Abstract
Purpose
Limited data exist on advanced critical care echocardiography (CCE) training programs for intensivists. We sought to describe a longitudinal echocardiography program and investigate the effect of distributed conditional supervision vs predefined en-bloc supervision, as well as the effect of an optional echocardiography laboratory rotation, on learners’ engagement.
Methods
In this mixed methods study, we enrolled critical care fellows and faculty from five University of Toronto-affiliated intensive care units (ICU) between July 2015 and July 2018 in an advanced training program, comprising theoretical lectures and practical sessions. After the first year, the program was modified with changes to supervision model and inclusion of a rotation in the echo laboratory. We conducted semistructured interviews and investigated the effects of curricular changes on progress toward portfolio completion (150 transthoracic echocardiograms) using a Bayesian framework.
Results
Sixty-five learners were enrolled and 18 were interviewed. Four (9%) learners completed the portfolio. Learners reported lack of time and supervision, and skill complexity as the main barriers to practicing independently. Conditional supervision was associated with a higher rate of submitting unsupervised echocardiograms than unconditional supervision (rate ratio, 1.11, 95% credible interval, 1.08 to 1.14). After rotation in the echocardiography laboratory, submission of unsupervised echocardiograms decreased.
Conclusion
Trainees perceived lack of time and limited access to supervision as major barriers to course completion. Nevertheless, successful portfolio completion was related to factors other than protected time in the echocardiography laboratory or unconditional direct supervision in ICU. Further research is needed to better understand the factors promoting success of CCE training programs.
Résumé
Objectif
Il n’existe que peu de données sur les programmes de formation avancés en échocardiographie pour les soins intensifs (écho-USI) destinés aux intensivistes. Nous avons cherché à décrire un programme longitudinal d’échocardiographie et à étudier l’effet d’une supervision conditionnelle distribuée vs une supervision prédéfinie en bloc, ainsi que l’effet d’une rotation facultative en laboratoire d’échocardiographie, sur le niveau d’implication des apprenants.
Méthode
Dans cette étude à méthodes mixtes, nous avons recruté des fellows en soins intensifs et des professeurs de cinq unités de soins intensifs (USI) affiliées à l’Université de Toronto entre juillet 2015 et juillet 2018 pour participer à un programme de formation avancée comprenant des conférences théoriques et des séances pratiques. Après la première année, le programme a été modifié en apportant des changements au modèle de supervision et en incluant une rotation dans le laboratoire d’écho. Nous avons mené des entretiens semi-structurés et étudié les effets des changements du programme d’études sur les progrès vers la réussite de la formation (150 échocardiogrammes transthoraciques) en utilisant un cadre bayésien.
Résultats
Soixante-cinq apprenants étaient inscrits et 18 ont été interviewés. Quatre (9 %) apprenants ont complété la formation. Les apprenants ont signalé que le manque de temps et de supervision ainsi que la complexité des compétences constituaient les principaux obstacles à une pratique autonome. La supervision conditionnelle était associée à un taux plus élevé de soumission d’échocardiogrammes non supervisés que la supervision inconditionnelle (ratio de taux, 1,11, intervalle crédible à 95 %, 1,08 à 1,14). Après la rotation dans le laboratoire d’échocardiographie, la soumission d’échocardiogrammes non supervisés a diminué.
Conclusion
Les stagiaires ont perçu le manque de temps et l’accès limité à la supervision comme des obstacles majeurs à la réussite de la formation. Néanmoins, l’achèvement du cours était lié à des facteurs autres que le temps protégé au laboratoire d’échocardiographie ou la supervision directe inconditionnelle aux soins intensifs. D’autres recherches sont nécessaires pour mieux comprendre les facteurs favorisant le succès des programmes de formation en écho-USI.
