Abstract
Background/Purpose
Non-alcoholic fatty liver disease (NAFLD) patients are at increased risk of liver-related as well as cardiovascular mortality, including diabetes, coronary heart disease, and stroke, independently of traditional cardiovascular risk factors and metabolic syndrome. The aim of this study was to find out the predictive impact of hepatorenal index (HRI) in the detection of impaired glucose metabolism in asymptomatic NAFLD patients.
Methods
B-mode ultrasound examinations were performed and ultrasound images from all 89 NAFLD patients aged 50.8 ± 10.1 years were analyzed by echogenicity analyzing software and HRI was acquired, and appropriate laboratory tests for liver, glucose, and lipid metabolism were undertaken.
Results
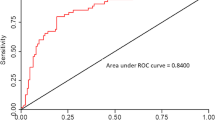
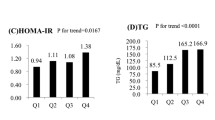
The mean HRI was 1.345 ± 0.189. 23.59% of patients had mild NAFLD (HRI = 1.167 ± 0.041), 64.04% moderate (HRI = 1.401 ± 0.102), and 12.36% patients severe NAFLD (HRI = 1.802 ± 0.098). Impaired glucose metabolism was present in 48.31% of patients. A positive correlation was present between HRI and impaired glucose metabolism (r = 0.335, p = 0.001). The coefficients of determinations R2 for linear regression for HRI and glycated hemoglobin (HbA1c) and oral glucose tolerance test (GTT) were 0.05841 and 0.07498, respectively. The cutoff values for HRI in the detection of diabetes and prediabetes, and prediabetes only, were 1.4 and 1.38, respectively. In logistic regression, the β coefficients for oral GTT, HbA1c, or HRI were 0.62042 (p = 0.0002), 2.18036 (p = 0.0033), and 2.36986 (p = 0.012). The hazard ratio (HR) coefficients (exp [b]) for HRI, HbA1c, and oral GTT sorted according to their HR strength were 10.6958, 8.8494, and 1.8597, respectively.
Conclusion
Ultrasonographically acquired HRI has a significant predictive impact on the detection of prediabetes and diabetes in patients with NAFLD.






Similar content being viewed by others
References
Zelber-Sagi S, Webb M, Assy N, et al. Comparison of fatty liver index with noninvasive methods for steatosis detection and quantification. World J Gastroenterol. 2013;19:57–64.
Kanwar P, Kowdley KV. The metabolic syndrome and its influence on nonalcoholic steatohepatitis. Clin Liver Dis. 2016;20:225–43.
Patil R, Sood GK. Non-alcoholic fatty liver disease and cardiovascular risk. World J Gastrointest Pathophysiol. 2017;8:51–8.
Kotronen A, Yki-Järvinen H. Fatty liver: a novel component of the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28:27–38.
Pang Q, Zhang J-Y, Song S-D, et al. Central obesity and nonalcoholic fatty liver disease risk after adjusting for body mass index. World J Gastroenterol. 2015;21:1650–62.
Straub BK, Schirmacher P. Pathology and biopsy assessment of non-alcoholic fatty liver disease. Dig Dis. 2010;28:197–202.
Raszeja-Wyszomirska J, Lawniczak M, Marlicz W, Miezyńska-Kurtycz J, Milkiewicz P. Non-alcoholic fatty liver disease--new view. Pol Merkur Lekarski. 2008;24:568–71.
Riley TR, Bruno MA. Sonographic measurement of the thickness of subcutaneous tissues in nonalcoholic fatty liver disease versus other chronic liver diseases. J Clin Ultrasound. 2005;33:439–41.
Khov N, Sharma A, Riley TR. Bedside ultrasound in the diagnosis of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:6821–5.
Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez R, McCullough AJ. Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol. 2009;51:1061–7.
Marshall RH, Eissa M, Bluth EI, Gulotta PM, Davis NK. Hepatorenal index as an accurate, simple, and effective tool in screening for steatosis. AJR Am Roentgenol. 2012;199:997–1002.
Marchesini G, Brizi M, Bianchi G, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–50.
Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–31.
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31.
Amiri Dash Atan N, Koushki M, Motedayen M, et al. Type 2 diabetes mellitus and non-alcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterol Hepatol Bed Bench. 2017;10 Suppl 1:S1–7.
Leite NC, Villela-Nogueira CA, Cardoso CR, Salles GF. Non-alcoholic fatty liver disease and diabetes: from physiopathological interplay to diagnosis and treatment. World J Gastroenterol. 2014;20:8377–92.
