Abstract
Purpose
We aimed to elucidate whether postinduction hypotension (PIH), defined as hypotension between anesthesia induction and skin incision, and intraoperative hypotension (IOH) are associated with postoperative mortality.
Methods
We conducted a retrospective cohort study of adult patients with an ASA Physical Status I–IV who underwent noncardiac and nonobstetric surgery under general anesthesia between 2015 and 2021 at Nagoya City University Hospital. The primary and secondary outcomes were 30-day and 90-day postoperative mortality, respectively. We calculated four hypotensive indices (with time proportion of the area under the threshold being the primary exposure variable) to evaluate the association between hypotension (defined as a mean blood pressure < 65 mm Hg) and mortality using multivariable logistic regression models. We used propensity score matching and RUSBoost (random under-sampling and boosting), a machine-learning model for imbalanced data, for sensitivity analyses.
Results
Postinduction hypotension and IOH were observed in 82% and 84% of patients, respectively. The 30-day and 90-day postoperative mortality rates were 0.4% (52/14,210) and 1.0% (138/13,334), respectively. Postinduction hypotension was not associated with 30-day mortality (adjusted odds ratio [aOR], 1.03; 95% confidence interval [CI], 0.93 to 1.13; P = 0.60) and 90-day mortality (aOR, 1.01; 95% CI, 0.94 to 1.07; P = 0.82). Conversely, IOH was associated with 30-day mortality (aOR, 1.19; 95% CI, 1.12 to 1.27; P < 0.001) and 90-day mortality (aOR, 1.12; 95% CI, 1.06 to 1.19; P < 0.001). Sensitivity analyses supported the association of IOH but not PIH with postoperative mortality.
Conclusion
Despite limitations, including power and residual confounding, postoperative mortality was associated with IOH but not with PIH.
Résumé
Objectif
Nous avons cherché à déterminer si l’hypotension post-induction (HPI), définie comme une hypotension entre l’induction de l’anesthésie et l’incision cutanée, et l’hypotension peropératoire (HPO) étaient associées à la mortalité postopératoire.
Méthode
Nous avons mené une étude de cohorte rétrospective de patient·es adultes ayant un statut physique I-IV selon l’ASA et ayant bénéficié d’une chirurgie non cardiaque et non obstétricale sous anesthésie générale entre 2015 et 2021 à l’Hôpital universitaire de la ville de Nagoya. Les critères d’évaluation principal et secondaire étaient la mortalité postopératoire à 30 et 90 jours, respectivement. Nous avons calculé quatre indices d’hypotension (la proportion temporelle de la zone sous le seuil étant la principale variable d’exposition) pour évaluer l’association entre l’hypotension (définie comme une tension artérielle moyenne < 65 mm Hg) et la mortalité à l’aide de modèles de régression logistique multivariée. Nous avons utilisé l’appariement par score de propension et le RUSBoost (sous-échantillonnage et boosting aléatoire), un modèle d’apprentissage automatique pour les données déséquilibrées, pour les analyses de sensibilité.
Résultats
Une HPI et une HPO ont été observées chez 82 % et 84 % des patient·es, respectivement. Les taux de mortalité postopératoire à 30 et 90 jours étaient respectivement de 0,4 % (52/14 210) et de 1,0 % (138/13 334). L’hypotension post-induction n’était pas associée à la mortalité à 30 jours (rapport de cotes ajusté [RCa], 1,03; intervalle de confiance [IC] à 95 %, 0,93 à 1,13; P = 0,60) et à la mortalité à 90 jours (RCa, 1,01; IC 95 %, 0,94 à 1,07; P = 0,82). À l’inverse, l’HPO était associée à une mortalité à 30 jours (RCa, 1,19; IC 95 %, 1,12 à 1,27; P < 0,001) et à la mortalité à 90 jours (RCa, 1,12; IC 95 %, 1,06 à 1,19; P < 0,001). Les analyses de sensibilité ont confirmé l’association de l’HPO, mais pas de l’HPI, avec la mortalité postopératoire.
