Abstract
Purpose
Older adults with COVID-19 have a high prevalence of complications and mortality during hospitalization. Given the large proportion of older adults requiring admission to an intensive care unit (ICU), we aimed to describe the management and outcomes of older adults with COVID-19 requiring ICU care and identify predictors of hospital mortality.
Methods
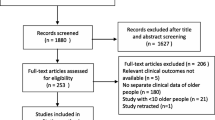
We included consecutive patients ≥ 65 yr of age who were admitted between 11 March 2020 and 30 June 2021 to one of five Toronto (ON, Canada) ICUs with a primary diagnosis of SARS-CoV-2 infection in a retrospective cohort study. Patient characteristics, ICU treatment, and outcomes were recorded. We used multivariable logistic regression to identify predictors of in-hospital mortality.
Results
Of the 273 patients, the median [interquartile range] age was 74 [69–80] yr, 104 (38.1%) were female, and 164 (60.1%) required invasive mechanical ventilation. One hundred and forty-two patients (52.0%) survived their hospital stay. Compared with survivors, nonsurvivors were older (74 [70–82] yr vs 73 [68–78] yr; P = 0.03), and a smaller proportion was female (39/131, 29.8% vs 65/142, 45.8%; P = 0.01). Patients had long hospital (19 [11–35] days) and ICU (9 [5–22] days) stays, with no significant differences in ICU length of stay or duration of invasive mechanical ventilation between the two groups. Higher APACHE II score, increasing age, and the need for organ support were independently associated with higher in-hospital mortality while female sex was associated with lower mortality.
Conclusions
Older critically ill COVID-19 patients had long ICU and hospital stays, and approximately half died in hospital. Further research is needed to identify individuals who will benefit most from an ICU admission and to evaluate posthospitalization outcomes.
Résumé
Objectif
Les personnes âgées atteintes de la COVID-19 ont une prévalence élevée de complications et de mortalité pendant l’hospitalisation. Compte tenu de la forte proportion de personnes âgées nécessitant une admission dans une unité de soins intensifs (USI), nous avons cherché à décrire la prise en charge et les devenirs des personnes âgées atteintes de COVID-19 nécessitant des soins intensifs et à identifier les prédicteurs de mortalité hospitalière.
Méthode
Nous avons inclus des patient·es consécutif·ves âgé·es de ≥ 65 ans admis·es entre le 11 mars 2020 et le 30 juin 2021 dans l’une des cinq unités de soins intensifs de Toronto (ON, Canada) avec un diagnostic primaire d’infection par le SRAS-CoV-2 dans une étude de cohorte rétrospective. Les caractéristiques des patient·es, le traitement en USI et les devenirs ont été enregistrés. Nous avons utilisé une régression logistique multivariable pour identifier les prédicteurs de mortalité hospitalière.
Résultats
Parmi les 273 patient·es, l’âge médian [écart interquartile] était de 74 [69-80] ans, 104 (38,1 %) étaient des femmes et 164 (60,1 %) ont nécessité une ventilation mécanique invasive. Cent quarante-deux personnes (52,0 %) ont survécu à leur séjour à l’hôpital. Comparativement aux personnes survivantes, les personnes qui n’ont pas survécu étaient plus âgées (74 [70-82] ans vs 73 [68–78] ans; P = 0,03), et une plus faible proportion était de sexe féminin (39/131, 29,8 % vs 65/142, 45,8 %; P = 0,01). Les séjours des patient·es à l’hôpital (19 [11-35] jours) et à l’USI (9 [5-22] jours) étaient longs, sans différence significative dans la durée du séjour en USI ou la durée de la ventilation mécanique invasive entre les deux groupes. Un score APACHE II plus élevé, un âge plus avancé et le besoin de mesures de soutien d’organes étaient indépendamment associés à une mortalité plus élevée à l’hôpital, tandis que le sexe féminin était associé à une mortalité plus faible.
Conclusion
Les personnes plus âgées gravement malades atteintes de la COVID-19 ont eu de longs séjours en soins intensifs et à l’hôpital, et environ la moitié sont décédées à l’hôpital. D’autres recherches sont nécessaires pour identifier les personnes qui bénéficieraient le plus d’une admission à l’USI et pour évaluer les devenirs post-hospitalisation.
Similar content being viewed by others
References
Wong EK, Watt J, Zou H, et al. Mortality in hospitalized older adults with COVID-19 during three waves: a multicenter retrospective cohort study. Health Sci Rep 2022; 5: e603. https://doi.org/10.1002/hsr2.603
Canadian Institute for Health Information. COVID-19 hospitalization and emergency department statistics, 2023. Available from URL: https://www.cihi.ca/en/covid-19-hospitalization-and-emergency-department-statistics (accessed February 2023).