Isaksen VT, Larsen MA, Goll R, Florholmen JR, Paulssen EJ. Hepatic steatosis, detected by hepatorenal index in ultrasonography, as a predictor of insulin resistance in obese subjects. BMC Obes. 2016;3:39.
Webb M, Yeshua H, Zelber-Sagi S, et al. Diagnostic value of computerized hepatorenal index for sonographic quantification of liver steatosis. AJR Am J Roentgenol. 2009;192:909–14.
Salgado AL, Carvalho Ld, Oliveira AC, Santos VN, Vieira JG, Parise ER. Insulin resistance index (HOMA-IR) in the differentiation of patients with non-alcoholic fatty liver disease and healthy individuals. Arq Gastroenterol. 2010;47:165–9.
Eguchi Y, Eguchi T, Mizuta T, et al. Visceral fat accumulation and insulin resistance are important factors in nonalcoholic fatty liver disease. J Gastroenterol. 2006;41:462–9.
Kim HJ, Kim HJ, Lee KE, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med. 2004;164:2169–75.
Loomis AK, Kabadi S, Preiss D, et al. Body mass index and risk of nonalcoholic fatty liver disease: two electronic health record prospective studies. J Clin Endocrinol Metab. 2016;101:945–52.
Margariti E, Deutsch M, Manolakopoulos S, Papatheodoridis GV. Non-alcoholic fatty liver disease may develop in individuals with normal body mass index. Ann Gastroenterol. 2012;25:45–51.
Marovic D. Elevated body mass index and fatty liver. Srp Arh Celok Lek. 2008;136:122–5.
Tilg H, Moschen RA, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14:32–42.
Hazlehurst JM, Woods C, Marjot T, Cobbold JF, Tomlinson JW. Non-alcoholic fatty liver disease and diabetes. Metabolism. 2016;65:1096–108.
Musso G, Gambino R, Cassader M, Pagano G. Meta analysis: natural history of non-alcoholic liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43:617–49.
Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis. Diabetes Care. 2018. 41:372–82.
Williams KH, Shackel NA, Gorrell MD, McLennan SV, Twigg SM. Diabetes and nonalcoholic fatty liver disease: a pathogenic duo. Endocr Rev. 2013;34:84–129.
Willner IR, Waters B, Patil SR, Reuben A, Morelli J, Riely CA. Ninety patients with nonalcoholic steatohepatitis: insulin resistance, familial tendency, and severity of disease. Am J Gastroenterol. 2001;96:2957–61.
Ortiz-Lopez C, Lomonaco R, Orsak B, et al. Prevalence of prediabetes and diabetes and metabolic profile of patients with nonalcoholic fatty liver disease (NAFLD). Diabetes Care. 2012;35:873–8.
Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–23.
Doerr R, Hoffmann U, Otter W, et al. Oral glucose tolerance test and HbA1 c for diagnosis of diabetes in patients undergoing coronary angiography: [corrected] the Silent Diabetes Study. Diabetologia. 2011;54:2923–30.
Peter A, Fritsche A, Stefan N, Heni M, Häring HU, Schleicher E. Diagnostic value of hemoglobin A1c for type 2 diabetes mellitus in a population at risk. Exp Clin Endocrinol Diabetes. 2011;119:234–7.
Midthjell K, Lee CMY, Platou CGP, Colagiuri S. Comparison of HbA1c and OGTT in the diagnosis of diabetes in high-risk population. The HUNT-DE-PLAN Study, Norway. Diabetologia. 2010; 53: 87–93.
Hjellestad ID, Astor MC, Nilsen RM, Søfteland E, Jonung T4. Correction to: HbA 1c versus oral glucose tolerance test as a method to diagnose diabetes mellitus in vascular surgery patients. Cardiovasc Diabetol. 2018;17:42.
Shibata M, Kihara Y, Taguchi M, Tashiro M, Otsuki M. Nonalcoholic fatty liver disease is a risk factor for type 2 diabetes in middle-aged Japanese men. Diabetes Care. 2007;30:2940–4.
Kim CH, Park JY, Lee KU, Kim JH, Kim HK. Fatty liver is an independent risk factor for the development of type 2 diabetes in Korean adults. Diabet Med. 2008;25:476–81.
Adams LA, Waters OR, Knuiman MW, Elliott RR, Olynyk JK. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol. 2009;104:861–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PA, MA, ZN, BI, KS, and ES declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Avramovski, P., Avramovska, M., Nikleski, Z. et al. The predictive value of the hepatorenal index for detection of impaired glucose metabolism in patients with non-alcoholic fatty liver disease. Indian J Gastroenterol 39, 50–59 (2020). https://doi.org/10.1007/s12664-019-01009-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-019-01009-7