence of dengue hepatitis was 11.9%). Of the 199 dengue hepatitis patients (age: 29 [13 – 80] years, median [range], 67% males), 100 patients (50%) had severe dengue, 73 (36%) had severe dengue hepatitis, 32 (16%) had dengue shock syndrome and eight (4%) had acute liver failure. Forty-five patients (23%) had acute lung injury and 32 (16%) had acute kidney injury. The dengue hepatitis patients were treated with standard medical care, including vital organ support, as needed—166 (83%) patients survived, while 33 patients (17%) died (cause of death: multi-organ failure: 24 patients, septic shock: nine patients). The presence of shock independently predicted mortality (odds ratio 6.4, 95% confidence interval: 1.2 – 34). Among patients with dengue hepatitis, mortality rate was higher in those with severe dengue (23%), dengue shock syndrome (47%), severe dengue hepatitis (24%) and acute liver failure (38%).
Conclusion
In this large series of hospitalized patients with dengue infection, the incidence of dengue hepatitis was 11.9%. Among 199 dengue hepatitis, 17% died; multi-organ failure was the commonest cause for death and death rate was higher in patients with more severe disease. The presence of shock at presentation independently predicted mortality.

Similar content being viewed by others
Data availability
Supporting data will be made available as and when required.
References
Souza LJ de, Alves JG, Nogueira RMR, et al. Aminotransferase changes and acute hepatitis in patients with dengue fever: analysis of 1,585 cases. Braz J Infect Dis. 2004;8:156–63.
Kumar A, Arora A. Non-viral infective and non-infective nimics of hepatitis. In: Anand AC, ed. Viral Hepatitis in Indian Subcontinent. . 1st ed. Indian College of Physicians, Mumbai: India; 2017. pp. 91–118.
Kumar A, Arora A. Liver involvement in common febrile illnesses. Curr Med Res Pract. 2018;8:170–6.
Kulkarni AV, Choudhury AK, Premkumar M, Jain P, Gupta E, Sarin SK. Spectrum, manifestations and outcomes of dengue infection in individuals with and without liver disease. J Clin Transl Hepatol. 2019;7:106–11.
Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control: New Edition [Internet]. Geneva: World Health Organization; 2009. Available from: http://www.ncbi.nlm.nih.gov/books/NBK143157/. Accessed 30 November 2022
O’Grady JG, Schalm SW, Williams R. Acute liver failure: redefining the syndromes. Lancet. 1993;342:273–5.
Devarbhavi H, Ganga D, Menon M, Kothari K, Singh R. Dengue hepatitis with acute liver failure: Clinical, biochemical, histopathological characteristics and predictors of outcome. J Gastroenterol Hepatol. 2020;35:1223–8.
Kuo CH, Tai DI, Chang-Chien CS, Lan CK, Chiou SS, Liaw YF. Liver biochemical tests and dengue fever. Am J Trop Med Hyg. 1992;47:265–70.
Nath P, Agrawal DK, Mehrotra RM. Ultrastructural changes in skeletal muscles in dengue virus-infected mice. J Pathol. 1982;136:301–5.
Kalita J, Misra UK, Mahadevan A, Shankar SK. Acute pure motor quadriplegia: is it dengue myositis? Electromyogr Clin Neurophysiol. 2005;45:357–61.
Seneviratne SL, Malavige GN, de Silva HJ. Pathogenesis of liver involvement during dengue viral infections. Trans R Soc Trop Med Hyg. 2006;100:608–14.
Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC. Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoS Negl Trop Dis. 2012;6: e1676.
Chongsrisawat V, Hutagalung Y, Poovorawan Y. Liver function test results and outcomes in children with acute liver failure due to dengue infection. Southeast Asian J Trop Med Public Health. 2009;40:47–53.
Deepak NA, Patel ND. Differential diagnosis of acute liver failure in India. Ann Hepatol. 2006;5:150–6.
Tan S-S, Bujang MA. The clinical features and outcomes of acute liver failure associated with dengue infection in adults: a case series. Braz J Infect Dis. 2013;17:164–9.