Conclusion
Malgré les limitations, y compris la puissance et persistance de facteurs confondants, la mortalité postopératoire était associée à l’hypotension peropératoire mais pas à l’hypotension post-induction seule.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intraoperative hypotension (IOH), conventionally defined as mean arterial pressure (MAP) < 60–70 mm Hg or systolic blood pressure (SBP) < 100 mm Hg, is associated with postoperative acute kidney injury (AKI), myocardial injury, and mortality.1,2,3,4,5,6,7,8,9 In two randomized controlled trials, interventions to prevent IOH did not reduce postoperative organ injuries and mortality.10,11
Compared with IOH, postinduction hypotension (PIH) is defined as hypotension occurring between anesthesia induction and skin incision.5 Postinduction hypotension has greatly interested anesthesiologists because it is unaffected by surgery and must be controlled by themselves. Several investigators have attempted to predict PIH using statistical and machine-learning models.12,13,14,15 Unlike IOH, the effect of PIH on postoperative patient outcomes has not been thoroughly examined. To our knowledge, only one study reported that PIH and IOH had a positive correlation with postoperative AKI.5 Thus, whether PIH affects the hardest endpoint, i.e., postoperative mortality, is unclear.
We hypothesized that PIH, as well as IOH, would be associated with postoperative mortality. Thus, we aimed to elucidate the relationship between PIH and postoperative mortality in a retrospective seven-year cohort of a university hospital in Japan. We sought to reduce confounding of PIH on postoperative mortality using propensity score matching (PSM) models. Furthermore, we aimed to use the random under-sampling and boosting (RUSBoost) model, a decision tree type of machine-learning model designed for classifying imbalanced data, to explore the effects of PIH and IOH on mortality.16
Methods
This single-centre retrospective cohort study was approved by the Nagoya City University Graduate School of Medical Sciences and the Nagoya City University Hospital Institutional Review Board (60-21-0155, 15 March 2022). The manuscript adheres to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.17 A data analysis and statistical plan was written after the data were accessed.
Participants
We included adult patients (aged ≥ 18 yr) with an American Society of Anesthesiologists Physical Status (ASA-PS) I–IV who underwent noncardiac and nonobstetric surgery with duration of ≥ 60 min under general anesthesia in Nagoya City University Hospital between January 2015 and December 2021. Additional inclusion criteria were patients without mechanical circulatory support before and during the surgery, patients who experienced 5–120 min of anesthesia induction time, defined as the duration between induction and skin incision,5 and patients who underwent tracheal intubation or supraglottic airway device insertion at least once. After the automated extraction of eligible patients using the anesthesia information management system (AIMS), patients with incorrect data (ASA-PS classification or surgical type) or missing characteristic data were excluded by reviewing the electronic medical records (EMR) according to the following rules. First, patients who underwent surgery for intracranial hemorrhage with mass effect or aortic rupture were reclassified as ASA-PS V and excluded from the study.18 Second, patients who actually underwent cardiac or obstetric surgery were excluded. Finally, patients with missing data (characteristic data, blood pressure [BP] values, or postoperative outcomes) were excluded. If more than one surgical record met the inclusion criteria for the same patient, the most recent one was analyzed.
