Abstract
Purpose
Postoperative atrial fibrillation (POAF) is a common complication following cardiac surgery. Although the evidence suggests that beta blockers prevent POAF, they often cause hypotension. Landiolol, an ultra-short-acting β1 blocker, may prevent POAF, without adverse hemodynamic consequences.
Source
We searched MEDLINE, CENTRAL, Embase, and trial registries between January 1970 and March 2022. We included randomized controlled trials (RCTs) that evaluated the effect of landiolol for the prevention of POAF after cardiac surgery. Two reviewers independently assessed eligibility, extracted data, and assessed risk of bias using the Risk of Bias 2.0 tool. We pooled data using random-effects models. We used the Grading of Recommendations, Assessment, Development and Evaluations framework to assess certainty of evidence.
Principal findings
Nine RCTs including 868 participants met the eligibility criteria. Patients randomized to landiolol (56/460) had less POAF compared with controls (133/408) with a relative risk (RR) of 0.40 (95% confidence interval [CI], 0.30 to 0.54; I2 = 0%;) and an absolute risk of 12.2% vs 32.6% (absolute risk difference, 20.4%; 95% CI, 15.0 to 25.0). Landiolol resulted in a shorter hospital length-of-stay (LOS) (268 patients; mean difference, −2.32 days; 95% CI, −4.02 to −0.57; I2 = 0%). We found no significant difference in bradycardia (RR, 1.11; 95% CI, 0.48 to 2.56; I2 = 0%). No hypotension was reported with landiolol. We judged the certainty of evidence as moderate for POAF (because of indirectness as outcomes were not clearly defined) and low for LOS (because of imprecision and concern of reporting bias).
Conclusion
In patients undergoing cardiac surgery, landiolol likely reduces POAF and may reduce LOS. A definitive large RCT is needed to confirm these findings.
Study registration
PROSPERO (CRD42021262703); registered 25 July 2021.
Résumé
Objectif
La fibrillation auriculaire postopératoire (FAPO) est une complication fréquente après une chirurgie cardiaque. Bien que les données probantes suggèrent que les bêta-bloqueurs préviennent la FAPO, ces agents provoquent souvent une hypotension. Le landiolol, un β1-bloqueur à action ultra-courte, pourrait prévenir la FAPO sans conséquences hémodynamiques indésirables.
Sources
Nous avons effectué des recherches dans les bases de données MEDLINE, CENTRAL et Embase, et dans les registres d’études publiées entre janvier 1970 et mars 2022. Nous avons inclus les études randomisées contrôlées (ERC) évaluant l’effet du landiolol pour la prévention de la FAPO après une chirurgie cardiaque. Deux personnes ont indépendamment révisé l’éligibilité, extrait les données et évalué le risque de biais à l’aide de l’outil Risque de biais 2.0. Nous avons regroupé les données à l’aide de modèles à effets aléatoires. Nous avons utilisé le système de notation GRADE (Grading of Recommendations Assessment, Development, and Evaluation) pour évaluer la certitude des données probantes.
Constatations principales
Neuf ERC incluant 868 personnes remplissaient les critères d’éligibilité. Les patient·es randomisé·es dans le groupe landiolol (56/460) présentaient moins de FAPO que les témoins (133/408), avec un risque relatif (RR) de 0,40 (intervalle de confiance [IC] à 95 %, 0,30 à 0,54; I2 = 0 %) et un risque absolu de 12,2 % vs 32,6 % (différence de risque absolue, 20,4 %; IC 95 % 95 %, 15,0 à 25,0). Le landiolol a entraîné une durée de séjour hospitalier plus courte (268 patient·es; différence moyenne, −2,32 jours; IC 95 %, −4,02 à −0,57; I2 = 0 %). Nous n’avons trouvé aucune différence significative en matière de bradycardie (RR, 1,11; IC 95 %, 0,48 à 2,56; I2 = 0 %). Aucune hypotension n’a été rapportée avec le landiolol. Nous avons jugé que la certitude des données probantes était modérée pour la FAPO (en raison du caractère indirect car les critères d’évaluation n’étaient pas clairement définis) et faible pour la durée de séjour hospitalier (en raison de l’imprécision et de questionnements concernant le biais de déclaration).