Pun BT, Badenes R, La Calle GH, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med 2021; 9: 239–50. https://doi.org/10.1016/s2213-2600(20)30552-x
Chang R, Elhusseiny KM, Yeh YC, Sun WZ. COVID-19 ICU and mechanical ventilation patient characteristics and outcomes—a systematic review and meta-analysis. PLoS One 2021; 16: e0246318. https://doi.org/10.1371/journal.pone.0246318
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–7. https://doi.org/10.7326/0003-4819-147-8-200710160-00010
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–81. https://doi.org/10.1016/j.jbi.2008.08.010
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–95. https://doi.org/10.1503/cmaj.050051
Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 1998; 26: 1793–800. https://doi.org/10.1097/00003246-199811000-00016
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315: 801–10. https://doi.org/10.1001/jama.2016.0287
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818–29.
Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001; 29: 1370–9. https://doi.org/10.1097/00003246-200107000-00012
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med 2001; 27: 859–64. https://doi.org/10.1007/s001340100909
Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST Jr, Leslie DL, Agostini JV. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc 2005; 53: 312–8. https://doi.org/10.1111/j.1532-5415.2005.53120.x
Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth 2019; 22: 67–72. https://doi.org/10.4103/aca.aca_157_18
Vallet H, Schwarz GL, Flaatten H, de Lange DW, Guidet B, Dechartres A. Mortality of older patients admitted to an ICU: a systematic review. Crit Care Med 2021; 49: 324–34. https://doi.org/10.1097/ccm.0000000000004772
Modra L, Higgins A, Vithanage R, Abeygunawardana V, Bailey M, Bellomo R. Sex differences in illness severity and mortality among adult intensive care patients: a systematic review and meta-analysis. J Crit Care 2021; 65: 116–23. https://doi.org/10.1016/j.jcrc.2021.05.019
Simpson A, Puxty K, McLoone P, Quasim T, Sloan B, Morrison DS. Comorbidity and survival after admission to the intensive care unit: a population-based study of 41,230 patients. J Intensive Care Soc 2021; 22: 143–51. https://doi.org/10.1177/1751143720914229
Flaatten H, De Lange DW, Morandi A, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med 2017; 43: 1820–8. https://doi.org/10.1007/s00134-017-4940-8
Bingold TM, Lefering R, Zacharowski K, et al. Individual organ failure and concomitant risk of mortality differs according to the type of admission to ICU—a retrospective study of SOFA score of 23,795 patients. PLoS One 2015; 10: e0134329. https://doi.org/10.1371/journal.pone.0134329
GitHub. mice: Multivariate imputation by chained equations. Available from URL: https://github.com/amices/mice (accessed February 2023).
The R Foundation. The R project in statistical computing. Available from URL: https://www.R-project.org/ (accessed February 2023).
Gkoufa A, Maneta E, Ntoumas GN, et al. Elderly adults with COVID-19 admitted to intensive care unit: a narrative review. World J Crit Care Med 2021; 10: 278–89. https://doi.org/10.5492/wjccm.v10.i5.278
Xu J, Yang X, Yang L, et al. Clinical course and predictors of 60-day mortality in 239 critically ill patients with COVID-19: a multicenter retrospective study from Wuhan, China. Crit Care 2020; 24: 394. https://doi.org/10.1186/s13054-020-03098-9
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323: 1574–81. https://doi.org/10.1001/jama.2020.5394
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–81. https://doi.org/10.1016/s2213-2600(20)30079-5
Alshukry A, Ali H, Ali Y, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) patients in Kuwait. PLoS One 2020; 15: e0242768. https://doi.org/10.1371/journal.pone.0242768
Aleva FE, van Mourik L, Broeders ME, Paling AJ, de Jager CP. COVID-19 in critically ill patients in North Brabant, the Netherlands: patient characteristics and outcomes. J Crit Care 2020; 60: 111–5. https://doi.org/10.1016/j.jcrc.2020.08.001
Larsson E, Brattström O, Agvald-Öhman C, et al. Characteristics and outcomes of patients with COVID-19 admitted to ICU in a tertiary hospital in Stockholm, Sweden. Acta Anaesthesiol Scand 2021; 65: 76–81. https://doi.org/10.1111/aas.13694
