Abstract
Purpose
The acceptability of waiver of consent for participation in clinical research in intensive care unit (ICU) settings is uncertain. We sought to survey the Canadian public to assess levels of support, comfort, and acceptability for waived consent for low-risk clinical trials.
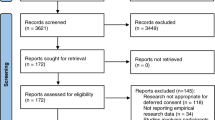
Methods
We performed a prospective cross-sectional survey of the Canadian public aged 18 yr or older. The survey was conducted by Ipsos between 19 and 23 November 2020. The survey content was derived from a literature review and in consultation with a patient and family partnership committee. The survey focused on attitudes and beliefs on waived consent for participation in low-risk clinical trials in ICU settings. The survey contained 35 items focused on sociodemographics, general health status, participation in medical research, and levels of support and comfort with research and with waived consent. The survey used a case study of a low-risk clinical trial intervention in ICU patients. Analysis was descriptive.
Results
We included 2,000 participants, 38% of whom reported experience with ICU and 16% with medical research. Participation in medical research was more common among those with postsecondary education, those with chronic disease, and those who were employed in health care. Most (80%) would support a model of waived consent for low-risk clinical trials, citing medical benefits (36%) and low perceived risk (34%). Most (77%) were comfortable with personally participating in a low-risk clinical trial. Most (80%) believed waived consent approaches were acceptable. Half (52%) believed the waived consent process should provide information about the research and include the option of opting out. When asked whether participants should always give full informed consent, regardless of the practicality or level of risk, 74% and 72% agreed, respectively.
Conclusions
There is public support for models of waived consent for participation in low-risk pragmatic clinical trials in ICU settings in Canada; however, this is not universal. This information can inform and guide education, ethics, policy, and legal discussion on consent models.
Résumé
Objectif
L’acceptabilité de la renonciation au consentement pour la participation à la recherche clinique à l’unité de soins intensifs (USI) est incertaine. Nous avons cherché à sonder la population canadienne afin d’évaluer les niveaux de soutien, de confort et d’acceptabilité de la renonciation au consentement pour les études cliniques à faible risque.
Méthode
Nous avons réalisé un sondage transversal prospectif auprès de la population canadienne âgée de 18 ans et plus. Le sondage a été réalisé par Ipsos entre le 19 et le 23 novembre 2020. Le contenu du sondage a été élaboré à partir d’une revue de la littérature et en consultation avec un comité de partenariat composé de patient·es et de familles. Le sondage portait sur les attitudes et les croyances à l’égard de la renonciation au consentement pour participer à des études cliniques à faible risque dans les unités de soins intensifs. Le sondage comportait 35 questions axées sur les données sociodémographiques, l’état de santé général, la participation à la recherche médicale et les niveaux de soutien et de confort à l’égard de la recherche et de la renonciation au consentement. Le sondage s’est appuyé sur une étude de cas d’une intervention d’étude clinique à faible risque chez des patient·es des soins intensifs. L’analyse était descriptive.
Résultats
Nous avons inclus 2000 personnes, dont 38 % ont déclaré avoir eu des expériences en soins intensifs et 16 % en recherche médicale. La participation à la recherche médicale était plus fréquente chez les personnes ayant fait des études postsecondaires, celles atteintes de maladies chroniques et celles qui travaillaient dans le domaine des soins de santé. La plupart d’entre elles (80 %) appuieraient un modèle de renonciation au consentement pour les études cliniques à faible risque, citant les avantages médicaux (36 %) et le faible risque perçu (34 %). La majorité des personnes répondantes (77 %) étaient à l’aise à l’idée de participer personnellement à une étude clinique à faible risque. La plupart d’entre elles (80 %) croyaient que les approches fondées sur la renonciation au consentement étaient acceptables. La moitié (52 %) estimaient que le processus de renonciation au consentement devrait fournir des renseignements sur la recherche et inclure la possibilité de se retirer. Lorsqu’on leur a demandé si les participant·es devraient toujours donner un consentement éclairé complet, quel que soit l’aspect pratique ou le niveau de risque, 74 % et 72 % ont répondu par l’affirmative, respectivement.
Conclusion
Il y a un appui public pour les modèles de renonciation au consentement quant à la participation à des études cliniques pragmatiques à faible risque dans les unités de soins intensifs au Canada; cet appui n’est toutefois pas universel. Ces renseignements peuvent éclairer et orienter l’éducation, l’éthique, les politiques et les discussions juridiques sur les modèles de consentement.