Conclusion
Chez les patient·es bénéficiant d’une chirurgie cardiaque, le landiolol réduit probablement la FAPO et peut réduire la durée de séjour hospitalier. Une ERC définitive à grande échelle est nécessaire pour confirmer ces résultats.
Enregistrement de l’étude
PROSPERO (CRD42021262703); enregistrée le 25 juillet 2021.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Atrial fibrillation (AF) is the most common perioperative complication following cardiac surgery. The incidence of postoperative atrial fibrillation (POAF) is as high as 30% following isolated coronary artery bypass graft (CABG), and 40% following valvular surgery; the incidence increases up to 50% in combined CABG and valvular surgery.1,2 Postoperative atrial fibrillation is associated with an increased risk of postoperative adverse events such as stroke, all-cause mortality, and increased length of hospital stay (LOS).3,4,5
A recent Cochrane systematic review of cardiac surgery randomized controlled trials (RCTs) reported that patients on beta blocker therapy had a lower risk of POAF compared with control, (relative risk, 0.50; 95% confidence interval [CI], 0.42 to 0.59; I2 = 59%); however, the evidence was rated as low certainty because several studies had a high risk of bias and a moderate level of statistical heterogeneity that was not explained through subgroup analysis.6 Moreover, there was uncertainty about safety.6 For example, perioperative beta blockers had a relative risk of 1.84 (95% CI, 0.89 to 3.80; I2 = 0%) for perioperative hypotension, but the evidence was rated as moderate because several studies had a high risk of bias.6
Landiolol is an ultra-short-acting intravenous β1 blocker that is highly cardioselective.7 Its action peaks within ten minutes and its offset occurs between 20 and 30 min.7 Compared with other beta blockers, landiolol’s increased negative chronotropic effect, less potent negative inotropic effect, and rapid offset make it an appealing pharmacologic option in the perioperative setting for preventing or treating POAF, while potentially avoiding important hypotension and its consequences.8 We undertook a systematic review to summarize and appraise the existing evidence of landiolol to prevent POAF following cardiac surgery.
Methods
This systematic review and meta-analysis was performed in accordance with the Cochrane Handbook for Systematic Reviews and Interventions and reported following the PRISMA statement for meta-analysis in health care interventions.9 The study protocol was registered in the international prospective register of systematic reviews (PROSPERO: CRD42021262703).
Eligibility criteria
We included RCTs of perioperative landiolol (i.e., intraoperative or postoperative administration) vs control in adults undergoing cardiac surgery (i.e., CABG, valvular, CABG and valvular). We included trials if they reported any of our prespecified outcomes. We excluded trials that randomized patients after POAF occurred; trials that included patients < 18 yr of age (unless the results for patients ≥ 18 yr of age were available); or trials evaluating the effect of landiolol compared with another active medication (e.g., amiodarone). We also excluded trials that were exclusive to patients with pre-existing AF. There were no restrictions on language or date of publication, and we included trials published as full manuscripts or conference abstracts.
Literature search
We worked with a senior librarian to develop a search strategy. We searched MEDLINE (Electronic Supplementary Material [ESM] eTable 1), Embase (ESM eTable 2), and CENTRAL (ESM eTable 3) databases for relevant articles published from January 1970 until March 2022. ClinicalTrials.gov and the EU Clinical Trials Register were searched for completed nonpublished trials. We reviewed previously published systematic reviews to include all original studies that met our inclusion criteria. We used the following keywords to conduct our systematic search: cardiac surgery, landiolol hydrochloride, short-acting beta blockers, adrenergic beta-antagonists, adrenergic β1 receptor antagonists, rapibloc, randomized, and randomized control trial. Electronic Supplementary Material eFigs 1–3 present further details of the search strategy.