Data sources
We collected patient data from the EMR, an AIMS (Fortec ORSYS, Koninklijke Philips N.V., Amsterdam, Netherlands), and a diagnosis procedure code (DPC) database of our hospital. All data were obtained between June and December 2022. The DPC database is used for the medical fee billing of inpatients in Japan and has been used in several epidemiological studies.19,20,21 The DPC database includes administrative claims data and patient data, such as diagnoses and comorbidities at admissions identified by the International Classification of Diseases 10th Revision (ICD-10) codes, surgical procedures identified by the Japanese original codes (K codes), and malignancy.20 A previous validation study of the DPC database reported that malignancy has 83.5% sensitivity and 97.7% specificity.22
Variables
Patient characteristics, including age, sex, height, weight, body mass index (BMI), and ASA-PS class, were collected from the AIMS. Outliers in the patient height and weight data with > 3 standard deviations (SDs) were manually checked to determine if they were identical to the EMR data. If the outliers were erroneous and the correct values were obtained from the EMR, they were corrected. In addition, patients with a BMI of 30–40 kg m−2 and those with a BMI ≥ 40 kg m−2 were reclassified to be at least ASA-PS ≥ II and ≥ III, respectively.18 Anesthetic and surgical data, such as duration, emergency surgery, anesthesia type (total intravenous or inhalational), neuraxial anesthesia (epidural or spinal), and peripheral nerve block, were extracted from the EMR and AIMS. Furthermore, the K codes were extracted from the DPC database, and each surgery was classified for three-level risk scores, i.e., low, intermediate, and high risk, defined by the European Society of Cardiology and the European Society of Anaesthesiology.19,23
The most recent blood testing data within 90 days preoperatively were extracted from the EMR. Preoperative medication types were also extracted from the EMR. To calculate the Charlson’s comorbidity index, the ICD-10 codes for comorbidities and malignancies were extracted from the DPC database.24
Endpoints
The primary and secondary endpoints were the 30-day and 90-day mortality, respectively. These endpoints were extracted from the EMR. For patients discharged or transferred to another centre, the last outpatient visit data and mortality records written in the medical information forms from other centres were investigated.
Preprocessing of blood pressure data
Data preprocessing of BP is described in Electronic Supplementary Material (ESM) eAppendix. Hypotension was defined as a MAP below 65 mm Hg.1,2,5,6,7,8 We used absolute values because there was no benefit to using relative rather than absolute thresholds for postoperative organ injuries in a large retrospective study.8 Additionally, we used a threshold of 65 mm Hg based on a systemic review that showed an increased risk of organ injuries with MAP < 65 mm Hg.25 To quantitatively evaluate the degree of hypotension, the following four indices were calculated: duration, time proportion (hypotensive duration divided by the evaluated duration), area under the curve (AUC) of BP values < 65 mm Hg, and the proportion of AUC (AUC divided by the evaluated duration [anesthesia induction time or surgical duration]). The proportion of AUC was defined as the most important exposure because it included the severity and duration of hypotension and was time-adjusted.
Statistical analysis
Data are reported as number (proportion) for categorical data and median [interquartile range] for continuous data. For comparisons of two groups, we used Fisher’s exact test for binomial variables and the Mann–Whitney U test for continuous variables.
Multivariable logistic regression model
As a primary analysis, we used multivariable logistic regression models to reveal the relationship between hypotension and postoperative mortality. No sample size was calculated. The total number of patients in our cohort was expected to be approximately 16,000 cases. Based on recent reports, we assumed that the incidence rates of 30-day and 90-day mortality in our cohort would be 0.3%–0.5% and 0.8%–1.2%, respectively.1,26,27,28 Considering a 10% dropout rate of patients because of missing variables, 30-day and 90-day mortality events were estimated as 40–70 and 100–180, respectively. Considering the model stability, four explanatory variables for 30-day mortality and eight for 90-day mortality classification were included in the logistic regression models.29 From a clinical standpoint and previous literature, age, ASA-PS (dichotomized as ASA-PS < III and ≥ III), emergency, and surgical risk (dichotomized as low risk and others) were initially selected as explanatory variables for the 30-day mortality classification models.14,15 For the 90-day mortality models, age, sex, BMI, ASA-PS (four classes), emergency, surgical risk (three classes), anesthesia type, and neuraxial anesthesia were prespecified.
Sensitivity analyses
We performed sensitivity analyses using the PSM and RUSBoost models for the robustness of the results. Patients whose DPC data were unavailable or whose induction time was < ten minutes were excluded. Missing values of the blood tests were imputed by the mean values.