Similar content being viewed by others
References
Smith M, Saunders R, Stuckhardt L, McGinnis JM. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, D.C.: National Academies Press; 2013.
Young PJ. Learning healthcare systems will protect patients from unscientific practice variation. Ann Am Thorac Soc 2018; 15: 131–3. https://doi.org/10.1513/annalsats.201709-717ip
Kim SY, Miller FG. Informed consent for pragmatic trials—the integrated consent model. N Engl J Med 2014; 370: 769–72. https://doi.org/10.1056/nejmhle1312508
Faden RR, Beauchamp TL, Kass NE. Informed consent for comparative effectiveness trials. N Engl J Med 2014; 370: 1959–60. https://doi.org/10.1056/nejmc1403310
Murdoch B, Caulfield T. Pragmatic clinical trials and the consent process. Res Ethics 2017; 14: 1–14. https://doi.org/10.1177/1747016117733506
Burns KE, Magyarody NM, Duffett M, Nisenbaum R, Cook DJ. Attitudes of the general public toward alternative consent models. Am J Crit Care 2011; 20: 75–83. https://doi.org/10.4037/ajcc2010645
Government of Canada. Tri-Council policy statement: ethical conduct for research involving humans – TCPS 2 (2022). Available from URL: https://ethics.gc.ca/eng/policy-politique_tcps2-eptc2_2022.html (accessed December 2023).
Government of Alberta. Alberta Health Act; 2014. Available from URL: https://open.alberta.ca/publications/a19p5 (accessed December 2023).
Young PJ, Bagshaw SM, Forbes AB, et al. Effect of stress ulcer prophylaxis with proton pump inhibitors vs histamine-2 receptor blockers on in-hospital mortality among ICU patients receiving invasive mechanical ventilation: the PEPTIC randomized clinical trial. JAMA 2020; 323: 616–26. https://doi.org/10.1001/jama.2019.22190
Sharma A, Minh Duc NT, Lam Thang TL, et al. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med 2021; 36: 3179–87. https://doi.org/10.1007/s11606-021-06737-1
Government of Canada. TCPS 2 (2018)—Chapter 2: scope and approach. Available from URL: https://ethics.gc.ca/eng/tcps2-eptc2_2018_chapter2-chapitre2.html (accessed December 2023).
Opgenorth D, Stelfox HT, Gilfoyle E, et al. Perspectives on strained intensive care unit capacity: a survey of critical care professionals. PLoS One 2018; 13: e0201524. https://doi.org/10.1371/journal.pone.0201524
Burns KE, Zubrinich C, Tan W, et al. Research recruitment practices and critically ill patients. A multicenter, cross-sectional study (the Consent Study). Am J Respir Crit Care Med 2013; 187: 1212–8. https://doi.org/10.1164/rccm.201208-1537oc
Annane D, Outin H, Fisch C, Bellissant E. The effect of waiving consent on enrollment in a sepsis trial. Intensive Care Med 2004; 30: 321–4. https://doi.org/10.1007/s00134-003-2065-8
Ciroldi M, Cariou A, Adrie C, et al. Ability of family members to predict patient's consent to critical care research. Intensive Care Med 2007; 33: 807–13. https://doi.org/10.1007/s00134-007-0582-6
Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005; 171: 987–94. https://doi.org/10.1164/rccm.200409-1295oc
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
Sean M. Bagshaw and Dawn Opgenorth contributed to study concept and design, drafting the manuscript, and statistical analysis. Sean M. Bagshaw contributed to administrative, technical or material support, and supervision. All authors contributed to acquisition, analysis, or interpretation of data and critical revision of the manuscript for important intellectual content.
Acknowledgements
Dr. Bagshaw is supported by a Canada Research Chair in Critical Care Outcomes and Systems Evaluation. The authors would like to thank Blake Murdoch, Health Law Institute, University of Alberta, for his thoughtful review and comments.
Disclosures
The authors have no conflicts of interest to declare.
Funding statement
Funding support was provided by CIHR (2018 Project Grant 399343). The CIHR has no role in the survey design, implementation, analysis, or decision to submit for publication.
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Opgenorth, D., Duquette, D.J., Tyre, L. et al. Public perception of participation in low-risk clinical trials in critical care using waived consent: a Canadian national survey. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02723-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02723-3