Study selection
Our search output was imported to Covidence.org. Two independent reviewers (T. C. and M. A.) screened titles and abstracts in duplicate to determine possible eligibility. The citations selected during the screening process underwent full-text review in duplicate by two independent reviewers to determine eligibility for our systematic review. Any disagreement during both abstract screening and full-text review were resolved by consensus.
Data collection and quality assessment
Two independent reviewers (T. C. and L. P.) undertook data extraction and assessed the quality of the included studies. We recorded event rates and reported relative risks (RRs) of all trial outcomes. We recorded LOS in days and reported the mean difference. We used the Risk of Bias 2.0 tool (RoB2) to assess the quality of trials included in this systematic review.10 The RoB2 tool is structured into five domains of bias (randomization, deviation from intended intervention, missing data, measurement of outcomes, and selection of the reported results). A series of questions and prompts aim to elicit a proposed judgement about the risk of bias arising from each domain. Judgement can be “low” or “high” risk of bias or can express “some concerns” of bias.
We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to assess the certainty of evidence for each of the prespecified outcomes, and this was determined in duplicate. The evidence rating for the studies was graded according to the five GRADE considerations (risk of bias, inconsistency, indirectness, imprecision, and publication bias) to rate the certainty of evidence for each outcome as high, moderate, low, or very low certainty.11 Evidence from RCTs starts at high certainty and can be downgraded for several reasons.
Study outcomes
We evaluated events up to 30 days after surgery. The primary outcome was the incidence of POAF. We report the definition of POAF used in each study in the Table. Secondary individual outcomes included hospital LOS, all-cause mortality, myocardial infarction (MI), and congestive heart failure (CHF), as defined by study authors. Safety outcomes included the incidence of hypotension (mean arterial pressure ≤ 65), bradycardia (heart rate ≤ 50 beats per min), and stroke.
Statistical analysis
We performed statistical analyses using Review Manager (RevMan) V.5.3.3 (Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark). For dichotomous outcomes, we calculated a Mantel–Haenszel pooled RR with 95% CI. For the continuous outcome of hospital LOS (days), we calculated the 95% CI and the mean differences and the absolute difference of the mean number of days spent in hospital between the landiolol and control group. We used random effects models to pool the results across trials for each outcome.
We quantified the degree of heterogeneity using the I2 index. We viewed any I2 ≥ 30% as representing meaningful heterogeneity. We undertook subgroup analyses to explore possible explanations of heterogeneity.12 Our a priori potential explanations for heterogeneity included: high vs some concerns vs low risk of bias (we expected the lower quality trials to have a larger treatment effect); high landiolol infusion rate (i.e., ≥ 2 µg·kg–1·min–1) vs lower infusion rate (we expected the higher infusion rate to have a larger treatment effect); landiolol treatment throughout the intraoperative and postoperative period vs landiolol treatment not throughout these periods (we expected landiolol treatment throughout the perioperative period to have a larger treatment effect). We also undertook subgroup meta-analyses according to the type of cardiac surgery (e.g., isolated CABG; isolated valve surgery; combined CABG and valve surgery). For our primary outcome of POAF, we visually inspected funnel plots to explore for the potential presence of publication bias.