Similar content being viewed by others
Critical care echocardiography (CCE) is a noninvasive diagnostic tool that has, in many countries, largely replaced invasive cardiovascular monitoring.1,2 International consensus panels agree that all intensivists should be able to perform basic CCE.3,4,5,6,7,8 Major professional societies in Europe and North America have implemented certification processes to assess intensivists’ competencies in CCE.9,10,11,12 Achieving proficiency in CCE has thus become a key component of safe critical care practice, yet the optimal path for intensivists to master the skill remains unknown.13,14,15
While many European countries have fully integrated echocardiography into critical care clinical practice and training, other countries, especially in North America, continue to depend on cardiology services to perform and interpret CCE. A major barrier to CCE uptake in North America is the lack of CCE-certified staff intensivists.16,17 Without certified intensivists providing longitudinal supervision, trainees may not achieve competence and may interpret CCE findings erroneously, thereby potentially compromising patient care.18 Numerous publications have reported on the successful implementation of short CCE workshops and basic curricula in critical care and emergency medicine, but the literature on advanced CCE training remains scarce.19,20,21,22,23,24,25,26 There are concerns that short, basic CCE courses are inadequate for safe clinical practice.13,14,15,27,28,29 Yet, a paucity of evidence informs the design of advanced CCE training, despite the recent development of international certifications in Europe and North America.10,11,18 Only a few authors have reported the implementation of advanced CCE programs.16,21,22
We developed and implemented a longitudinal echocardiography training program for advanced CCE, based on recommendations from professional societies and principles of curriculum design.30,31,32,33 The primary objective of the present work was to evaluate our advanced CCE program to better understand reasons for low completion rates. Our secondary objective was to assess if two curricular changes implemented after the first year of the program increased program completion. The curricular changes that we investigated were 1) distributed supervised CCE sessions conditional to learners’ independent practice (vs predefined supervised blocks) and 2) an optional echocardiography laboratory (echo lab) rotation.18
Methods
Initial structure of and subsequent changes to the echocardiography training program
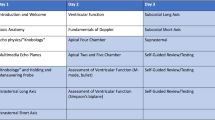
The advanced CCE program took place within the Interdepartmental Division of Critical Care Medicine (IDCCM) of the University of Toronto (Toronto, ON, Canada), which is composed of approximately 70 attending physicians with different specialty backgrounds (e.g., anesthesiology, internal medicine) and 70 senior critical care trainees (fellows) per year. Only two IDCCM attending physicians were formally trained to perform CCE, and only one was certified for advanced CCE. Enrollment in the course was voluntary. The advanced CCE program consisted of a combination of theoretical and practical components (Table 1). Practical sessions included independent (unsupervised) and supervised hands-on practice in the intensive care unit (ICU). Learners submitted unsupervised CCE electronically. To complete the program, each learner had to collect a portfolio of 150 transthoracic echocardiograms with their corresponding reports (as per international recommendations)11,30,34 and attend at least half of the didactic sessions (see Electronic Supplementary Material [ESM] eAppendix 1 for additional details). The portfolio could comprise both unsupervised and supervised echocardiograms, including those performed in the echo lab. All echocardiograms submitted were reviewed and graded according to previously published scales.35 Reports generated by the learners were also reviewed. For learners aiming to obtain international certification, echocardiograms submitted as part of our training program were included in the learner’s portfolio required for international certification. The practical component of the training was tailored to the learners’ previous experience. Learners without previous experience were introduced to basic CCE and progressed to advanced CCE throughout the training. Low engagement and shortage of instructors during year 1 led us to modify the program for subsequent iterations in two ways. First, we optimized hands-on CCE practice by adopting a distributed conditional supervision model. To increase independent practice with delayed feedback (i.e., aiming toward “deliberate practice”), we required submission of a minimal number of unsupervised echocardiograms every month to “earn” access to direct supervision (Table 1).36,37,38,39,40,41,42,43 In year 2, 15 monthly echocardiograms’ submission allowed learners to access as many supervised sessions as available; in year 3, one two-hour supervised session could be obtained for each seven echocardiograms submitted. We hypothesized that this change would increase learners’ motivation to practice independently between supervised sessions, while optimizing our educational resource use. Additionally, based on concepts in psychomotor learning, we distributed the supervision over time (one- to two-hour sessions throughout the year upon request, Fig. 1) instead of using a massed practice schedule (i.e., one- to two-week blocks of supervised practice each year).44,45 Second, we provided an opportunity to complete an optional two- to four-week rotation in the echo lab, where learners could practice on cardiology outpatients under supervision of a sonographer. Learners could choose to complete a rotation in the echo lab (by using one of their critical care program elective blocks) if spots were available for noncardiology trainees.
Distribution of supervised practice over the three years of implementation. The first year offered en-bloc supervision of one week at a time (two in total throughout the year). Supervision was organized based on the learner’s schedule and instructors’ availability. For the subsequent years, supervised practice was divided in multiple two-hour sessions. Only learners who had submitted echocardiograms for review by the instructors were offered supervised sessions.
Study design, participants, and setting
This prospective cohort study followed a multiphase, convergent mixed methods design with the purpose of triangulation and complementarity. The study was conducted within the IDCCM of the University of Toronto. All IDCCM fellows and staff physicians who enrolled in the advanced CCE program between September 2015 and June 2018 were eligible to participate in the evaluation study if they attended more than three didactic sessions. Learners who did not have a portfolio requirement (i.e., attending physicians during year 1) were excluded from the analysis. Study participation was voluntary. Quantitative and qualitative data (with equal priority) were collected between September 2015 and June 2018. Approval from the Institutional Research and Ethics Board was obtained, and participants gave written informed consent.