Dres M, Hajage D, Lebbah S, et al. Characteristics, management, and prognosis of elderly patients with COVID-19 admitted in the ICU during the first wave: insights from the COVID-ICU study: prognosis of COVID-19 elderly critically ill patients in the ICU. Ann Intensive Care 2021; 11: 77. https://doi.org/10.1186/s13613-021-00861-1
Galbadage T, Peterson BM, Awada J, et al. Systematic review and meta-analysis of sex-specific COVID-19 clinical outcomes. Front Med 2020; 7: 348. https://doi.org/10.3389/fmed.2020.00348
Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res 2020; 116: 2197–206. https://doi.org/10.1093/cvr/cvaa284
Williamson CA, Faiver L, Nguyen AM, Ottenhoff L, Rajajee V. Incidence, predictors and outcomes of delirium in critically ill patients with COVID-19. Neurohospitalist 2022; 12: 31–7. https://doi.org/10.1177/19418744211034815
Mendes A, Herrmann FR, Périvier S, Gold G, Graf CE, Zekry D. Delirium in older patients with COVID-19: prevalence, risk factors, and clinical relevance. J Gerontol A Biol Sci Med Sci 2021; 76: e142–6. https://doi.org/10.1093/gerona/glab039
Oxenbøll-Collet M, Egerod I, Christensen V, Jensen J, Thomsen T. Nurses’ and physicians’ perceptions of confusion assessment method for the intensive care unit for delirium detection: focus group study. Nurs Crit Care 2018; 23: 16–22. https://doi.org/10.1111/nicc.12254
Klein S, Mayer D. Choosing Wisely Canada recommendations. Can Fam Physician 2017; 63: e473.
Lonardo NW, Mone MC, Nirula R, et al. Propofol is associated with favorable outcomes compared with benzodiazepines in ventilated intensive care unit patients. Am J Respir Crit Care Med 2014; 189: 1383–94. https://doi.org/10.1164/rccm.201312-2291oc
Aragón RE, Proaño A, Mongilardi N, et al. Sedation practices and clinical outcomes in mechanically ventilated patients in a prospective multicenter cohort. Crit Care 2019; 23: 130. https://doi.org/10.1186/s13054-019-2394-9
Author contributions
Eric K. C. Wong, Jennifer Watt, Richard Norman, Katrina Piggott, Sharon E. Straus, Barbara Liu, and Sangeeta Mehta contributed to the study conception and design. Data collection was performed by Kiyan Heybati, Eric K. C. Wong, Hanyan Zou, Arthana Chandraraj, and Alissa W. Zhang. Data analysis was performed by Eric Kai-Chung Wong. The first draft of the manuscript was written by Kiyan Heybati, Eric K. C. Wong, and Sangeeta Mehta and all authors commented on previous versions of the manuscript.
Disclosures
None.
Funding statement
Academic Health Science Centre Alternate Funding Plans Innovative Funds from Unity Health Toronto; Sinai Health/University Health Network Healthy Ageing and Geriatrics Program and its Geriatrics Summer Scholars Program; Division of Geriatric Medicine and General Internal Medicine, Sunnybrook Health Sciences Centre. The sponsor has no role in this study’s design, method, patient recruitment, data collection, analysis, or the manuscript. SES is funded by a Tier 1 Canada Research Chair. EKW is funded by the Clinician Scientist Training Program at the University of Toronto and the Vanier Scholarship from the Canadian Institutes of Health Research.
Prior conference presentations
Dr. Heybati presented this research at the Critical Care Canada Forum (28 November–1 December 2022, Toronto, ON, Canada).
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12630_2023_2518_MOESM1_ESM.pdf
Supplementary file1 (PDF 705 KB)—eTable 1 STROBE checklist. eTable 2 Additional ventilatory interventions and parameters, stratified by hospital outcome. eFig. 1 Lowest PaO2/FIO2 ratio on ICU days 1 to 7. eFig. 2 Median tidal volume on ICU days 1 to 7. eFig. 3 Lowest arterial pH on ICU days 1 to 7. eFig. 4 Lowest arterial pH on ICU days 1 to 7. eFig. 5 Highest plateau pressure on ICU days 1 to 7. eFig. 6 Lowest mean arterial pressure on ICU days 1 to 7.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heybati, K., Wong, E.K.C., Watt, J. et al. Outcomes of critically ill older adults with COVID-19: a multicentre retrospective cohort study. Can J Anesth/J Can Anesth 70, 1371–1380 (2023). https://doi.org/10.1007/s12630-023-02518-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02518-y