Results
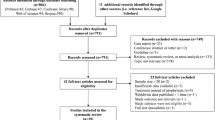
The literature search identified a total of 998 unique citations (ESM eFig. 1). After all titles and abstracts were screened, the full texts of 32 citations were further assessed to determine eligibility. Based on eligibility criteria, nine RCTs were included in our review.13,14,15,16,17,18,19,20,21 We included eight published manuscripts13,14,15,16,17,18,20,21 and one conference abstract.19
Characteristics of included studies
The characteristics of the nine included trials are described in the Table. These RCTs were published between 2012 and 2020 and included a total of 868 patients. Five studies focused on isolated CABG (n = 473 patients),14,15,16,17,20 and four studies focused on combined CABG and valve surgery (n = 395 patients).13,18,19,21 Two studies compared landiolol to placebo (saline infusion).15,16 Seven studies compared landiolol to control.13,14,17,18,19,20,21 The definition of POAF was variable as described in the Table. All patients were monitored in an intensive care unit. In all trials, heart rate and rhythm were monitored continuously for the duration of the follow-up period (from three to seven days). Eight studies were conducted in Japan13,14,15,17,18,19,20,21 and one in France.16
Risk of bias
Three of nine trials were judged to be at low risk of bias (Fig. 1).13,14,15 Five trials were deemed to have some risk of bias.16,17,18,19,20 One trial was determined to be at high risk of bias because of significant differences in baseline characteristics between the landiolol and control groups.21 Two trials did not disclose how the randomization process was conducted.17,19 Three trials were rated down from low risk of bias to some concerns of bias as they did not provide a pre-established statistical analysis plan (Fig. 1).16,18,20
Primary outcome—postoperative atrial fibrillation
For the landiolol vs control comparison, the outcome POAF (189 events among 868 patients) was reported in all RCTs, and landiolol showed a reduction in POAF; (RR, 0.40; 95% CI, 0.30 to 0.54; I2 = 0%) (Fig. 2).13,14,15 Based on the GRADE framework, we determined the certainty of the evidence for this outcome to be moderate because of indirectness based on poor outcome definition (ESM eTable 4). Due to the limited number of trials, the funnel plot could not exclude publication bias (ESM eFigs 2a and 2b). Subgroup analyses based on type of surgery, duration of infusion, concentration of infusion and risk of bias showed similar treatment effects of landiolol on POAF (ESM eFigs 3–7 and eTable 5).
Secondary outcomes
Length of hospital stay
Three trials that included 268 patients reported data on LOS.13,14,15 Length of hospital stay was significantly lower in the landiolol group (mean, 12.53 days) vs the control group (15.20 days) (mean difference, −2.32 days; 95% CI, −4.02 to −0.57; I2 = 0%) (Fig. 3).13,14,15 We judged the quality of evidence to be low. This judgement was based on imprecision and concern for potential reporting bias (ESM eTable 4).
Mortality
Three trials reported the occurrence of all-cause mortality.13,14,15 The risk of mortality during hospitalization was not significantly different with landiolol (six events; 268 patients; RR, 0.37; 95% CI, 0.07 to −1.97; I2 = 0%; absolute risk difference [ARD], 3.0%; 95% CI, −1.0 to 7.0) (Fig. 4). We judged the evidence to be very low-certainty because of very serious imprecision and indirectness because the follow-up period was shorter than 30 days (ESM eTable 4).
Congestive heart failure
Two trials reported the occurrence of CHF.14,15 There was no significant difference in the risk of CHF with landiolol (three events; 208 patients; RR, 0.26, 95% CI, 0.03 to −2.27; I2 = 0%; ARD 3.0%; 95% CI, −1.0 to 7.0) (Fig. 5). We judged the quality of the evidence for this outcome to be very low certainty because of indirectness and imprecision as the outcome was not defined (ESM eTable 4).
Myocardial infarction
Two trials reported the occurrence of MI.13,14 The risk of MI was not significantly different with landiolol (two events; 128 patients; RR, 1.0; 95% CI, 0.11 to 9.35; I2 = 0%; ARD, 0.0%; 95% CI, −6.0 to 7.0) (Fig. 6). We judged the quality of evidence for this outcome as be very low-certainty because of imprecision and indirectness as the outcome was not defined (ESM eTable 4).
Stroke
Two trials reported the occurrence of stroke.13,15 There was no significant difference in the risk of stroke with landiolol (three events; 200 patients; RR, 0.62; 95% CI, 0.08 to 4.96; I2 = 0%; ARD, 1.0%; 95% CI, −3.0 to 4.0) (Fig. 7). We judged the quality of evidence for this outcome as very low certainty because of imprecision and indirectness as the outcome was not defined (ESM eTable 4).
