Abstract
Purpose
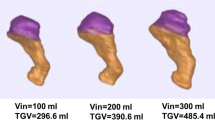
Surgical patients are asked to adhere to preoperative fasting guidelines to minimize gastric contents. Large fluid volumes or solid content can still be present as shown with gastric ultrasound. It has been suggested that additional rating of patients’ satiety, measured as the feeling of hunger and thirst, could help clinicians to better judge emptying of the stomach.
Methods
We performed a prospective observational study in fasted elective surgical patients. The primary objective was to investigate the correlation between hunger measured on a 0–10 numeric rating scale and total gastric fluid volume measured with gastric ultrasonography. Secondary objectives included the correlation between 1) thirst and total gastric fluid volume and 2) hunger, thirst, and the Perlas grading scale score.
Results
We included 515 patients. The exam was inconclusive in 14 individuals (2.7%). The Spearman correlation coefficient between gastric fluid volumes and hunger was 0.11 (95% confidence interval [CI], 0.02 to 0.20) (P = 0.01). The correlation between gastric fluid volumes and thirst was 0.11 (95% CI, 0.02 to 0.20) (P = 0.02). Between antral grades and numeric rating scale, the correlation coefficient was 0.00 (95% CI, −0.09 to 0.09) (P = 1.00) for thirst and 0.00 (95% CI, −0.08 to 0.09) (P = 0.94) for hunger. Ten patients (2.0%) had solid content, 24 presented a grade 2 antrum (4.8%).
Conclusion
This study suggests that the correlation between total gastric fluid volume and satiety sensation is very weak. Satiety did not reliably predict total gastric fluid volume.
Study registration
ClinicalTrials.gov (NCT04884373); registered 13 May 2021.
Résumé
Objectif
On demande aux patient·es de chirurgie de respecter les directives de jeûne préopératoire afin de minimiser leur contenu gastrique. Comme le montre l’échographie gastrique, de grands volumes de liquide ou des solides peuvent encore être présents. Il a été suggéré qu’une évaluation supplémentaire de la satiété des patient·es, mesurée par la sensation de faim et de soif, pourrait aider les clinicien·nes à mieux estimer la vidange de l’estomac.
Méthode
Nous avons réalisé une étude observationnelle prospective chez des patient·es de chirurgie non urgente à jeun. L’objectif principal était d’étudier la corrélation entre la faim mesurée sur une échelle d’évaluation numérique de 0 à 10 et le volume total de liquide gastrique mesuré par échographie gastrique. Les objectifs secondaires comprenaient la corrélation entre 1) la soif et le volume total de liquide gastrique et 2) la faim, la soif et le score de l’échelle de classement Perlas.
Résultats
Nous avons inclus 515 personnes. L’examen était non concluant chez 14 individus (2,7 %). Le coefficient de corrélation de Spearman entre les volumes de liquide gastrique et la faim était de 0,11 (intervalle de confiance [IC] à 95 %, 0,02 à 0,20) (P = 0,01). La corrélation entre les volumes de liquide gastrique et la soif était de 0,11 (IC 95 %, 0,02 à 0,20) (P = 0,02). Entre les grades antraux et l’échelle d’évaluation numérique, le coefficient de corrélation était de 0,00 (IC 95 %, -0,09 à 0,09) (P = 1,00) pour la soif et de 0,00 (IC 95 %, -0,08 à 0,09) (P = 0,94) pour la faim. Un contenu solide a été observé chez dix personnes (2,0 %), et 24 présentaient un antre de grade 2 (4,8 %).
Conclusion
Cette étude suggère que la corrélation entre le volume total de liquide gastrique et la sensation de satiété est très faible. La satiété n’a pas permis de prédire de manière fiable le volume total de liquide gastrique.
Enregistrement de l’étude
clinicaltrials.gov (NCT04884373); enregistrée le 13 mai 2021.



