Abstract
Purpose
Our objective was to investigate the temporal trends in baseline characteristics, interventions, and clinical outcomes in patients hospitalized with COVID-19 in Canada over five pandemic waves.
Methods
We conducted a multicentre prospective cohort study enrolling adults and children admitted with COVID-19 from 47 Canadian hospitals. We compared characteristics, interventions, and outcomes of patients across five distinct pandemic waves.
Results
We enrolled 5,285 patients between 2 January 2020 and 8 February 2022. The mean (standard deviation) age was 62.6 (21.0) yr; 41.2% (n = 2,176) were female, and 48% (n = 2,539) required admission to an intensive care unit (ICU), of whom 60.3% (n = 1,530) underwent invasive mechanical ventilation. The proportion of vaccinated patients increased over time. The proportion of vaccinated hospitalized patients progressing to require ICU admission fell over pandemic waves while the proportion of unvaccinated hospitalized patients progressing to require ICU admission did not. Patients were most commonly treated with corticosteroids (48.7%; n = 2,575); use of corticosteroids and other evidence-based treatments increased over time. Hospital mortality was 22.1% (n = 1,166) among all patients, 30.2% (n = 766) among those admitted to an ICU, and 37.9% (n = 580) among those requiring invasive mechanical ventilation. Younger age, absence of chronic cardiac or pulmonary disease, severity of illness at admission, and prior vaccination was associated with a lower mortality; however, pandemic wave itself was not.
Conclusion
Among patients hospitalized in Canada with COVID-19, several clinical factors including prior vaccination were associated with lower mortality, but pandemic wave was not.
Résumé
Objectif
Notre objectif était d’étudier les tendances temporelles des caractéristiques de base, des interventions et des issues cliniques chez la patientèle hospitalisée pour cause de COVID-19 au Canada au cours de cinq vagues de la pandémie.
Méthode
Nous avons mené une étude de cohorte prospective multicentrique auprès d’adultes et d’enfants admis·es avec la COVID-19 dans 47 hôpitaux canadiens. Nous avons comparé les caractéristiques, les interventions et les issues des patient·es sur cinq vagues pandémiques distinctes.
Résultats
Nous avons recruté 5285 patient·es entre le 2 janvier 2020 et le 8 février 2022. L’âge moyen (écart type) était de 62,6 (21,0) ans; 41,2 % (n = 2176) étaient des femmes, et 48 % (n = 2539) ont dû être admis·es à une unité de soins intensifs (USI), dont 60,3 % (n = 1530) ont bénéficié de ventilation mécanique invasive. La proportion de patient·es vacciné·es a augmenté au fil du temps. La proportion de patient·es hospitalisé·es vacciné·es nécessitant une admission aux soins intensifs a diminué au cours des vagues pandémiques, tandis que la proportion de patient·es hospitalisé·es non vacciné·es nécessitant une admission aux soins intensifs n’a pas diminué. Les patient·es étaient le plus souvent traité·es par corticostéroïdes (48,7 %; n = 2575); l’utilisation de corticostéroïdes et d’autres traitements fondés sur des données probantes a augmenté au fil du temps. La mortalité hospitalière était de 22,1 % (n = 1166) parmi l’ensemble des patient·es, 30,2 % (n = 766) chez les personnes admises à l’unité de soins intensifs, et 37,9 % (n = 580) parmi les personnes nécessitant une ventilation mécanique invasive. Le jeune âge, l’absence de maladie cardiaque ou pulmonaire chronique, la gravité de la maladie à l’admission et la vaccination antérieure étaient associés à une mortalité plus faible; cependant, la vague pandémique elle-même ne l’était pas.