Potential adverse effects
Bradycardia
Three trials reported the occurrence of bradycardia.11,12,17 There was no significant difference in the risk of bradycardia with landiolol (19 events; 384 patients; RR, 1.11; 95% CI, 0.48 to −2.56; I2 = 0%; ARD, 1.11; 95% CI, 0.48 to 2.56) (Fig. 8). We judged the quality of evidence for this outcome as low because of imprecision (ESM eTable 4).
Hypotension
Two trials reported the occurrence of hypotension11,12 (zero events; n = 416 patients). As no hypotension events were recorded, the RR and risk difference could not be estimated. The GRADE quality assessment was very low as the outcome was poorly defined and no events were reported (ESM eTable 4).
Discussion
Statement of principal findings
In this systematic review of RCTs, we found that the use of prophylactic landiolol in cardiac surgery resulted in a significantly and clinically meaningful reduction in the occurrence of POAF compared with control. Landiolol was also associated with a significant reduction of hospital LOS. Safety data were seldomly reported. The overall quality of evidence was rated as low to moderate because of small trial sizes and resultant imprecision.
Study in relation to other studies
Using beta blockers to prevent POAF following cardiac surgery is recommended by the European Association of Cardiothoracic Anesthesiology and European Society of Cardiology guidelines.22,23 Despite these recommendations, a multinational survey of cardiac anesthesiologists showed divergent practices with the risk for bradycardia cited as the most common barrier to pre- and intraoperative use of beta blockers.22 Landiolol being a highly β1 selective agent with a short half-life, could potentially be a safe alternative.
A recently published systematic review and meta-analysis evaluated the effectiveness and safety of landiolol in both cardiac (n = 646) and noncardiac surgeries.24 The RR (0.27; 95% CI, 0.18 to 0.40) represents data from two observational studies and six RCTs. Our systematic review included three more RCTs and showed an updated RR (0.40; 95% CI, 0.30 to 0.54) for POAF reduction with landiolol compared with a prior systematic review.22,24 To our knowledge, this is the largest systematic review of RCTs (n = 868) evaluating the effectiveness and safety of landiolol in patients undergoing cardiac surgery, and the only one to assess the quality and certainty of evidence. In our systematic review, POAF in the control group was 32.6%, similar to previous reports.22,24
Interpretation
Postoperative atrial fibrillation after cardiac surgery is associated with both clinical and patient-important outcomes including increased risk of mortality, stroke, longer hospital LOS, and readmission to hospital.3,4,5 Compared with other rate-controlling drugs, landiolol has the advantage of being ultra-short acting, allowing for more rapid reversal of adverse effects, making it a potentially appealing pharmacologic option for the prevention of POAF.
Larger studies have indicated that patients who develop AF after cardiac surgery have a longer hospital stay compared with those who do not.25 A Cochrane systematic review of perioperative beta blockers for preventing complications after cardiac surgery reported little or no difference in hospital LOS according to whether perioperative beta blockers were administered (mean difference, −1.21 days; 95% CI, −2.75 to 0.33; I2 = 66%; n = 404) but rated the evidence as very low certainty.6 The authors downgraded the evidence because several studies had a high risk of bias, a moderate level of statistical heterogeneity, and imprecision resulting from too few studies with few patients.6 Landiolol’s effect on LOS is encouraging and there is a need for more research regarding how this translates to cost effectiveness.
To date, no large scale RCT has been conducted to evaluate the safety and efficacy of landiolol in preventing POAF in cardiac surgery. Although landiolol has encouraging physiologic properties and preliminary trial data, all of the perioperative landiolol trials have been small (i.e., < 200 patients). The results presented in our meta-analysis are promising, and a definitive, large, high-quality, multicentre RCT is needed.