Qualitative analysis: exposure, outcomes, and analyses
We conducted semistructured interviews of a purposeful sample of consenting physicians who either completed or did not fully complete the program between 2015 and 2018 (see ESM eAppendix 2). We performed a purposive sampling to achieve maximum variation.46,47 Two investigators (L. D., A. J.) who were not course instructors conducted all interviews, which were audio-recorded and transcribed verbatim. We began inductive content analysis of the deidentified transcripts immediately and classified the findings into themes, subthemes, and matched quotes. We categorized interviews according to the interviewees’ level of engagement using their number of echocardiograms submitted for review (low: < 50 CCE, moderate: 50 to 100, and high: > 100 CCE). Our initial set of 12 interviews included learners from years 1 to 3 but failed to capture learners who had submitted a large number of echocardiograms. We then purposefully recruited such learners to expand our understanding of learners’ engagement (theoretical sampling). We modified the interview guide iteratively to include questions pertaining to emerging themes such as the experience in the echo lab. One of the authors (G. D.) conducted an inductive thematic content analysis of the transcripts by performing line-by-line coding and identifying emerging themes. A second researcher (D. P.) also coded the initial transcripts. Preliminary interpretations were reviewed, discussed, and agreed upon between the two co-investigators. As the qualitative analysis progressed, certain interpretations of the transcripts called for additional quantitative analyses as aforementioned. Interpretations also raised questions about the role of motivation in learners’ engagement with the program. An exploration of motivational theories informed a subsequent deductive analysis of the data set. The interview process was discontinued when data saturation was reached.48,49,50 Both investigators reflected, throughout the research process, on their position as clinician, educator, and teacher, and its impact on the analyses.
Quantitative analysis
For the quantitative analyses, we collected attendance and number of echocardiograms performed independently and under supervision. We used descriptive statistics to report the primary outcome, which was program completion defined as attendance of more than 50% of the theoretical sessions and completion of 150 echocardiograms (supervised and unsupervised). In the secondary analyses, we estimated the effects of conditional vs unconditional supervision on the rate of submission of unsupervised echocardiograms. Furthermore, we calculated the effect of an echo lab rotation on the submission rate of unsupervised echocardiograms. Analyses were conducted with a Bayesian framework using R (Version 3.5.3) and JAGS (Version 4.3.0).51 Further details are described in ESM eAppendix 3.
Results
Learners’ characteristics, engagement level, and program completion rate
Sixty-five learners enrolled in the program between September 2015 and June 2018. We excluded 14 learners (22%) who attended less than three didactic sessions, and six learners (9%) without CCE portfolio requirements (ICU attendings from year 1). A total of 45 learners (69%) were included in the final analysis. In total (including unsupervised, supervised, and echo lab echocardiograms), learners performed a median [interquartile range] of 32 [14–83] echocardiograms over the course of their enrollment in the program. Eight learners (17%) performed a total of ≥ 100 echocardiograms in a year. Four of these eight learners had previously performed less than 50 CCEs, and two had no previous CCE experience. Fourteen learners (31%) completed a rotation in the echo lab. Four learners (9%) completed their portfolio (one within a year, and three within three years) and attended more than 50% of the didactic sessions, thereby fulfilling criteria for program completion. Eleven learners eventually wrote a certifying examination with a success rate of 100%. One wrote the European Diploma of Echocardiography and ten wrote the Examination of Special Competence in Critical Care Examination of the American National Board of Echocardiography (CCEeXAM); of note, the first iteration of the CCEeXAM took place in January 2019. The four learners who completed their portfolio are now diplomates of the CCEeXAM (i.e., passed the CCEeXAM and performed at least 150 complete transthoracic CCEs). An illustration of the study profile and details on participant characteristics are reported in Fig. 2 and Tables 2 and 3.
Qualitative analysis of learners’ perceptions of the program
We conducted 18 individual interviews. The following abbreviations are used to describe the quotes: interviewee (I), fellow (F), attending (A), and cohort (C), with cohorts defined as cohort 1 (academic year 2015–2016), cohort 2 (2016–2017), and cohort 3 (2017–2018). Low, moderate, and high refers to engagement with independent practice as aforementioned. Quantified qualitative data are summarized in ESM eTable 1. Additional quotes are reported in ESM eTable 2.
Enrolling in a critical care echocardiography course with great expectations
Learners viewed echocardiography as an essential tool to assess and manage critically ill patients. They stated three main reasons to enroll: 1) to perform echocardiography independently from cardiologists, 2) to monitor patient’s clinical changes and responses to treatments, and 3) to use a noninvasive technique.
“I really want to know what happens [with my patients] and I feel there's a lot of constraint when I rely on other people” (I-13: F/C2-3/moderate).
