Abstract
Introduction
Sinus augmentation requires careful manipulation of the Schneider membrane. Perforation of the membrane can be a challenging complication.
Objectives
The objective of this study is to evaluate the sexual dimorphism of Schneider membrane (sinus membrane) using cone-beam computed tomography (CBCT) imaging modality and discuss its clinical applications vis-à-vis the sinus lift procedure for dental implants and also its forensic implications.
Materials and methods
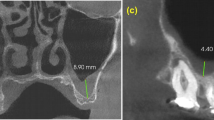
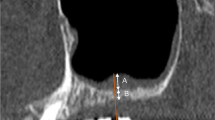
One hundred CBCT scans in the maxillary first molar region of fifty men and fifty women in the age group of 25–50 years were examined at two standardized points on the floor and lateral wall of maxillary sinus, and its mean was obtained. Measurements were taken for thickness of sinus membrane at most prominent antero-posterior and mesio-distal dimensions. The mean sinus membrane thickness and correlation in age groups (25–35 and 36–50 years) of both the genders were evaluated statistically.
Results
The results showed a thicker sinus membrane in women, especially in 36–50 age group than that of men.
Conclusion
This study correlates the thickness of the sinus membrane with gender dimorphism and delves on its association with the risk of perforation during sinus lift procedures and also its forensic implications.


Similar content being viewed by others
References
Humphrey S (2006) Implant maintenance. Dent Clin North Am 50(3):463–478
Ritter FN, Lee D (1978) The para nasal sinuses, anatomy and surgical technique, 6–16. The Mosby Company, St Louis, MO
McGowan DA, Baxter PW, James J (1993) The maxillary sinus and its dental implications, chapter 1, 1–125. Wright, Butterworth-Heinemann Ltd, Oxford
Stamberger H (1986) Nasal and paranasal sinus endoscopy. Endoscopy 6:213–218
May M, Sobol SM, Korzec K (1990) The location of the maxillary os and its importance to the endoscopic sinus surgeon. Laryngoscope 100:1037–1042
Eckert-Mobius A (1954) Die Kieferho¨ hlenentzu ¨ ndung im Kindersalter. Deutsche Stomatologie 00:170–177
Van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB (2000) Anatomical aspects of sinus floor elevations. Clin Oral Implants Res 11:256–265
Rapani M, rapaniRicci CL (2016) Scheider membrane thickness classification evaluated by cone-beam computed tomography and its importance in the predictability of perforation retrospective analysis of 200 patients. BJ Oral Maxillofac Aug 28(54):1106–1110
Hegde R, Prasad K, Shroff K (2016) Maxillary sinus augmentation using sinus membrane elevation without grafts- A systemic Review. J Indian Prosthodont Soc OCT-Dec 16(4):317–322
Pal US, Sharma N, Mandhyan D (2012) Direct vs. Indirect sinus lift procedure: a comparison. Natl J maxillofac Surg 3(1):31–37
Vijaykumar B, pavaniRaviraj MJ et al (2015) comparison of panoramic radiograph with cone-beam computed tomography in assessment of maxillary sinus floor and nasal floor. J Indian Acad Oral Med Radiol 27(2):194–197
Suresh Sharma J, Massarat Anil, kumar. (2014) Measurements of maxillary sinus volume and dimensions by computed tomography scan for gender determination. J Anat Soc India 63(1):36–42
Al-Salman WT, Almas K (2015) Maxillary sinus and success of dental implants: an update. Gen Dent. 63(4):47–54
Rehman Hamdy N, Wahed et al (2014) Three-dimensional linear and volumetric analysis of maxillary sinus pneumatisation. J Adv Res 5(3):387–395
Aimetti M, G massei, Morra M, et al (2008) Correlation between gingival phenotype and Schneider membrane thickness. Int J Oral Maxillofac Implants 23(6):1128–1132
Janner SF, Caversaccio MD, Dubach P, Sendi P, Buser D, Bornstein MM (2011) Characteristics and dimensions of the Schneider membrane: a radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin Oral Implants Res 22(12):1446–1453. https://doi.org/10.1111/j.1600-0501.2010.02140.x
Shahnaz tambawala, Frenykarjodkar, KaustubhSansare et al. Sexual dimorphism of maxillary sinus using cone beam computed tomography. Egypt J Forens Sci 2016(6): 120-125
Ruhi Sidhu S, Chandra Parvathi Devi et al (2014) forensic importance of maxillary sinus in gender determination: a morphometric analysis from Western Uttar Pradesh, India. Eur J General Dent 3(1):53–56
Bayrak S, Ustaoğlu G, Demiralp KÖ, Kurşun Çakmak EŞ (2018) Evaluation of the characteristics and association between Schneider membrane thickness and nasal septum deviation. J Craniofac Surg 29(3):683–687. https://doi.org/10.1097/SCS.0000000000004254
Kalyvas D, Kapsalas A, Paikou S, Tsiklakis K (2018) Thickness of the Schneider membrane and its correlation with anatomical structures and demographic parameters using CBCT tomography: a retrospective study. Int J Implant Dent 4(1):32. https://doi.org/10.1186/s40729-018-0143-5
Çakur B, Sümbüllü MA, Durna D (2013) Relationship among Schneider membrane, underwood’s septa, and the maxillary sinus inferior border. Clin Implant Dent Related Res 15:83–87. https://doi.org/10.1111/j.1708-8208.2011.00336.x
Huang Yen-Ting, Suh-Woan Hu, Huang Jing-Yang, Chang Yu-Chao (2020) Assessment of relationship between maxillary sinus membrane thickening and the adjacent teeth health by cone-beam computed tomography. J Dental Sci. https://doi.org/10.1016/j.jds.2020.05.002
Van Den Munckhof T, Patel S, Koller G, Berkhout E, Mannocci F, Foschi F (2020) Schneider membrane thickness variation following endodontic procedures: a retrospective cone beam computed tomography study. BMC Oral Health 20(1):133. https://doi.org/10.1186/s12903-020-01122-6
Dr. Chandulal D. Dhalkari, Dr. Maya S. Indurkar, Dr. Onkar A. Bagade and Dr. Jaishri S. Pagare (2019) Relationship between thickness of the Schneider membrane and dental findings. A retrospective CBCT study International journal of current research. 11(07): 5206-5212 https://doi.org/10.24941/ijcr.35715.07.2019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest
Ethics Approval
No ethics approval or patients’ consent was required for this paper, though the patients gave written consent to use their CBCT scans and participate for the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takalkar, S., Girotra, C., Kini, Y. et al. Evaluation of Sexual Dimorphism in Schneider Membrane Thickness Using Cone-Beam Computed Tomography (CBCT) for its Clinical and Forensic Implications. J. Maxillofac. Oral Surg. (2021). https://doi.org/10.1007/s12663-021-01531-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-021-01531-2