Propensity score matching model
We compared postoperative mortality rates between the two groups divided by the degree of PIH using PSM. For intuitive understanding and evidence of a significant increase in mortality in MAP < 65 mm Hg for ten minutes,25 patients were divided using the duration of hypotension, i.e., < 10 or ≥ 10 min of PIH. The propensity scores were calculated using 11 patients’ characteristics, 13 types of preoperative medication, 12 types of blood testing data, and Charlson’s comorbidity index score for each 30-day and 90-day mortality model. These 37 variables were determined based on clinical knowledge and previous literature. Propensity score matching was conducted with a 1:1 ratio by nearest-neighbour matching using 0.2 of the caliper width for the SD difference in the propensity scores without replacement.
RUSBoost model
We created machine learning models to predict postoperative mortality in each of the four hypotensive indices, and we evaluated the effects of hypotension using feature importance. As postoperative mortality rates were expected between 0.3% and 1.2% in our cohort, we used the RUSBoost model to classify imbalanced data.16 The RUSBoost algorithm consists of random undersampling and boosting algorithms. In these algorithms, the major class (survivor) is undersampled to a defined ratio to the minor class (deceased), and multiple models are trained sequentially to improve the classification performance. Feature importance measures how much a feature contributes to classifying a target and is used to interpret the relationship among variables.30 To construct RUSBoost models, patients were divided into training and test cohorts with a 7:3 ratio. Hyperparameters such as the learning rate and max depth were determined by GridSearch with five-fold cross-validation. Feature importance values were calculated for the patients’ characteristics and hypotensive indices of PIH and IOH. The performance of the created RUSBoost models for predicting postoperative mortality was assessed by the test data set using precision, recall, geometric mean (G-mean), and area under the precision–recall curve, considering the imbalanced nature of the outcome. The G-mean is the square root of the product of sensitivity (recall) and specificity. In total, 100 repeated trials were performed to precisely evaluate feature importance and model performance.
In addition, we performed sensitivity analyses using different definitions of hypotension and various subgroup analyses. All P values < 0.05 were considered statistically significant. Data preprocessing and model constructions were performed with Python 3.8.13 (Python Software Foundation, Wilmington, DA, USA) and scikit-learn 1.1.1,Footnote 1 and statistical analyses were performed with R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria).
Results
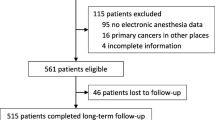
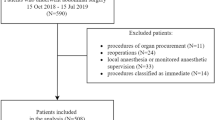
From the AIMS, 16,104 patients with 19,255 surgical records were initially extracted (Fig. 1). After excluding 1,894 patients, 14,210 were finally analyzed (ESM eTable 1). In an overall cohort, 82% and 84% of patients experienced PIH and IOH, respectively. Patient characteristics are shown in Table 1.
The 30-day and 90-day postoperative mortality rates were 0.4% (52/14,210) and 1.0% (138/13,334), respectively. We found no differences in hypotensive indices for PIH between the groups with or without 30-day postoperative mortality (Table 2).
The multivariable logistic regression models revealed that 30-day postoperative mortality positively correlated with IOH (adjusted odds ratio [aOR], 1.19; 95% confidence interval [CI], 1.12 to 1.27; P < 0.001) but not with PIH (aOR, 1.03; 95% CI, 0.93 to 1.13; P = 0.60; Table 3). Moreover, 90-day postoperative mortality was also associated with three out of the four IOH indices but not with PIH.
Sensitivity analyses
For the analyses using the PSM and RUSBoost models, 13,563 patients were included (Fig. 1). Missing blood-test data were imputed by mean values in 8% (1,099/13,563) patients (ESM eTable 2). In the sensitivity analyses of the cohorts, the 30-day and 90-day postoperative mortality rates were 0.4% (48/13,563) and 1.0% (132/12,763), respectively.