Certain learners chose an advanced CCE program to mitigate potential risks of superficial CCE learning, while others aimed to prepare for a formal certification. This was perceived as an advantage in a competitive employment market.
“There are risks with any diagnostic modality if their use is inappropriate […] you need some form of standards, an expertise to be able to do it and interpret it. Otherwise, it may easily give you a false sense of security” (I-15: F/C2/high).
“The reality is that most people who do this course are more interested in all aspects of critical care and in passing the exam and getting certified” (I-13, F/C3/moderate).
Facing the reality of learning a complex skill in a challenging environment
Learners unanimously mentioned the lack of protected time as a significant barrier to training.
“It was not just the course; it was everything else that was going on at the same time. You know … there was lots of things going on like … work and academic work and personally as well” (I-10, F/C2/moderate).
Learners also commented on the complexity of learning echocardiographic skills for critically ill patients, whose anatomical and physiologic dynamic changes complicated acquisition and interpretation of images. Learners reported a range of negative emotions, such as frustration and stress, while practicing independently in the ICU. In addition, they felt infantilized and punished by the conditional access to supervision based on independent practice.
“It was also hard because if you were doing the sessions on your own, you’d just get the view and after 10 minutes you just gave up, because you can’t stay there for hours […]” (I-17, F/C3/moderate).
“The treatment that we got was a bit like I [was] back at a five years old school and the fact that by not doing one thing [i.e., independent practice] we were punished without supervised sessions really put me off” (I-9: F/C2/low).
Benefiting from direct supervision
Learners felt that direct supervision in the ICU and in the echo laboratory was crucial to their learning and continuing motivation.
“Without [the supervised] sessions, […] I wouldn't have continued the course. I think the sessions are the core part of the training program” (I-15, F/C2/high).
“The instructors should not be expecting [trainees] to do unsupervised sessions without having about a couple of weeks of echo lab training or supervised training because without that, it’s just a spiral down. It’s a vicious cycle and we won’t learn and we won’t be motivated” (I-4, F/C1/moderate).
Protected time in the echo lab was perceived as invaluable. Yet, learners acknowledged that performing echocardiography in the ICU was more challenging than in the echo lab, and recalled experiencing difficulties in transferring CCE skills acquired in the echo lab to ICU patients:
“The second year was better [and] I have to attribute it a lot to the fact that I did the echo lab training. So, I got my confidence […] and then now the learning is more about how to adjust the views to an ICU patient […]” (I-4, F/C1/moderate).
Rising or not rising to the challenge: sustaining motivation
Learners described two types of response to difficulties encountered in the program. Certain trainees disengaged with the program, felt demoralized about different aspects of the course, and eventually gave up.
“Maybe six months or so [into the training], I just thought, I actually just can’t do this anymore” (I-10, F/C2/moderate).
Learners explained their loss of motivation in three ways: a perceived lack of performance improvement over time, personal circumstances that interfered with their ability to complete the program requirements, and realization of a misalignment between the program and their personal objectives.
“I felt that I wasn’t getting much out of the echoes because I wasn't having supervised sessions” (I-9, F/C2/low).
“Maybe I did not read enough around it afterwards […] because other folks did manage it and did complete it, so obviously, it’s doable. It might have just been my circumstances at the time […]. Some concepts may [have been] too advanced for intensivists, [who] wanted to learn basic or intermediate echo skills” (I-10, F/C2).
Conversely, other learners recalled investing more effort and engaging in additional independent practice when facing training challenges. Realizing their learning progress and seeing the potential impact of CCE on the management of their patients eventually contributed to maintaining high levels of motivation.
“When I was not confident, I just put more effort into training and then I started feeling more confident, which gave me more interest in the course, because it showed me that what I was doing was actually working, that I had actually learned things. […] It was the day I diagnosed an aortic dissection in a patient with an echo […] [that I realized] the many diagnoses I was able to make and the patients that I was able to help by knowing echocardiography” (I-14, F/C3/high).
When reflecting on their experience, highly engaged learners also reported stress when performing CCE initially, but eventually enjoyed it.
Quantitative effect of curricular changes on learners’ engagement
Teaching attendance and echocardiogram submissions are presented in ESM eTable 3. Learners submitted unsupervised echocardiograms with a 1.11-fold higher rate when supervision was conditional than when supervision was unconditional (rate ratio, 1.11; 95% credible interval [CrI], 1.08 to 1.14) (ESM eTable 3 and eTable 4). Rotation in the echo lab was associated with a subsequent decrease in the rate of submitting unsupervised echocardiograms (Fig. 3 and ESM eTable 5). Trainees who went to the echo lab either did not submit any unsupervised echocardiograms after the echo lab rotation (odds ratio of submitting echocardiograms, 0.2; 95 % CrI, 0.1 to 0.33) or submitted at a substantially lower rate (rate ratio of submitting echocardiograms, 0.10; 95% CrI, 0.09 to 0.14).