Conclusion
Parmi les personnes hospitalisées au Canada en raison de la COVID-19, plusieurs facteurs cliniques, y compris la vaccination antérieure, étaient associés à une mortalité plus faible, mais pas la vague pandémique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The COVID-19 pandemic led to an increased demand for inpatient care services, with hospitals and intensive care units (ICUs) overwhelmed during the peaks of epidemiological waves in many health systems. Globally, mortality was high when demand exceeded capacity for acute care in many global jurisdictions early in the pandemic. Canadian data from the pandemic’s first waves indicated an overall hospital morality of 20% and an ICU mortality of 26%.1 Nevertheless, mortality has varied over time and across jurisdictions.2,3,4,5
Public health measures to reduce SARS-CoV-2 infections, including vaccination, have reduced the spread and severity of COVID-19 in Canada.6 Numerous therapies have been studied, and dexamethasone, remdesivir, tocilizumab, and baricitinib have been incorporated into the standard of medical care for eligible inpatients.7,8,9,10,11
To better prepare for future pandemics, it is important to assess characteristics of this pandemic and how it evolved over distinct waves. Using a national data collection protocol in hospitals throughout Canada, we investigated temporal trends in baseline characteristics, interventions received, and clinical outcomes in patients hospitalized with COVID-19.
Methodology
Objective
Our objective was to investigate temporal trends in baseline characteristics, vaccination status, interventions received, and clinical outcomes in hospitalized patients with COVID-19 over five pandemic waves in Canada.
Study design
The Short Period Incidence Study of Severe Acute Respiratory Infection (SPRINT-SARI) is an international collaboration initiated in 2016 designed to describe the prevalence of severe acute respiratory infection in hospitals, and characteristics of patients and clinical outcomes.1 At the beginning of the COVID-19 pandemic, the SPRINT-SARI case report form was adapted to conduct a multicentre prospective cohort study enrolling adults and children admitted to hospitals with COVID-19. In Canada, we recruited sites through both the Canadian Critical Care Trials Group and the Association of Medical Microbiology and Infectious Disease Canada.
Participants
Patients admitted to participating hospitals with proven acute respiratory infection with SARS-CoV-2; with onset within the past 14 days; and with one or more of fever, cough, dyspnea, or tachypnoea were eligible for inclusion. Patient recruitment was targeted during periods corresponding to population-level waves of infection to characterize changing patterns of illness over time. While not all patients admitted to hospital with COVID-19 were enrolled, to minimize selection bias, the protocol emphasized enrolment of consecutive patients according to either start and stop dates or to a total number of patients at sites. Infection with SARS-CoV-2 was confirmed by polymerase chain reaction (PCR) for all patients. Critically ill patients were defined as those ever admitted to an ICU. Using prespecified case report forms, data were collected on admission to hospital and ICU and on the day of discharge for all patients. On a subset of patients, daily data were also collected. We collected patient demographics, characteristics, comorbidities, symptoms on presentation, severity of illness by the quick Sequential Organ Failure Assessment (qSOFA) score,12 oxygenation and ventilation support modalities, mortality, duration of mechanical ventilation, and ICU and hospital length of stay. Vaccination status was captured as a binary variable, such that receipt of any dose of vaccine classified the patient as vaccinated. Vaccination timing was also recorded.