Electronic Supplementary Material eTables 3 and 4 show the characteristics before and after the PSM for 30-day and 90-day postoperative mortality. Electronic Supplementary Material eFigs 1–4 show the balance of covariates and the distribution of propensity scores before and after the PSM. After the PSM, we found no differences in 30-day (0.4% vs 0.3%; P = 1) and 90-day (1.1% vs 0.9%; P = 0.38) postoperative mortality between patients who experienced < 10 minutes and ≥ 10 minutes of PIH. Postinduction hypotension duration had sufficiently high correlation coefficients with the other three hypotensive indices (ESM eTable 5).
The performance of the RUSBoost models is summarized in ESM eTable 6. The feature importance values of the RUSBoost model for predicting 30-day and 90-day mortality are shown in Fig. 2 and ESM eFigs 5–11. The feature importance of IOH was higher than that of PIH in all evaluated models (Table 4). The five most important features in the 30-day prediction model using the hypotensive proportion of AUC were albumin, height, age, platelet, and prothrombin international normalized ratio (PT-INR; Fig. 2).
Feature importance of variables in the RUSBoost model for predicting 30-day postoperative mortality using hypotensive proportion of area under the curve. The boxes’ lower and upper edges represent the 25th and 75th percentiles, respectively. The medians are represented by the horizontal lines that run across the boxes. The whiskers represent the lowest and highest values from the 25th and 75th percentiles within a 1.5-box length. Outliers (extreme points beyond whiskers) are shown as dots.
APTT = activated partial thromboplastin time; ASA-PS = American Society of Anesthesiologists Physical Status; BB = beta-blockade; BUN = blood urea nitrogen; BMI = body mass index; CCB = calcium blockade; DM = diabetes mellitus; eGFR = estimated glomerular filtration ratio; IOH = intraoperative hypotension; PIH = post-induction hypotension; PT-INR = prothrombin-international normalized ratio; RAAI = renin-angiotensin-aldosterone system inhibitors; TIVA = total intravenous anesthesia
The results of the other sensitivity analyses are shown in ESM eTables 7–18 and ESM eFigs 12 and 13. Although the age < 60 yr subgroup showed no association between IOH and mortality (ESM eTable 10), the other subgroups showed trends consistent with the main results. The results were also consistent across a range of hypotensive definitions (ESM eTables 12–17).
Discussion
In this study, we evaluated the association between the timing of hypotension and postoperative mortality using a single-centre, seven-year electronic database with 14,210 patients. In the multivariable logistic regression analyses, 30-day and 90-day postoperative mortality rates were associated with IOH but not with PIH. The PSM models and feature importance of the machine-learning models revealed similar trends, thereby supporting the lack of a significant effect of PIH on postoperative mortality.
As opposed to our hypothesis, PIH was not associated with postoperative mortality. Maheshwari et al. reported that PIH and IOH increased the risk of AKI, with increasing duration and AUC of hypotension (MAP < 65 mm Hg).5 The discrepancy between our findings and those of Maheshwari et al. suggests different mechanisms between postoperative mortality and the pathogenesis of AKI. Although postoperative AKI increases mortality,31 other factors such as myocardial injury,32 delirium,33 and respiratory failure,34 can also affect a patient’s prognosis. Postinduction hypotension might have been less associated with prognostic factors other than AKI compared with IOH and did not result in postoperative mortality.
In contrast to PIH, IOH was associated with postoperative mortality, which is consistent with the findings of several studies.1,4,7,9 Thus, PIH and IOH may affect patients differently despite having the same degree of hypotension. The conflicting results between PIH and IOH may be largely due to different causes behind hypotension. Postinduction hypotension is caused by decreased preload and afterload from vasodilation and cardiac depression after the administration of anesthetics. By contrast, IOH is related to various factors, including bleeding, surgical manipulation, and systematic inflammatory response.14 Differentiating the effects of PIH and IOH is crucial in anesthesiology research and practice for physiologic interpretation and management strategy. Our findings suggest the importance of managing circulation by addressing the underlying causes rather than merely maintaining BP levels.