Critical care echocardiograms submission pre- and post-echo lab rotation. The dotted vertical lines represent the rotation in the echo lab. In blue are the number of echocardiograms submitted monthly before the rotation in the echo lab. The red lines represent the monthly number of echocardiograms submitted after the rotation in the echo lab.
Discussion
We found that learners reported lack of protected time and limited access to supervision as the main barriers to successful program completion. Nevertheless, unconditional access to en-bloc supervision or rotation in the echo lab (sustained supervision by a sonographer) did not increase independent practice. We assumed that offering supervision as a reward for regular independent practice would motivate learners to practice more independently between supervised sessions and would increase program completion rates. Providing shorter (two-hour) but more frequent supervised sessions distributed throughout the year was expected to foster consolidation of newly acquired skills compared with longer (week-long), but infrequent (twice a year) supervised sessions. Our assumption was based on existing evidence showing that distributive practice can lead to superior learning outcomes compared with en-bloc practice.44,45 In implementing these changes, we hoped to motivate learners and to identify trainees who, by showing that they had practiced independently, were more likely to benefit from further supervision.52 We were also cognizant of the potential risk of “too much” supervision, which may limit learners’ ability to learn to perform independently.53 Surprisingly, the implementation of conditional and distributed supervision was perceived negatively by many learners and failed to increase the rate of training completion, despite having a positive impact on independent practice, as measured by the number of unsupervised echocardiograms submitted for review.
Our findings indicated that throughout the three years of the advanced CCE program implementation, many learners lost their motivation early in the academic year. There were different reasons for this: 1) discouragement in response to the skill complexity and lack of perceived progress, 2) negative emotions experienced during independent practice, 3) unintended negative perception of the conditional supervision implemented after year 1 and, 4) learners’ realization of a mismatch between their goals and the course objectives. Our assumption that the promise of supervision would be globally perceived as a reward and increase learners’ motivation to engage in unsupervised practice was incorrect. As described by Deci, contingent rewards may have a negative effect on intrinsic motivation.54,55,56 Applying contingent supervision may have blunted learner’s sense of autonomy and volition, resulting in lower intrinsic motivation. Interestingly, whereas some learners became disengaged, others embraced the challenges encountered by investing more efforts in training. As they started seeing the benefits of their efforts and of their newly acquired skills in clinical practice, they were increasingly motivated to pursue training, which they eventually reportedly enjoyed.
Additionally, we observed that, following the echo lab rotation, trainees submitted even fewer echocardiograms than before. We speculate that as learners gained confidence throughout their echo lab rotation, they may have deemed subsequent independent practice unnecessary.57 Possibly facing a steep de-learning curve without immediate skill consolidation after the echo lab rotation, they may have faced unexpected challenges when resuming independent practice on challenging ICU patients.28,44,58
Our low rate of program completion is similar to those described in previous reports.16,22 Likewise, technical challenges (especially without supervision), clinical duties conflicting with educational activities, variable willingness to persist despite challenges, and personal factors were identified as major barriers.16 Our study also suggests that underlying factors, such as motivation and persistence when facing failure, may be playing a role, which aligns with self-regulated learning theory.59 Indeed, learning advanced echocardiography in the critical care context appears to be more challenging than learning echocardiography on cardiology patients. Moreover, learning advanced CCE differs from echocardiography training for cardiologists, which heavily relies on extended time in the echo lab where supervision (by a cardiologist or sonographer) is not a limitation. Advanced CCE learners may not expect a slow learning curve, a realization that may lead them to abandon training unless they remain intrinsically motivated and have personal goals aligned with curricular objectives.
Our study has several limitations. First, the sample size was small, which is why we used Bayesian instead of frequentist statistics to analyze the data. Second, at the time of program inception, our units did not have the equipment to perform transesophageal echocardiography, so our program was restricted to transthoracic echocardiography. Furthermore, the paucity of highly trained echocardiographers among critical care attendings may have been a limitation. Indeed, learners had limited opportunities to observe the use and benefit of echocardiography, and to obtain real-time feedback from their primary clinical supervisor during their daily clinical activities. Third, relevant residual confounding (explaining low completion) cannot be excluded. Fourth, interviews were analyzed by two investigators, one of whom had an instrumental role in the design and delivery of the program. To mitigate narrow interpretations, we incorporated reflexivity throughout the research process. Fifth, although our study elicited possible explanations for low engagement, further research is needed to clarify differences between learners that maintained motivation throughout training and achieved CCE competence and those that failed to do so.