Statistical analysis
We characterized patients admitted across the first five Canadian pandemic waves: 1 January to 31 August 2020, 1 September 2020 to 28 February 2021, 1 March to 30 June 2021, 1 July to 31 December 2021, and 1 January to 8 February 2022. While there is no consensus definition of onset and conclusion of each COVID-19 wave, these dates were chosen to reflect peak periods of infection at a national level, appreciating geographic variation in onset, and to encompass interpeak hospitalizations. Continuous data are summarized using means and standard deviation (SD) or medians and interquartile range [IQR], and compared using ANOVA or the Kruskal–Wallis test. Test for trend was performed using Cochran–Armitage for categorical variables and linear regression for continuous variables. Categorical data were compared using the Chi square test and are presented per wave as frequencies and proportions. If vaccination status was missing or unknown, we coded it as “no” before 14 December 2020 and considered it “missing” after this date.6 To assess the association between hospital mortality and COVID-19 waves adjusting for vaccination status, sex, age, qSOFA, diabetes mellitus, hypertension, chronic cardiac disease, and chronic pulmonary disease, we used generalized estimating equations with clustering of patients within sites. The associations between covariates and mortality are presented as odds ratios and 95% confidence intervals. All tests are two-sided with a P value less than 0.05 considered statistically significant. Analyses were not adjusted for multiple comparisons. The analyses were performed in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline
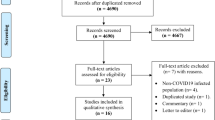
From 1 January 2020 to 8 February 2022, we enrolled 5,285 patients with confirmed COVID-19 across 47 hospitals (21 adult academic, 19 community, and seven pediatric academic) (Electronic Supplementary Material [ESM] eFigure), of which 48.0% (n = 2,539) required admission to an ICU at any time during hospital admission. The mean (SD) age was 62.6 (21.0) years and 2,176 (41.2%) were female. The cohort included 74 (3.5% of women) pregnant patients and 170 (3.2%) health care workers (Table 1). Hypertension (51.9%) was the most common comorbidity, followed by diabetes mellitus (32.3%) and chronic cardiac disease (24.5%) (Table 1). Shortness of breath (70.5%), cough (66.2%), and fever (64.5%) were the most common symptoms (Fig. 1). The mean age of patients admitted to an ICU was 60.3 (16.9) yr and 926 (36.5%) were women. The baseline characteristics of all hospitalized, critically ill, and invasively ventilated patients including the unknown/missing are presented in ESM eTables 1–3.
Supportive care
Oxygen was administered to 70.7% (n = 3,737) of all patients, high-flow nasal oxygen (HFNO) to 29.2% (n = 1,543), noninvasive mechanical ventilation (NIV) to 7.9% (n = 418), invasive mechanical ventilation to 29.0% (n = 1,533), vasopressor/inotrope support to 27.5% (n = 1,453), dialysis to 6.5% (n = 345), and prone positioning to 17.8% (n = 939) at any point during admission.
Among patients admitted to an ICU, 92.9% (n = 2,360) received some form of oxygen, 48.5% (n = 1,232) received HFNO, 14.6% (n = 370) NIV, 60.3% (n = 1,530) invasive mechanical ventilation, 56.3% (n = 1,429) vasopressor/inotropic support, 11.8% (n = 300) dialysis, 33.2% (n = 844) prone positioning, and 3.3% (n = 85) extracorporeal membrane oxygenation (ESM eTable 4). Characteristics of patients invasively ventilated are presented in ESM eTable 5.
Medications
Corticosteroids were the most commonly received medication (received by 48.7% of patients, n = 2,575). Interleukin (IL)-6 receptor inhibitors were received by 5.2% (n = 277), remdesivir by 4.5% (n = 236), neuraminidase inhibitors by 4.3% (n = 227), chloroquine/hydroxychloroquine by 2.3% (n = 122), protease inhibitors by 2.1% (109), baricitinib by 0.3% (n = 18), interferons by 0.1% (n = 3), and bamlanivimab by one patient. Antibiotics were received by 73.9% (n = 3,906) of all patients.
Among patients admitted to an ICU, corticosteroids were received by 68.8% (n = 1,746), IL-6 inhibitors by 9.0% (n = 228), remdesivir by 5.3% (n = 134), neuraminidase inhibitors by 6.3% (n = 161), chloroquine/hydroxychloroquine by 3.2% (n = 81), protease inhibitors by 2.7% (n = 68), baricitinib by 0.4% (n = 11), and interferons by 0.1% (n = 3). Antibiotics were received by 88.8% (n = 2,255) of patients admitted to an ICU.
Outcomes
Median [IQR] hospital length of stay among all patients was 12 [5–24] days; 17 [9–30] days if admitted to ICU and 21 [13–39] days for those requiring invasive mechanical ventilation. Hospital mortality among all patients was 22.1% (n = 1,166); 30.2% (N = 766) if admitted to an ICU and 37.9% (n = 580) among those invasively ventilated.