In the PSM models, postoperative mortality was not different between patients with < 10 or ≥ 10 minutes of PIH. Several variables, including patient characteristics, preoperative medications, and blood testing data that could not be used in the primary analysis, were used, and the PSM models were designed to create a pair of patients with similar probabilities of having ≥ 10 minutes of PIH. Thus, we could evaluate the difference in postoperative mortality between patients who experienced or did not experience ≥ 10 minutes of PIH with similar susceptibility to PIH. This reinforces our results that PIH was not associated with mortality even further.
We used a machine-learning algorithm to classify imbalanced data to investigate important variables and predict postoperative mortality. The feature importance values of decision tree-based machine-learning models have been used as explainable artificial intelligence (AI).35 Our models showed that the importance of IOH was greater than that of PIH, supporting our primary analysis. The results for variables with high feature importance are clinically understandable. Mortality increases with advancing age. Being underweight also increases postoperative mortality.36,37 Clinically, albumin, platelet, and PT-INR values may have contributed to mortality prediction, as these values decrease with impaired liver function, chronic inflammation, and aging.38 Consequently, the feature importance of the RUSBoost model provided valid results for interpreting factors contributing to postoperative mortality.
This study has some limitations. First, given the retrospective design, establishing causality between hypotension and mortality was limited. To make causal inferences, we adjusted for possible confounders with PSM and produced clinically interpretable results. Nevertheless, PSM cannot adjust for unselected or unmeasured confounders. For instance, vasopressor and inotrope use, intraoperative fluid volume, and estimated blood loss were not included in the models as these variables could be observed after PIH. Patients with high doses of vasopressors may underestimate hypotensive indices. Second, the single-centre setting and the small number of mortality outcomes are fraught with the potential for selection bias, statistical model instability, and insufficient power. Only a limited number of variables could be put into the logistic regression analyses. Therefore, sensitivity analyses were performed to confirm the robustness of the primary results. Future studies using multicentre or nationwide databases combining laboratory and BP data are warranted. Third, 1,756 patients were excluded because of missing BP values and mortality information, which also led to selection bias. Fourth, the feature importance values for continuous variables tend to be higher than those for categorical variables.39 Thus, categorical variables, such as emergency surgery and surgical risk, should not be compared with continuous variables, such as blood testing values. Finally, physiologic and imaging data, such as electrocardiogram and chest x-ray images, were not used.
Nevertheless, this study has several strengths. First, we examined the previously under-explored relationship between the timing of hypotension and postoperative mortality. Second, PSM models were used for causal inferences and machine-learning models as an explainable AI, and consistent trends in the results were noted. In the sensitivity analyses, as many potentially confounding factors that were electronically available were included, which may strengthen the validity of our findings and facilitate their clinical interpretation. Future studies must establish optimal circulatory management by taking into account the timing of hypotension.
In conclusion, this study revealed that 30-day and 90-day postoperative mortality events were associated with IOH but not with PIH.
Notes
Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: machine learning in Python. J Mach Learn Res 2011; 12: 2825–30. Available from URL: https://scikit-learn.org/stable/about.html#citing-scikit-learn (accessed August 2023).