It may be argued that our program was too ambitious, especially for learners without previous basic CCE experience; however, the requirement of 150 echocardiograms was based on international recommendations and matched the requirements for North American certification.11 Furthermore, learners could complete their portfolio in more than one year and could remotely submit their echocardiograms for review. Lastly, we did not explore if and to what extent supervision impacted trainees’ learning curve. The fact that supervision failed to increase learners’ engagement and program completion does not invalidate its importance. Indeed, given the technical challenges of performing echocardiography on critically ill patients, novices may be unable to discern whether low-quality echocardiographic images relate to patients’ factors or to their inexperience.
In summary, lack of time and limited access to supervised practice were the major barriers reported by learners. Nevertheless, the provision of protected time in the echo lab and direct supervision in a critical care setting did not increase the likelihood of trainees completing their portfolios. Other factors such as sustained motivation and persistence may play significant roles in learners’ engagement and training completion. Further research is needed to better understand potential modifiers of motivation and engagement of learners enrolled in advanced CCE training.
References
Vieillard-Baron A, Slama M, Cholley B, Janvier G, Vignon P. Echocardiography in the intensive care unit: from evolution to revolution? Intensive Care Med 2008; 34: 243–249. https://doi.org/10.1007/s00134-007-0923-5
Royse CF, Canty DJ, Faris J, Haji DL, Veltman M, Royse A. Core review: physician-performed ultrasound: the time has come for routine use in acute care medicine. Anesth Analg 2012; 115: 1007–28. https://doi.org/10.1213/ane.0b013e31826a79c1
Price S, Via G, Sloth E, et al. Echocardiography practice, training and accreditation in the intensive care: document for the World Interactive Network Focused on Critical Ultrasound (WINFOCUS). Cardiovasc Ultrasound 2008; 6: 49. https://doi.org/10.1186/1476-7120-6-49
Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 2014; 27: e1–33. https://doi.org/10.1016/j.echo.2014.05.001
Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 2010; 23: 1225–30. https://doi.org/10.1016/j.echo.2010.10.005
Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 2013; 26: 567–81. https://doi.org/10.1016/j.echo.2013.04.001
Moore CL, Copel JA. Point–of–care ultrasonography. New Engl J Med 2011; 364: 749–57. https://doi.org/10.1056/nejmra0909487
Vignon P, Mücke F, Bellec F, et al. Basic critical care echocardiography: validation of a curriculum dedicated to noncardiologist residents. Crit Care Med 2011; 39: 636–42. https://doi.org/10.1097/ccm.0b013e318206c1e4
Wiegers SE. The point of care. J Am Soc Echocardiogr 2016; 29: A19. https://doi.org/10.1016/j.echo.2016.02.007
European Society of Intensive Care Medicine. European diploma in advanced critical care echocardiography. Available from URL: https://www.esicm.org/education/edec-2/ (accessed May 2022).
National Board of Echocardiography, Inc. Application for Certification in Critical Care Echocardiography (CCEeXAM): certifcation requirements and online certification instructions 2021. Available from URL: https://echoboards.org/docs/CCEeXAM-Cert_App-2021.pdf (accessed April 2022).
Mayo PH, Koenig S. Advanced critical care echocardiography certification: an update. Chest 2020; 158: 48–9. https://doi.org/10.1016/j.chest.2020.02.037
Almaani M, Alabdrab Alnabi M, Bainbridge D, Taneja R. Transthoracic echocardiography performed by intensive care fellows: Is minimal focused training enough? Crit Care 2011; 15: S9. https://doi.org/10.1186/cc9445
Charron C, Templier F, Goddet NS, Baer M, Vieillard-Baron A, Group of Investigators of SAMU 92. Difficulties encountered by physicians in interpreting focused echocardiography using a pocket ultrasound machine in prehospital emergencies. Eur J Emerg Med 2015; 22: 17–22. https://doi.org/10.1097/mej.0000000000000153
Manasia AR, Nagaraj HM, Kodali RB, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth 2005; 19: 155–9. https://doi.org/10.1053/j.jvca.2005.01.023
Gillon S, Walker D, Jones N. Barriers to focused echocardiography education. Eur J Emerg Med 2016; 23: 75–6. https://doi.org/10.1097/mej.0000000000000309
Eisen LA, Leung S, Gallagher AE, Kvetan V. Barriers to ultrasound training in critical care medicine fellowships: a survey of program directors. Crit Care Med 2010; 38: 1978–83. https://doi.org/10.1097/ccm.0b013e3181eeda53
Kirkpatrick JN, Grimm R, Johri AM, et al. Recommendations for Echocardiography Laboratories Participating in Cardiac Point of Care Cardiac Ultrasound (POCUS) and critical care echocardiography training: report from the American Society of Echocardiography. J Am Soc Echocardiogr 2020; 33: 409–22. https://doi.org/10.1016/j.echo.2020.01.008
Noritomi DT, Vieira ML, Pesaro AE, et al. Validation of an echochardiography training program for intensivists. Crit Care 2009; 13: P3. https://doi.org/10.1186/cc7805
Ahern M, Mallin MP, Weitzel S, Madsen T, Hunt P. Variability in ultrasound education among emergency medicine residencies. West J Emerg Med. 2010; 11: 314–8.