Comparison across pandemic waves
The number of patients enrolled varied across waves, with the greatest number of patients being enrolled in the study during the first wave (n = 2,123) and the least during the fourth wave (n = 197) (Table 1). Among all hospitalized patients, fever was the most common symptom in wave one, shortness of breath in waves two and three, and cough was the most common symptom in wave five (see Fig. 1). The proportion of enrolled patients requiring admission to an ICU also varied, with the highest proportion occurring during the second wave (56.3%) and the least during the fifth wave (32.5%) (Table 1). The mean (SD) age of hospitalized patients was greatest during the first wave (64.8 [19.4] yr) and lowest during the fourth wave (52.7 [25.1] yr) (Table 1). The first wave saw the highest proportion of critically ill patients requiring invasive mechanical ventilation at 65.5% (n = 565) after which rates consistently decreased to 42.9% (n = 33) in the fifth wave.
Corticosteroids administration increased from 22.3% (n = 474) in wave one to 72.5% (n = 1,363) in wave two and remained high in the following waves (Table 1). Interleukin-6 inhibitor administration also increased as the pandemic progressed, from 0.7% (n = 14) and 1% (n = 19) in the first two waves to 23.6% (n = 200) and 16.2% (n = 32) in the third and fourth waves, respectively (Table 1). Interleukin-6 inhibitors were primarily administered to patients admitted to the ICU (82.3% [n = 228] of all patients receiving this medication; ESM eTable 1). Remdesivir administration increased after the first wave and remained prominent in the following waves (Table 1). Baricitinib use began in the fourth wave and continued into the fifth wave (Table 1). The administration of hydroxychloroquine, neuraminidase inhibitors, and protease inhibitors occurred primarily in the first wave and decreased thereafter (Table 1). All P values in Table 1 were < 0.05 except for asthma and treatment with interferons and bamlanivimab. Trends across the waves are presented in ESM eTables 6–8.
Vaccination
In total, 6.0% (n = 318) of all hospitalized patients were vaccinated, increasing across pandemic waves (Fig. 2). From the beginning of vaccination in Canada,6 30.2% (n = 96) of vaccinated hospitalized patients progressed to requiring admission to an ICU compared with 49.2% (n = 2,443) of unvaccinated hospitalized patients. The proportion of vaccinated hospitalized patients progressing to require ICU admission was 50% (n = 3) in the second wave, 41.5% (n = 51) in the third wave, 20.3% (n = 14) in the fourth wave, and 23.3% (n = 28) in the fifth wave. The proportion of unvaccinated hospitalized patients progressing to require ICU admission was 56.3% (n = 1,055) in the second wave, 56.0% (n = 406) in the third wave, 51.6% (n = 66) in the fourth wave, and 41.9% (n = 49) in the fifth wave.
Mortality
After we adjusted for vaccination status, sex, age, diabetes mellitus, hypertension, chronic cardiac disease, chronic pulmonary disease, and qSOFA on presentation to the hospital, we found that the specific pandemic wave, considering the first five waves of the pandemic, had negligible impact on mortality (Table 2). Older age (odds ratio [OR], 1.64; 95% confidence interval [CI], 1.50 to 1.79; P < 0.001), chronic pulmonary disease (OR, 1.43; 95% CI, 1.11 to 1.83; P < 0.01) and greater severity of illness by qSOFA at presentation (OR, 4.31; 95% CI, 2.94 to 6.33; P < 0.001) were associated with higher mortality. Receipt of vaccination (OR, 0.50; 95% CI, 0.32 to 0.78; P < 0.01) and female sex (OR, 0.78; 95% CI, 0.66 to 0.91; P < 0.01) were associated with lower mortality (Table 2).
Analyzing the cohort of critically ill patients, older age, greater severity of illness, chronic cardiac disease, and chronic pulmonary disease on presentation were associated with higher mortality (ESM eTable 9). In the cohort of invasively ventilated patients, only older age, chronic cardiac disease, and chronic pulmonary disease on presentation were associated with higher mortality (ESM eTable 10).
Discussion
Among patients hospitalized in Canada with COVID-19 across five pandemic waves from 1 January 2020 to 8 February 2022, we found that 29% of all patients required invasive mechanical ventilation. Hospital mortality was 22.1% overall, 30.2% among those admitted to an ICU, and 37.9% in those on invasive mechanical ventilation. We found that prior receipt of vaccination was associated with a decreased risk of developing critical illness and lower mortality. While there were significant variations in the baseline characteristics and outcomes of patients enrolled across the various waves, wave itself was not associated with higher or lower adjusted mortality.
