Abstract
Background
Though pathogenesis of non-alcoholic steatohepatitis (NASH) is unclear, association with small intestinal bacterial overgrowth [SIBO] and fecal dysbiosis is suggested. We evaluated SIBO in NASH using quantitative jejunal aspirate culture (conventional criteria: ≥ 105 colony forming unit (CFU)/mL and newer cutoff ≥ 103 CFU/mL) and glucose hydrogen breath test.
Methods
Thirty-eight patients with NASH (age 37.5 years, range 20–54, 9, 24% female), diagnosed by ultrasonography, alanine aminotransferase >1.5 times normal and liver biopsy (in 27/38, 71%) and exclusion of other causes and 12 constipation-predominant irritable bowel syndrome as historical controls (age 39.5-y, 26–44; 3, 25% female) without fatty liver were studied.
Results
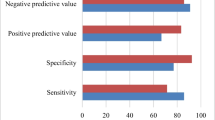
Jejunal aspirates, obtained in 35/38 patients, were sterile in 14/35 (40%) and bacteria isolated in 21 (60%) (all aerobic, in one anaerobe also; Gram positive 5, negative 13, both 3). In contrast, bacteria (two Gram negative) were isolated in 3/12 (25%) controls (odds ratio 4.5, 95% CI 1.0–19.5; p = 0.04); colony counts were higher in NASH than controls (median 380 CFU/mL, 0–200,000 vs. 0 CFU/mL, 0–1000; p = 0.02). Gram negative bacteria tended to be commoner in NASH than controls (16/35 vs. 2/12; p = 0.07). Seven out of 35 (20%) patients with NASH (≥ 105 CFU/mL in 5 and 2 other on glucose hydrogen breath test) and no control had SIBO (p = ns); low-grade SIBO (≥103 CFU/mL) was commoner in NASH than controls (14/35, 40%, vs. 1/12, 8.3%; p = 0.04). There was no correlation between bacterial colony count and bacterial type and anthropometric and biochemical parameters.
Conclusion
Low-grade bacterial overgrowth, particularly with Gram negative bacteria, was commoner in NASH than controls.



Similar content being viewed by others
References
Bellentani S. The epidemiology of non-alcoholic fatty liver disease. Liver Int. 2017;37 Suppl 1:81–4.
Agrawal S, Duseja AK. Non-alcoholic fatty liver disease: east versus west. J Clin Exp Hepatol. 2012;2:122–34.
Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356–62.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149. 389-97:e10.
Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58:1538–44.
Ratziu V, Giral P, Charlotte F, et al. Liver fibrosis in overweight patients. Gastroenterology. 2000;118:1117–23.
Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–10.
Wiest R, Albillos A, Trauner M, Bajaj J, Jalan R. Targeting the gut-liver axis in liver disease. J Hepatol. 2017; pii: S0168-8278(17)32016-0.
Sreenivasa Baba C, Alexander G, Kalyani B, et al. Effect of exercise and dietary modification on serum aminotransferase levels in patients with nonalcoholic steatohepatitis. J Gastroenterol Hepatol. 2006;21:191–8.
Boursier J, Mueller O, Barret M, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764–75.
Fialho A, Thota P, McCullough AJ, Shen B. Small intestinal bacterial overgrowth is associated with non-alcoholic fatty liver disease. J Gastrointestin Liver Dis. 2016;25:159–65.
Kapil S, Duseja A, Sharma BK, et al. Small intestinal bacterial overgrowth and toll-like receptor signaling in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2016;31:213–21.
Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarthy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut. 2001;48:206–11.
Sabate JM, Jouet P, Harnois F, et al. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: a contributor to severe hepatic steatosis. Obes Surg. 2008;18:371–7.
Ghoshal UC, Ghoshal U. Small intestinal bacterial overgrowth and other intestinal disorders. Gastroenterol Clin N Am. 2017;46:103–20.
Hocking MP, Duerson MC, O'Leary JP, Woodward ER. Jejunoileal bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308:995–9.
Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17:510–9.
Drenick EJ, Fisler J, Johnson D. Hepatic steatosis after intestinal bypass--prevention and reversal by metronidazole, irrespective of protein-calorie malnutrition. Gastroenterology. 1982;82:535–48.
Gangarapu V, Ince AT, Baysal B, et al. Efficacy of rifaximin on circulating endotoxins and cytokines in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2015;27:840–5.
Ma YY, Li L, Yu CH, Shen Z, Chen LH, Li YM. Effects of probiotics on nonalcoholic fatty liver disease: a meta-analysis. World J Gastroenterol. 2013;19:6911–8.
Duseja A, Chawla YK. Obesity and NAFLD: the role of bacteria and microbiota. Clin Liver Dis. 2014;18:59–71.
Ghoshal UC. How to interpret hydrogen breath tests. J Neurogastroenterol Motil. 2011;17:312–7.
Ghoshal UC, Ghoshal U, Ayyagari A, et al. Tropical sprue is associated with contamination of small bowel with aerobic bacteria and reversible prolongation of orocecal transit time. J Gastroenterol Hepatol. 2003;18:540–7.
Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70.