Limitations
Our study has several limitations associated mostly with the restricted availability of outcome data. Our study was primarily limited by the lack of relevant outcome data on adverse effects. Secondary outcomes were rarely reported in the included studies, which limited the certainty of the evidence. Only three included studies were rated as having a low risk of bias; however, subgroup analysis based on risk of bias (low vs some concerns vs high risk of bias) did not show significant differences in effect size. Most included trials (8/9) were conducted in Japan, raising the question of generalizability to other patient populations.13,14,15,17,18,19,20,21 Results of numerous in vitro studies suggest that genetic polymorphisms may contribute to variability in response to beta blockers; however, discordance among results prevents reliable conclusions on the influence of receptor genotypes on the clinical use of beta blockers.26,27
Conclusion
In this systematic review, the use of prophylactic landiolol in cardiac surgery led to a large reduction of POAF and a shorter LOS compared with controls. There were no obvious differences in side effects such as hypotension, bradycardia, and mortality, but there were too few events to draw firm conclusions.
Although landiolol has encouraging physiologic properties and preliminary trial data, all the perioperative landiolol trials have been small (i.e., < 200 patients) and require confirmation in a large, high-quality, multicentre trial to establish both efficacy and safety. Future trials designed to systematically capture clinically important primary and associated secondary outcomes are needed.
References
Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol 2008; 51: 793–801. https://doi.org/10.1016/j.jacc.2007.10.043
Mathew JP, Fontes ML, Tudor IC, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA 2004; 291: 1720–9. https://doi.org/10.1001/jama.291.14.1720
Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol 2004; 43: 742–8. https://doi.org/10.1016/j.jacc.2003.11.023
Conen D, Wang MK, Devereaux PJ, et al. New-onset perioperative atrial fibrillation after coronary artery bypass grafting and long-term risk of adverse events: an analysis from the coronary trial. J Am Heart Assoc 2021; 10: e020426. https://doi.org/10.1161/jaha.120.020426
Wang MK, Meyre PB, Heo R, et al. Short-term and long-term risk of stroke in patients with perioperative atrial fibrillation after cardiac surgery: systematic review and meta-analysis. CJC Open 2021; 4: 85–96. https://doi.org/10.1016/j.cjco.2021.09.011
Blessberger H, Lewis SR, Pritchard MW, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing non-cardiac surgery. Cochrane Database Syst Rev 2019; 9: CD-13438. https://doi.org/10.1002/14651858.cd013438
Syed YY. Landiolol: a review in tachyarrhythmias. Drugs 2018; 78: 377–88. https://doi.org/10.1007/s40265-018-0883-9
Li L, Ai Q, Lin L, Ge P, Yang C, Zhang L. Efficacy and safety of landiolol for prevention of atrial fibrillation after cardiac surgery: a meta-analysis of randomized controlled trials. Int J Clin Exp Med 2015; 8: 10265–73.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372 : n71. https://doi.org/10.1136/bmj.n71
Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: I4898. https://doi.org/10.1136/bmj.l4898
Santesso N, Glenton C, Dahm P, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 2020; 119: 126–35. https://doi.org/10.1016/j.jclinepi.2019.10.014
Deeks JJ, Higgins JP, Altman DC. Chapter 10: analysing data and undertaking meta-analyses. Available from URL: https://training.cochrane.org/handbook/current/chapter-10 (accessed April 2023).
Sezai A, Osaka S, Yaoita H, et al. Safety and efficacy of landiolol hydrochloride for prevention of atrial fibrillation after cardiac surgery in patients with left ventricular dysfunction: prevention of atrial fibrillation after cardiac surgery with landiolol hydrochloride for left ventricular dysfunction (PLATON) trial. J Thorac Cardiovasc Surg 2015; 150: 957–64. https://doi.org/10.1016/j.jtcvs.2015.07.003
Sezai A, Nakai T, Hata M, et al. Feasibility of landiolol and bisoprolol for prevention of atrial fibrillation after coronary artery bypass grafting: a pilot study. J Thorac Cardiovasc Surg 2012; 144: 1241–8. https://doi.org/10.1016/j.jtcvs.2012.06.042
Sezai A, Minami K, Nakai T, et al. Landiolol hydrochloride for prevention of atrial fibrillation after coronary artery bypass grafting: new evidence from the PASCAL trial. J Thorac Cardiovasc Surg 2011; 141: 1478–87. https://doi.org/10.1016/j.jtcvs.2010.10.045
Ferraris A, Jacquet-Lagrèze M, Cazenave L, et al. Microcirculatory effects of landiolol: a double-blind, randomised, controlled study after cardiac surgery. Br J Anaesth 2021; 126: e212–4. https://doi.org/10.1016/j.bja.2021.03.013
Fujii M, Bessho R, Ochi M, Shimizu K, Terajima K, Takeda S. Effect of postoperative landiolol administration for atrial fibrillation after off pump coronary artery bypass surgery. J Cardiovasc Surg (Torino) 2012; 53: 369–74.