Similar content being viewed by others
References
Van de Putte P, Vernieuwe L, Jerjir A, Verschueren L, Tacken M, Perlas A. When fasted is not empty: a retrospective study in fasted surgical patients. Br J Anaesth 2017; 118: 363–71. https://doi.org/10.1093/bja/aew435
Bouvet L, Desgranges FP, Aubergy C, et al. Prevalence and factors predictive of full stomach in elective and emergency surgical patients: a prospective cohort study. Br J Anaesth 2017; 118: 372–9. https://doi.org/10.1093/bja/aew462
Weiji Q, Shitong L, Yu L, Tianfang H, Ning K, Lina Z. The predictive value of hunger score on gastric evacuation after oral intake of carbohydrate solution. BMC Anesthesiol 2018; 18: 6. https://doi.org/10.1186/s12871-018-0470-3
Janssen P, Vanden Berghe P, Verschueren S, Lehmann A, Depoortere I, Tack J. Review article: the role of gastric motility in the control of food intake. Aliment Pharmacol Ther 2011; 33: 880–94. https://doi.org/10.1111/j.1365-2036.2011.04609.x
Stribiţcaia E, Evans CE, Gibbons C, Blundell J, Sarkar A. Food texture influences on satiety: systematic review and meta-analysis. Sci Rep 2020; 10: 12929. https://doi.org/10.1038/s41598-020-69504-y
Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth 2014; 113: 12–22. https://doi.org/10.1093/bja/aeu151
Perlas A, Van de Putte P, Van Houwe P, Chan VW. I-AIM framework for point-of-care gastric ultrasound. Br J Anaesth 2016; 116: 7–11. https://doi.org/10.1093/bja/aev113
Perlas A, Mitsakakis N, Liu L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination. Anesth Analg 2013; 116: 357–63. https://doi.org/10.1213/ane.0b013e318274fc19
Kruisselbrink R, Arzola C, Jackson T, Okrainec A, Chan V, Perlas A. Ultrasound assessment of gastric volume in severely obese individuals: a validation study. Br J Anaesth 2017; 118: 77–82. https://doi.org/10.1093/bja/aew400
Arzola C, Perlas A, Siddiqui NT, Downey K, Ye XY, Carvalho JC. Gastric ultrasound in the third trimester of pregnancy: a randomised controlled trial to develop a predictive model of volume assessment. Anaesthesia 2018; 73: 295–303. https://doi.org/10.1111/anae.14131
Perlas A, Davis L, Khan M, Mitsakakis N, Chan VW. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg 2011; 113: 93–7. https://doi.org/10.1213/ane.0b013e31821b98c0
May JO, Looney SW. Sample size charts for Spearman and Kendall coefficients. J Biom Biostat 2020; 11; 1–7. https://doi.org/10.37421/jbmbs.2020.11.440
Swinscow TD. Statistics at Square One: correlation and regression. Available from: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression (accessed December 2022).
Hveem K, Jones KL, Chatterton BE, Horowitz M. Scintigraphic measurement of gastric emptying and ultrasonographic assessment of antral area: relation to appetite. Gut 1996; 38: 816–21. https://doi.org/10.1136/gut.38.6.816
Jones KL, Doran SM, Hveem K, et al. Relation between postprandial satiation and antral area in normal subjects. Am J Clin Nutr 1997; 66: 127–32. https://doi.org/10.1093/ajcn/66.1.127
Sturm K, Parker B, Wishart J, et al. Energy intake and appetite are related to antral area in healthy young and older subjects. Am J Clin Nutr 2004; 80: 656–67. https://doi.org/10.1093/ajcn/80.3.656
Van de Putte P, Perlas A. The link between gastric volume and aspiration risk. In search of the Holy Grail? Anaesthesia 2018; 73: 274–9. https://doi.org/10.1111/anae.14164
Perlas A, Arzola C, Van de Putte P. Point-of-care gastric ultrasound and aspiration risk assessment: a narrative review. Can J Anesth 2018; 65: 437–48. https://doi.org/10.1007/s12630-017-1031-9
Forde CG. Measuring satiation and satiety. In: Ares G, Varela P (Eds.). Methods in Consumer Research: Alternative Approaches and Special Applications (Vol. 2). Duxford: Woodhead Publishing; 2018: 151–82. https://doi.org/10.1016/B978-0-08-101743-2.00007-8
Kruisselbrink R, Arzola C, Endersby R, Tse C, Chan V, Perlas A. Intra- and interrater reliability of ultrasound assessment of gastric volume. Anesthesiology 2014; 121: 46–51. https://doi.org/10.1097/aln.0000000000000193
Deemer SE, Plaisance EP, Martins C. Impact of ketosis on appetite regulation-a review. Nutr Res 2020; 77: 1–11. https://doi.org/10.1016/j.nutres.2020.02.010
Ni D, Smyth HE, Cozzolino D, Gidley MJ. integrating effects of human physiology, psychology, and individual variations on satiety–an exploratory study. Front Nutr 2022; 9: 872169. https://doi.org/10.3389/fnut.2022.872169
Author contributions
Peter Van de Putte contributed to study design, data collection, data interpretation, writing and revision of the manuscript, and approval of the final manuscript. Anneleen Herijgers, An Wallyn, and Lisa Van Dyck contributed to data collection, writing and revision of the manuscript, and approval of the final manuscript. Tom Bleeser contributed to statistical analysis, interpretation of data, writing and revising the manuscript, and approval of the final manuscript. Brecht Calle, Jenny del Jesus Sanchez Fernandez, Fikriye Dogrul, and Ellen Hendrickx contributed to data collection, revision of the manuscript, and approval of the final manuscript.
Acknowledgements
The authors want to thank Tom Cattaert, MSc, PhD and Sara Van de Putte, MSc, for their help with the statistical analysis.
Disclosures
No conflicts of interests to declare.
Funding statement
No funding.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an Editorial. Please see Can J Anesth 2023; https://doi.org/10.1007/s12630-023-02507-1.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van de Putte, P., Herijgers, A., Wallyn, A. et al. The correlation between patient satiety sensation and total gastric fluid volume: a prospective observational study. Can J Anesth/J Can Anesth 70, 1307–1314 (2023). https://doi.org/10.1007/s12630-023-02508-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02508-0