Since the beginning of the pandemic, reported hospital mortality has ranged widely.13,14 We report an overall mortality of 22.1%, comparable to earlier analyses and similar to what others have reported in many high-income countries.1,15 Although we described differences in mortality across the pandemic waves, varying patient characteristics and vaccination across waves appear to explain much of this variation. A large European multinational cohort of > 3,000 patients similarly found no difference in mortality across pandemic waves after adjusting for patient-level differences across waves.16
As treatments were studied, their clinical adoption evolved. Following the first wave, the use of hydroxychloroquine decreased significantly, aligning with emerging evidence of ineffectiveness.17 In contrast, we found an increased administration of corticosteroids from the second wave onwards and IL-6 receptor antagonists from the third wave onwards as trials showing efficacy were published.7,8,10 Given the challenges of confounding by indication and time-dependent biases in observational cohorts, we did not include treatments in our model to compare hospital mortality across different waves of COVID-19.
A systematic review of 52 studies across multiple geographical regions found a pooled mortality of 35.3% in patients admitted to an ICU.18 We report a mortality slightly lower than what has been described globally, although comparable to some regions.16,19 We also found a lower mortality in patients who required invasive mechanical ventilation compared with two multinational systematic reviews reporting mortality of 45% and 47.9%, respectively.20,21 Potential explanations for these differences include varying underlying patient characteristics, variable criteria for ICU admission, differences in sampling techniques, and the availability of health care resources during surges. Consistent with previous findings, we also found that mortality worsened with increasing age,22 chronic pulmonary disease,23 chronic cardiac disease,24 and increasing severity of illness at presentation.25,26
We found that the proportion of patients hospitalized who were vaccinated increased with each consecutive pandemic wave, likely given vaccination uptake in the general Canadian population.27 Notably, progression to critical illness was lower in vaccinated patients compared with those unvaccinated. We also found prior vaccination to be protective against dying among hospitalized patients, consistent with prior studies.28,29,30 This protective effect, however, was not shown among critically ill and invasively ventilated patients, similar to what has been reported;31,32 however, this study is underpowered to investigate this association. In other studies, vaccination has been shown to decrease the risk of hospitalization and severity of COVID-19 illness.28,29 These findings highlight the major impact that vaccination has had on both the risk of infection and on outcomes for those who developed COVID-19 during the pandemic.
There are a number of limitations to our study. Data were extracted from case report forms, which lack granularity for some variables. For example, it was not possible to ascertain the timing of application of specific in-hospital treatments. Precise characterization of the severity of some pre-existing comorbidities was not possible. Likewise, the impact of pre-existing immunity against SARS-CoV-2, in the form of natural infection or vaccination boosters, could not be reliably ascertained. We were also not able to record changes over the course of the admission decisions to withhold life-sustaining treatments. Although we enrolled patients from 47 hospitals across Canada, the convenience sampling may result in data not fully representative of all Canadian patients hospitalized with COVID-19. Across Canada, there were around 164,093 confirmed COVID-19 hospitalizations from January 2020 to March 2022, of which 21.3% (n = 35,001) required admission to an ICU.33 Although we conducted a Cochran–Armitage test-for-trends, the smaller number of patients enrolled in waves four and five compared with the first three waves limits the power to compare findings across all waves. A key knowledge gap during this pandemic was timely ascertainment of virus and variant data, and linkage with clinical data. Specifically, at most participating centres, there was limited access to variant status or PCR cycle time in the clinical medical record. This knowledge gap will require collaboration among hospital and regional laboratories and provincial and national data repositories.
In conclusion, across the first five COVID-19 pandemic waves in Canada, we found that younger age, absence of chronic cardiac or pulmonary disease, lower severity of illness at presentation, and prior receipt of vaccination was associated with a decreased risk of developing critical illness and lower mortality, and that pandemic wave itself was less influential on clinical outcomes. It is possible that dynamic changes in treatment and capacity for acute care have residual effects on outcomes.