Colebourn CL, Jones L. Preventing too little too late: a novel process of continuous curriculum evaluation. JPD 2014; 4: 3–14.
Ali A, Korzick K, Miller A, Urrutia L, Strony R. Toward echocardiography and critical care ultrasound integration into critical care fellowship. Crit Care Med 2014; 42: A1436.
Kanji HD, McCallum JL, Bhagirath KM, Neitzel AS. Curriculum development and evaluation of a hemodynamic critical care ultrasound: a systematic review of the literature. Crit Care Med 2016; 44: e742–50. https://doi.org/10.1097/ccm.0000000000001661
Greenstein YY, Littauer R, Narasimhan M, Mayo PH, Koenig SJ. Effectiveness of a critical care ultrasonography course. Chest 2017; 151: 34–40. https://doi.org/10.1016/j.chest.2016.08.1465
Blackstock A, Morton S, Powell-Tuck J, Aron J. Development of an intensive care advanced echo course. Intensive Care Med Exp 2018; 6: 246.
Beraud AS, Rizk NW, Pearl RG, Liang DH, Patterson AJ. Focused transthoracic echocardiography during critical care medicine training: Curriculum implementation and evaluation of proficiency. Crit Care Med 2013; 41: e179–81. https://doi.org/10.1097/ccm.0b013e31828e9240
Yamamoto R, Clanton D, Willis RE, Jonas RB, Cestero RF. Rapid decay of transthoracic echocardiography skills at 1 month: a prospective observational study. J Surg Educ 2018; 75: 503–9. https://doi.org/10.1016/j.jsurg.2017.07.011
Kimura BJ, Sliman SM, Waalen J, Amundson SA, Shaw DJ. Retention of ultrasound skills and training in "point-of-care" cardiac ultrasound. J Am Soc Echocardiogr 2016; 29: 992–7. https://doi.org/10.1016/j.echo.2016.05.013
Hempel D, Stenger T, Dell' Orto MC, et al. Analysis of trainees' memory after classroom presentations of didactical ultrasound courses. Crit Ultrasound J 2014; 6: 10. https://doi.org/10.1186/2036-7902-6-10
Expert Round Table on Echocardiography in ICU. International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med 2014; 40: 654–666. https://doi.org/10.1007/s00134-014-3228-5
Harden RM. Ten questions to ask when planning a course or curriculum. Med Educ 1986; 20: 356–65. https://doi.org/10.1111/j.1365-2923.1986.tb01379.x
Prideaux D. Curriculum design. BMJ 2003; 326: 268–70. https://doi.org/10.1136/bmj.326.7383.268
Grant J. Principles of curriculum design. In: Swanwick T, Forrest K, O'Brien BC (Eds.). Understanding Medical Education: Evidence, Theory and Practice, 2nd ed. Chichester: Wiley-Blackwell; 2014: 31–46.
Quiñones MA, Douglas PS, Foster E, et al. ACC/AHA clinical competence statement on echocardiography: a report of the American College of Cardiology/American Heart Association/American College of Physicians-American Society of Internal Medicine Task Force on clinical competence. J Am Soc Echocardiogr 2003;16:379-402. https://doi.org/10.1016/s0894-7317(03)00113-5
Millington SJ, Arntfield RT, Hewak M, et al. The rapid assessment of competency in echocardiography scale: validation of a tool for point-of-care ultrasound. J Ultrasound Med 2016; 35: 1457–63. https://doi.org/10.7863/ultra.15.07083
Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev 1993; 100: 363–406.
Artino AR Jr, Brydges R, Gruppen LD. Self-regulated learning in healthcare profession education: theoretical perspectives and research methods. In: Cleland J, Dunning SJ (Eds.). Researching Medical Education. Wiley-Blackwell; 2015: 155–66.
McGaghie WC, Kristopaitis T. Deliberate practice and mastery learning: origins of expert medical performance. In: Cleland J, Dunning SJ (Eds.). Researching Medical Education. Wiley-Blackwell; 2015: 219–30.