References
Gregory A, Stapelfeldt WH, Khanna AK, et al. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg 2021; 132: 1654–65. https://doi.org/10.1213/ane.0000000000005250
Ahuja S, Mascha EJ, Yang D, et al. Associations of intraoperative radial arterial systolic, diastolic, mean, and pulse pressures with myocardial and acute kidney injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 2020; 132: 291–306. https://doi.org/10.1097/aln.0000000000003048
Mathis MR, Naik BI, Freundlich RE, et al. preoperative risk and the association between hypotension and postoperative acute kidney injury. Anesthesiology 2020; 132: 461–75. https://doi.org/10.1097/aln.0000000000003063
Mascha EJ, Yang D, Weiss S, Sessler DI. Intraoperative Mean Arterial Pressure Variability and 30-day Mortality in Patients Having Noncardiac Surgery. Anesthesiology 2015; 123: 79–91. https://doi.org/10.1097/aln.0000000000000686
Maheshwari K, Turan A, Mao G, et al. The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: a retrospective cohort analysis. Anaesthesia 2018; 73: 1223–8. https://doi.org/10.1111/anae.14416
Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 2015; 123: 515–23. https://doi.org/10.1097/aln.0000000000000765
Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 2013; 119: 507–15. https://doi.org/10.1097/aln.0b013e3182a10e26
Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 2017; 126: 47–65. https://doi.org/10.1097/aln.0000000000001432
Monk TG, Bronsert MR, Henderson WG, et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 2015; 123: 307–19. https://doi.org/10.1097/aln.0000000000000756
Futier E, Lefrant JY, Guinot PG, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA 2017; 318: 1346–57. https://doi.org/10.1001/jama.2017.14172
Wanner PM, Wulff DU, Djurdjevic M, Korte W, Schnider TW, Filipovic M. Targeting higher intraoperative blood pressures does not reduce adverse cardiovascular events following noncardiac surgery. J Am Coll Cardiol 2021; 78: 1753–64. https://doi.org/10.1016/j.jacc.2021.08.048
Kendale S, Kulkarni P, Rosenberg AD, Wang J. Supervised machine-learning predictive analytics for prediction of postinduction hypotension. Anesthesiology 2018; 129: 675–88. https://doi.org/10.1097/aln.0000000000002374
Lee S, Lee HC, Chu YS, et al. Deep learning models for the prediction of intraoperative hypotension. Br J Anaesth 2021; 126: 808–17. https://doi.org/10.1016/j.bja.2020.12.035
Südfeld S, Brechnitz S, Wagner JY, et al. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth 2017; 119: 57–64. https://doi.org/10.1093/bja/aex127
Reich DL, Hossain S, Krol M, et al. Predictors of hypotension after induction of general anesthesia. Anesth Analg 2005; 101: 622–8. https://doi.org/10.1213/01.ane.0000175214.38450.91
Seiffert C, Khoshgoftaar TM, van Hulse J, Napolitano A. RUSBoost: a hybrid approach to alleviating class imbalance. IEEE Trans Syst 2010; 40: 185–97. https://doi.org/10.1109/TSMCA.2009.2029559
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–7. https://doi.org/10.1016/s0140-6736(07)61602-x
American Society of Anesthesiologists. Statement on ASA Physical Status classification system; 2020. Available from URL: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (accessed August 2023).
Yonekura H, Seto K, Ide K, et al. Preoperative blood tests conducted before low-risk surgery in Japan: a retrospective observational study using a nationwide insurance claims database. Anesth Analg 2018; 126: 1633–40. https://doi.org/10.1213/ane.0000000000002734
Makito K, Matsui H, Fushimi K, Yasunaga H. Volatile versus total intravenous anesthesia for cancer prognosis in patients having digestive cancer surgery. Anesthesiology 2020; 133: 764–73. https://doi.org/10.1097/aln.0000000000003440
Makito K, Mouri H, Matsui H, Michihata N, Fushimi K, Yasunaga H. Spinal epidural hematoma and abscess after neuraxial anesthesia: a historical cohort study using the Japanese Diagnosis Procedure Combination database. Can J Anaesth 2021; 68: 42–52. https://doi.org/10.1007/s12630-020-01827-w
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 2017; 27: 476–82. https://doi.org/10.1016/j.je.2016.09.009
Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management: the Joint Task Force on Non-cardiac Surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 2014; 35: 2383–431. https://doi.org/10.1093/eurheartj/ehu282