References
Murthy S, Archambault PM, Atique A, et al. Characteristics and outcomes of patients with COVID-19 admitted to hospital and intensive care in the first phase of the pandemic in Canada: a national cohort study. CMAJ Open 2021; 9: E181–8. https://doi.org/10.9778/cmajo.20200250
Bhatraju PK, Ghassemieh BJ, Nichols M, et al. COVID-19 in critically ill patients in the Seattle region—case series. N Engl J Med 2020; 382: 2012–22. https://doi.org/10.1056/nejmoa2004500
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323: 1574–81. https://doi.org/10.1001/jama.2020.5394
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020; 323: 2052–9. https://doi.org/10.1001/jama.2020.6775
Armstrong RA, Kane AD, Cook TM. Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies. Anaesthesia 2020; 75: 1340–9. https://doi.org/10.1111/anae.15201
Government of Canada. COVID-19 vaccine: doses administered; 2024. Available from URL: https://health-infobase.canada.ca/covid-19/vaccine-administration/ (accessed April 2024).
Abani O, Abbas A, Abbas F, et al. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021; 397: 1637–45. https://doi.org/10.1016/s0140-6736(21)00676-0
Gordon AC, Mouncey PR, Al-Beidh F, et al. Interleukin-6 receptor antagonists in critically ill patients with COVID-19. N Engl J Med 2021; 384: 1491–502. https://doi.org/10.1056/nejmoa2100433
Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of COVID-19—final report. N Engl J Med 2020; 383: 1813–26. https://doi.org/10.1056/nejmoa2007764
Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med 2021; 384: 693–704. https://doi.org/10.1056/nejmoa2021436
Ely EW, Ramanan AV, Kartman CE, et al. Efficacy and safety of baricitinib plus standard of care for the treatment of critically ill hospitalised adults with COVID-19 on invasive mechanical ventilation or extracorporeal membrane oxygenation: an exploratory, randomised, placebo-controlled trial. Lancet Respir Med 2022; 10: 327–36. https://doi.org/10.1016/s2213-2600(22)00006-6
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996; 22: 707–10. https://doi.org/10.1007/bf01709751
Nikpouraghdam M, Jalali Farahani A, Alishiri GH, et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in Iran: a single center study. J Clin Virol 2020; 127: 104378. https://doi.org/10.1016/j.jcv.2020.104378
Docherty AB, Mulholland RH, Lone NI, et al. Changes in in-hospital mortality in the first wave of COVID-19: a multicentre prospective observational cohort study using the WHO Clinical Characterisation Protocol UK. Lancet Respir Med 2021; 9: 773–85. https://doi.org/10.1016/s2213-2600(21)00175-2
Gray WK, Navaratnam AV, Day J, Wendon J, Briggs TW. COVID-19 hospital activity and in-hospital mortality during the first and second waves of the pandemic in England: an observational study. Thorax 2022; 77: 1113–20. https://doi.org/10.1136/thoraxjnl-2021-218025
Carbonell R, Urgelés S, Rodríguez A, et al. Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: a multicentre retrospective cohort study. Lancet Reg Health Eur 2021; 11: 100243. https://doi.org/10.1016/j.lanepe.2021.100243
Horby P, Mafham M, Linsell L, et al. Effect of hydroxychloroquine in hospitalized patients with COVID-19. N Engl J Med 2020; 383: 2030–40. https://doi.org/10.1056/nejmoa2022926
Armstrong RA, Kane AD, Kursumovic E, Oglesby FC, Cook TM. Mortality in patients admitted to intensive care with COVID-19: an updated systematic review and meta-analysis of observational studies. Anaesthesia 2021; 76: 537–48. https://doi.org/10.1111/anae.15425
Auld SC, Harrington KR, Adelman MW, et al. Trends in ICU mortality from coronavirus disease 2019: a tale of three surges. Crit Care Med 2022; 50: 245–55. https://doi.org/10.1097/ccm.0000000000005185
Lim ZJ, Subramaniam A, Reddy MP, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. A meta-analysis. Am J Respir Crit Care Med 2021; 203: 54–66. https://doi.org/10.1164/rccm.202006-2405oc