Pusic MV, Pecaric M, Boutis K. How much practice is enough? Using learning curves to assess the deliberate practice of radiograph interpretation. Acad Med 2011; 86: 731–6. https://doi.org/10.1097/acm.0b013e3182178c3c
Pusic MV, Boutis K, Hatala R, Cook DA. Learning curves in health professions education. Acad Med 2015; 90: 1034–42. https://doi.org/10.1097/acm.0000000000000681
Ericsson KA. Acquisition and maintenance of medical expertise: a perspective from the expert-performance approach with deliberate practice. Acad Med 2015; 90: 1471–86. https://doi.org/10.1097/acm.0000000000000939
Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med 2008; 15: 988–94. https://doi.org/10.1111/j.1553-2712.2008.00227.x
Brydges R, Dubrowski A, Regehr G. A new concept of unsupervised learning: directed self-guided learning in the health professions. Acad Med 2010; 85: S49–55. https://doi.org/10.1097/acm.0b013e3181ed4c96
Savion-Lemieux T, Penhune VB. The effects of practice and delay on motor skill learning and retention. Exp Brain Res 2005; 161: 423–31. https://doi.org/10.1007/s00221-004-2085-9
Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R. Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg 2006; 244: 400–9. https://doi.org/10.1097/01.sla.0000234808.85789.6a
Bowling A. Research Methods in Health: Investigating Health and Health Services. McGraw-Hill Education; 2009.
Teddlie C, Yu F. Mixed methods sampling: a typology with examples. J Mix Methods Res 2007; 1: 77–100. https://doi.org/10.1177/1558689806292430
Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ 2000; 320: 114–6. https://doi.org/10.1136/bmj.320.7227.114
Baker SE, Edwards R. How many qualitative interviews is enough? Expert voices and early career reflections on sampling and cases in qualitative research. Availabe from URL: https://eprints.ncrm.ac.uk/id/eprint/2273/4/how_many_interviews.pdf (access April 2022).
Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th ed. Los Angeles: Sage; 2018.
Depaoli S, Rus HM, Clifton JP, van de Schoot R, Tiemensma J. An introduction to Bayesian statistics in health psychology. Health Psychol Rev 2017; 11: 248–64.
Dunlosky J, Ariel R. Self-regulated learning and the allocation of study time. Psychol Learn Motiv - Adv Res Theory 2011; 54: 103–40. https://doi.org/10.1016/B978-0-12-385527-5.00004-8
Salmoni AW, Schmdt RA, Walter CB. Knowledge of results and motor learning- a review and critical reappraisal. Psychol Bull 1984; 95: 355–86. https://doi.org/10.1037/0033-2909.95.3.355
Deci EL. Intrinsic motivation, extrinsic reinforcement, and inequity. J Pers Soc Psychol 1972; 22: 113–20. https://doi.org/10.1037/h0032355
Deci EL, Ryan RM, Williams GC. Need satisfaction and the self-regulation of learning. Learn Individ Diff 1996; 8: 165–83. https://doi.org/10.1016/S1041-6080(96)90013-8
Pink DH. Drive: The Surprising Truth About What Motivates Us. Riverhead Books; 2009.
Koriat A, Bjork RA. Illusions of competence in monitoring one's knowledge during study. J Exp Psychol Learn Mem Cogn 2005; 31: 187–94. https://doi.org/10.1037/0278-7393.31.2.187
Dayan E, Cohen LG. Neuroplasticity subserving motor skill learning. Neuron 2011; 72: 443–54. https://doi.org/10.1016/j.neuron.2011.10.008
Sitzmann T, Ely K. A meta-analysis of self-regulated learning in work-related training and educational attainment: what we know and where we need to go. Psychol Bull 2011; 137: 421–42. https://doi.org/10.1037/a0022777
Author contributions
Dominique Piquette, Ryan Brydges, and Ghislaine Douflé designed and planned the study. Ghislaine Douflé, Laura Dragoi, and Aditi Jain collected the data. Ghislaine Douflé, Dominique Piquette, and Martin Urner analyzed and interpreted the data. Ghislaine Douflé wrote the first draft. All authors were involved in critical revision of the final manuscript.
Acknowledgements
The authors would like to acknowledge Dr. Goffi for his instrumental role in the design of the program and Dr. Mema for her feedback and advice.
Disclosures
The authors have no conflict of interest to disclose.
Funding statement
None.
Data availability statement
The source code is included in the Electronic Supplementary Material, eAppendix 3. Data are available upon request from the authors.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Douflé, G., Urner, M., Dragoi, L. et al. Evaluation of an advanced critical care echocardiography program: a mixed methods study. Can J Anesth/J Can Anesth 69, 1260–1271 (2022). https://doi.org/10.1007/s12630-022-02281-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02281-6