Bhushan D, Kumar R. Clinical profile, hepatic dysfunctions, and outcome of dengue patients in a tertiary care hospital of eastern India. J Assoc Physicians India. 2018;66:52–4.
Sangkaew S, Ming D, Boonyasiri A, et al. Risk predictors of progression to severe disease during the febrile phase of dengue: a systematic review and meta-analysis. Lancet Infect Dis. 2021;21:1014–26.
Fahmy M, Young SP. Modulation of iron metabolism in monocyte cell line U937 by inflammatory cytokines: changes in transferrin uptake, iron handling and ferritin mRNA. Biochem J. 1993;296 Pt 1:175–81.
Ludwiczek S, Aigner E, Theurl I, Weiss G. Cytokine-mediated regulation of iron transport in human monocytic cells. Blood. 2003;101:4148–54.
Tran TN, Eubanks SK, Schaffer KJ, Zhou CY, Linder MC. Secretion of ferritin by rat hepatoma cells and its regulation by inflammatory cytokines and iron. Blood. 1997;90:4979–86.
Petchiappan V, Hussain TM, Thangavelu S. Can serum ferritin levels predict the severity of dengue early?: an observational study. Int J Res Med Sci. 2019;7:876–81.
Suresh SC, Hanumanthaiah R, Ramakrishna C, et al. Serum ferritin as a prognostic indicator in adult dengue patients. Am J Trop Med Hyg. 2021;104:1072–8.
Soundravally R, Agieshkumar B, Daisy M, Sherin J, Cleetus CC. Ferritin levels predict severe dengue. Infection. 2015;43:13–9.
Goel R, Eapen CE. Recognizing dysfunctional innate and adaptive immune responses contributing to liver damage in patients with cirrhosis. J Clin Exp Hepatol. 2022;12:993–1002.
De Koninck A-S, Dierick J, Steyaert S, Taelman P. Hemophagocytic lymphohistiocytosis and dengue infection: rare case report. Acta Clin Belg. 2014;69:210–3.
Yoshifuji K, Oshina T, Sonokawa S, et al. Domestic dengue infection with hemophagocytic lymphohistiocytosis successfully treated by early steroid therapy. Rinsho Ketsueki. 2016;57:864–8.
Eapen CE, Nair SC. Potential danger of isolated platelet transfusion in patients with dengue infection. Indian J Med Res. 2017;145:158–60.
Zachariah U, Kumar SE, Alexander V, Patel L, Goel A, Eapen CE. Low-volume plasma exchange and low-dose steroid to treat severe liver injury. Gastroenterol Hepatol Endosc Pract. 2021;1:47–54.
Alexander V, Zachariah U, Goel A, et al. Low-volume plasma exchange and low-dose steroid to treat secondary hemophagocytic lymphohistiocytosis: A potential treatment for severe COVID-19? Curr Med Issues. 2020;18:77–82.
Author information
Authors and Affiliations
Contributions
Ritesh Prajapati: Study idea, concept and design, data extraction, interpretation of data, drafting of manuscript. Rajiv Mehta, Mayank Kabrawala, Subhash Nandwani: Study idea, concept and design, interpretation of data. Nisharg Patel, Mohit Sethia, Kamlesh Magnani, Raj Tandel: data extraction, interpretation of data, drafting of manuscript. Ashish Kumar: interpretation of data, drafting of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
RP, RM, MK, SN, NP, MS, KM, RT and AK state no competing interest.
Ethics statement
The study was performed conforming to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Ethical approval and Consent to participate
Approval from the institutional review board (4 November 2021, Surat Institute of Digestive Sciences Ethics Committee) was taken.
Consent for publication
The authors give consent for publication.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prajapati, R., Mehta, R., Kabrawala, M. et al. Dengue hepatitis: Incidence, spectrum and outcome. Indian J Gastroenterol 42, 355–360 (2023). https://doi.org/10.1007/s12664-023-01405-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-023-01405-0