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173: 676–82. https://doi.org/10.1093/aje/kwq433
Wesselink EM, Kappen TH, Torn HM, Slooter AJ, van Klei WA. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth 2018; 121: 706–21. https://doi.org/10.1016/j.bja.2018.04.036
Lee SW, Lee HC, Suh J, et al. Multi-center validation of machine learning model for preoperative prediction of postoperative mortality. NPJ Digit Med 2022; 5: 91. https://doi.org/10.1038/s41746-022-00625-6
Dony P, Seidel L, Pirson M, Haller G. Common clinical thresholds of intraoperative hypotension and 30-day mortality following surgery: a retrospective cohort study. Acta Anaesthesiol Scand 2020; 64: 1388–96. https://doi.org/10.1111/aas.13670
Chiew CJ, Liu N, Wong TH, Sim YE, Abdullah HR. Utilizing machine learning methods for preoperative prediction of postsurgical mortality and intensive care unit admission. Ann Surg 2020; 272: 1133–9. https://doi.org/10.1097/sla.0000000000003297
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373–9. https://doi.org/10.1016/s0895-4356(96)00236-3
Puchner WF, Dünser MW, Paulus P, et al. A comparative study on adequate anesthesia depth: clinical judgement and the Narcotrend® measurement. Can J Anesth 2020; 67: 664–73. https://doi.org/10.1007/s12630-020-01602-x
Prowle JR, Forni LG, Bell M, et al. Postoperative acute kidney injury in adult non-cardiac surgery: joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative. Nat Rev Nephrol 2021; 17: 605–18. https://doi.org/10.1038/s41581-021-00418-2
Devereaux PJ, Biccard BM, Sigamani A, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2017; 317: 1642–51. https://doi.org/10.1001/jama.2017.4360
Pedemonte JC, Sun H, Franco-Garcia E, et al. Postoperative delirium mediates 180-day mortality in orthopaedic trauma patients. Br J Anaesth 2021; 127: 102–9. https://doi.org/10.1016/j.bja.2021.03.033
Ayad S, Khanna AK, Iqbal SU, Singla N. Characterisation and monitoring of postoperative respiratory depression: current approaches and future considerations. Br J Anaesth 2019; 123: 378–91. https://doi.org/10.1016/j.bja.2019.05.044
Lundberg SM, Erion G, Chen H, et al. From local explanations to global understanding with explainable AI for trees. Nat Mach Intell 2020; 2: 56–67. https://doi.org/10.1038/s42256-019-0138-9
Woo SH, Cha DH, Park EC, Kim SJ. The association of under-weight and obesity with mortality after hip arthroplasty. Age Ageing 2019; 48: 94–100. https://doi.org/10.1093/ageing/afy161
Hu WH, Cajas-Monson LC, Eisenstein S, Parry L, Cosman B, Ramamoorthy S. Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 2015; 14: 91. https://doi.org/10.1186/s12937-015-0081-5
Mahmud N, Fricker Z, Hubbard RA, et al. Risk Prediction models for post-operative mortality in patients with cirrhosis. Hepatology 2021; 73: 204–18. https://doi.org/10.1002/hep.31558
Strobl C, Boulesteix AL, Zeileis A, Hothorn T. Bias in random forest variable importance measures: illustrations, sources and a solution. BMC Bioinformatics 2007; 8: 25. https://doi.org/10.1186/1471-2105-8-25
Author contributions
TN contributed to the study conceptualization, study design, data acquisition, data analysis, data interpretation, and manuscript drafting. TT, YS, HH, and KF contributed to the study design, data analysis, data interpretation, and reviewing and revising the manuscript. KS contributed the study conceptualization, study design, data interpretation, and reviewing and revising the manuscript.
Acknowledgments
The authors would like to thank the staff of the Medical Affairs Division of Nagoya City University Hospital for data extraction and Enago (www.enago.jp) for the English language review.
Disclosures
None.
Funding statement
None.
Prior conference presentations
Part of the study was presented at the 70th Annual Meeting of the Japanese Society of Anesthesiologists (1–3 June 2023, Kobe, Japan).
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nakanishi, T., Tsuji, T., Sento, Y. et al. Association between postinduction hypotension and postoperative mortality: a single-centre retrospective cohort study. Can J Anesth/J Can Anesth 71, 343–352 (2024). https://doi.org/10.1007/s12630-023-02653-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02653-6