Sakaguchi M, Sasaki Y, Hirai H, et al. Efficacy of landiolol hydrochloride for prevention of atrial fibrillation after heart valve surgery. Int Heart J 2012; 53: 359–63. https://doi.org/10.1536/ihj.53.359
Osada H, Nakajima H, Masuyama S, Morishima M, Su T. Landiolol hydrochloride: prevention of atrial fibrillation after open-heart surgery. Eur Heart H 2014; 12; https://doi.org/10.1093/eurheartj/ehs281
Ogawa S, Okawa Y, Goto Y, Aoki M, Baba H. Perioperative use of a beta blocker in coronary artery bypass grafting. Asian Cardiovasc Thorac Ann 2013; 21: 265–9. https://doi.org/10.1177/0218492312451166
Sasaki K, Kumagai K, Maeda K, et al. Preventive effect of low-dose landiolol on postoperative atrial fibrillation study (PELTA study). Gen Thorac Cardiovasc Surg 2020; 68: 1240–51. https://doi.org/10.1007/s11748-020-01364-9
Tamura T, Yatabe T, Yokoyama M. Prevention of atrial fibrillation after cardiac surgery using low-dose landiolol: a systematic review and meta-analysis. J Clin Anesth 2017; 42: 1–6. https://doi.org/10.1016/j.jclinane.2017.07.009
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 2021; 42: 373–498. https://doi.org/10.1093/eurheartj/ehaa612
Hao J, Zhou J, Xu W, et al. Beta-blocker landiolol hydrochloride in preventing atrial fibrillation following cardiothoracic surgery: a systematic review and meta-analysis. Ann Thorac Cardiovasc Surg 2022; 28: 18–31. https://doi.org/10.5761/atcs.ra.21-00126
Norhayati MN, Bahari IS, Zaharah S, Hazlina NH, Aimanazrul ZM, Irfan M. Metoprolol for prophylaxis of postoperative atrial fibrillation in cardiac surgery patients: systematic review and meta-analysis. BMJ Open 2020; 10: e038364. https://doi.org/10.1136/bmjopen-2020-038364
Sasaguri T, Shiraishi F, Yoshihara T, Takahashi-Yanaga F, Morimoto S. β1-adrenergic receptor gene polymorphisms and the acute response to atenolol in healthy young Japanese subjects. J Pharmacol Sci 2011; 115: 490–9. https://doi.org/10.1254/jphs.10332fp
Shin J, Johnson JA. Pharmacogenetics of beta-blockers. Pharmacotherapy 2007; 27: 874–87. https://doi.org/10.1592/phco.27.6.874
Author contributions
All authors contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Disclosures
All authors have no financial or personal conflicts of interest that could influence the content or interpretation of the manuscript. Additionally, the research discussed in the article has been conducted in an ethical and responsible manner.
Funding statement
We received an unrestricted grant from Trimedic Therapeutics that supported conducting our systematic review and meta-analysis. The sponsor was not involved in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Prior conference presentations
40th International Symposium on Intensive Care on Emergency Medicine 2021 (31 August–3 September, Brussels, Belgium).
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cafaro, T., Allwood, M., McIntyre, W.F. et al. Landiolol for the prevention of postoperative atrial fibrillation after cardiac surgery: a systematic review and meta-analysis. Can J Anesth/J Can Anesth 70, 1828–1838 (2023). https://doi.org/10.1007/s12630-023-02586-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02586-0