Scatarige JC, Scott WW, Donovan PJ, Siegelman SS, Sanders RC. Fatty infiltration of the liver: ultrasonographic and computed tomographic correlation. J Ultrasound Med. 1984;3:9–14.
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–74.
Ghoshal U, Ghoshal UC, Ranjan P, Naik SR, Ayyagari A. Spectrum and antibiotic sensitivity of bacteria contaminating the upper gut in patients with malabsorption syndrome from the tropics. BMC Gastroenterol. 2003;3:9.
Collee JG, Miles RS, Walt B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. New York: Churchill Livingstone; 1996. p. 131–49.
Anonymous. Processing clinical specimens for anaerobic bacteria: Isolation and identification procedures. In: Baron EJ, Peterson LR, Finegold SM, editors. Bailey and Scott’s Diagnostic Microbiology. Philadelphia: Mosby; 1994. p. 474–503.
Bardhan PK, Gyr K, Beglinger C, Vogtlin J, Frey R, Vischer W. Diagnosis of bacterial overgrowth after culturing proximal small-bowel aspirate obtained during routine upper gastrointestinal endoscopy. Scand J Gastroenterol. 1992;27:253–6.
Bala L, Ghoshal UC, Ghoshal U, et al. Malabsorption syndrome with and without small intestinal bacterial overgrowth: a study on upper-gut aspirate using 1H NMR spectroscopy. Magn Reson Med. 2006;56:738–44.
Lakshmi CP, Ghoshal UC, Kumar S, et al. Frequency and factors associated with small intestinal bacterial overgrowth in patients with cirrhosis of the liver and extra hepatic portal venous obstruction. Dig Dis Sci. 2009;55:1142–8.
Ghoshal UC, Srivastava D, Ghoshal U, Misra A. Breath tests in the diagnosis of small intestinal bacterial overgrowth in patients with irritable bowel syndrome in comparison with quantitative upper gut aspirate culture. Eur J Gastroenterol Hepatol. 2014;26:753–60.
Ghoshal UC, Srivastava D, Misra A, Ghoshal U. A proof-of-concept study showing antibiotics to be more effective in irritable bowel syndrome with than without small-intestinal bacterial overgrowth: a randomized, double-blind, placebo-controlled trial. Eur J Gastroenterol Hepatol. 2016;28:281–9.
Goel A, Gupta M, Aggarwal R. Gut microbiota and liver disease. J Gastroenterol Hepatol. 2014;29:1139–48.
Festi D, Schiumerini R, Eusebi LH, Marasco G, Taddia M, Colecchia A. Gut microbiota and metabolic syndrome. World J Gastroenterol. 2014;20:16079–94.
Greenhill C. Obesity: gut microbiota, host genetics and diet interact to affect the risk of developing obesity and the metabolic syndrome. Nat Rev Endocrinol. 2015;11:630.
Duseja A, Singh SP, Saraswat VA, et al. Non-alcoholic Fatty Liver Disease and Metabolic Syndrome-Position Paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of Gastroenterology. J Clin Exp Hepatol. 2015;5:51–68.
Riordan SM, McIver CJ, Williams R. Liver damage in human small intestinal bacterial overgrowth. Am J Gastroenterol. 1998;93:234–7.
Boursier J, Diehl AM. Implication of gut microbiota in nonalcoholic fatty liver disease. PLoS Pathog. 2015;11:e1004559.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol. 2012;107:811–26.
Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–24.
Jiang W, Wu N, Wang X, et al. Dysbiosis gut microbiota associated with inflammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease. Sci Rep. 2015;5:8096.
Wang B, Jiang X, Cao M, et al. Altered fecal microbiota correlates with liver biochemistry in nonobese patients with non-alcoholic fatty liver disease. Sci Rep. 2016;6:32002.
Krajicek EJ, Hansel SL. Small intestinal bacterial overgrowth: A primary care review. Mayo Clin Proc. 2016;91:1828–33.
Corazza GR, Menozzi MG, Strocchi A, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology. 1990;98:302–9.
Dellert SF, Nowicki MJ, Farrell MK, Delente J, Heubi JE. The 13C-xylose breath test for the diagnosis of small bowel bacterial overgrowth in children. J Pediatr Gastroenterol Nutr. 1997;25:153–8.
Ghoshal UC, Kumar S, Mehrotra M, Lakshmi C, Misra A. Frequency of small intestinal bacterial overgrowth in patients with irritable bowel syndrome and chronic non-specific diarrhea. J Neurogastroenterol Motil. 2010;16:40–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
UCG, CSB, UG, GA, AM, VAS, and GC declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning Human and Animal Rights. The protocol was approved by the Institutional Ethics Committee and informed consent was obtained from the study subjects.
Rights and permissions
About this article
Cite this article
Ghoshal, U.C., Baba, C.S., Ghoshal, U. et al. Low-grade small intestinal bacterial overgrowth is common in patients with non-alcoholic steatohepatitis on quantitative jejunal aspirate culture. Indian J Gastroenterol 36, 390–399 (2017). https://doi.org/10.1007/s12664-017-0797-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-017-0797-6