Leazer S, Collen J, Alcover K, et al. Outcomes associated with intensive care and organ support among patients with COVID-19: a systematic review and meta-analysis. Mil Med 2023; 188: 541–6. https://doi.org/10.1093/milmed/usac143
Li Bassi G, Suen JY, White N, et al. Assessment of 28-day in-hospital mortality in mechanically ventilated patients with coronavirus disease 2019: an international cohort study. Crit Care Explor 2021; 3: e0567. https://doi.org/10.1097/cce.0000000000000567
Kilic H, Arguder E, Karalezli A, et al. Effect of chronic lung diseases on mortality of prevariant COVID-19 pneumonia patients. Front Med (Lausanne) 2022; 9: 957598. https://doi.org/10.3389/fmed.2022.957598
Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation 2020; 141: 1648–55. https://doi.org/10.1161/circulationaha.120.046941
Beigmohammadi MT, Amoozadeh L, Rezaei Motlagh F, et al. Mortality predictive value of APACHE II and SOFA scores in COVID-19 patients in the intensive care unit. Can Respir J 2022; 2022: 5129314. https://doi.org/10.1155/2022/5129314
Ganesan R, Mahajan V, Singla K, et al. Mortality prediction of COVID-19 patients at intensive care unit admission. Cureus 2021; 13: e19690. https://doi.org/10.7759/cureus.19690
Government of Canada. COVID-19 vaccination: vaccination coverage; 2024. Available from: https://health-infobase.canada.ca/covid-19/vaccination-coverage/ (accessed April 2024).
Mohammed I, Nauman A, Paul P, et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Hum Vaccin Immunother 2022; 18: 2027160. https://doi.org/10.1080/21645515.2022.2027160
Nordström P, Ballin M, Nordström A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: a retrospective, total population cohort study in Sweden. Lancet 2022; 399: 814–23. https://doi.org/10.1016/s0140-6736(22)00089-7
Suthar AB, Wang J, Seffren V, Wiegand RE, Griffing S, Zell E. Public health impact of COVID-19 vaccines in the US: observational study. BMJ 2022; 377: e069317. https://doi.org/10.1136/bmj-2021-069317
Hilty MP, Keiser S, Wendel Garcia PD, Moser A, Schuepbach RA, RISC-19-ICU Investigators for Switzerland. mRNA-based SARS-CoV-2 vaccination is associated with reduced ICU admission rate and disease severity in critically ill COVID-19 patients treated in Switzerland. Intensive Care Med 2022; 48: 362–5. https://doi.org/10.1007/s00134-021-06610-z
Sevinc SA, Metin S, Basi NB, Ling J, Cinar AS, Oba S. Effectiveness of inactivated SARS-CoV-2 vaccine (CoronaVac) on intensive care unit survival. Epidemiol Infect 2022; 150: e35. https://doi.org/10.1017/s0950268822000267
Canadian Institute for Health Information. COVID-19 hospitalization and emergency department statistics; 2024. Available from URL: https://www.cihi.ca/en/covid-19-hospitalization-and-emergency-department-statistics (accessed April 2024).
Author information
Authors and Affiliations
Contributions
Divyajot Sadana, David Granton, Neill K. J. Adhikari, and Srinivas Murthy contributed to study conception and design, interpretation of data, and drafting the article. Ruxandra Pinto contributed to acquisition, analysis, interpretation of data, and drafting the article. Robert A. Fowler contributed to study conception and design, acquisition and interpretation of data, and drafting the article.
Corresponding author
Ethics declarations
Disclosures
The authors have no disclosures.
Funding statement
This study was supported by a grant from the Canadian Institutes of Health Research (CIHR).
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sadana, D., Granton, D., Adhikari, N.K.J. et al. Trends in characteristics, interventions, and outcomes of hospitalized patients with COVID-19 in Canada: a multicentre prospective cohort study. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02826-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02826-x