Abstract
Purpose
Studies comparing the recently introduced Ambu® AuraGain™ (Auragain) with the LMA® Supreme™ (Supreme) supraglottic airway (SGA) have reported conflicting results regarding differences in oropharyngeal leak pressure (OLP). This randomized-controlled trial investigated the OLP of the Auragain compared with the Supreme in patients undergoing ambulatory surgery.
Methods
Adult patients with a body mass index ≤ 40 kg·m−2 presenting for ambulatory surgery and requiring an SGA were randomized to receive either the Auragain or the Supreme. Anesthesia was induced with lidocaine (1 mg·kg−1), fentanyl (1-2 μg·kg−1), and propofol (2-3 mg·kg−1). The SGA was inserted using a standard technique with the cuff inflated to 60 cmH2O. The groups were compared for the primary outcome of OLP.
Results
One hundred sixty-five patients (n = 81, Auragain; n = 84, Supreme) completed the study. Demographics were similar between the groups. The mean (standard deviation [SD]) OLP was significantly higher in the Auragain than in the Supreme group [26.4 (2.8) cmH2O vs 21.6 (3.4) cmH2O, respectively; difference in means (MD), 4.8 cmH2O; 95% confidence interval (CI), 3.9 to 5.8; P < 0.001]. The mean (SD) insertion time was longer in the Auragain than in the Supreme group [13 (4) sec vs 11 (3) sec, respectively; MD, 2 sec; 95% CI, 1 to 3 sec; P < 0.001].
Conclusion
In patients undergoing ambulatory anesthesia, the OLP was higher but took longer to insert with the Auragain than with the Supreme. A higher OLP may allow for SGAs to be utilized in a wider range of patients and procedures.
Trial registration
www.clinicaltrials.gov (NCT02816463). Registered 28 June 2016.
Résumé
Objectif
Des études comparant les voies respiratoires supraglottiques (SGA) Ambu® AuraGain™ (Auragain) nouvellement commercialisé et LMA® Supreme™ (Supreme) ont fourni des résultats contradictoires concernant les différences de pressions de fuite oropharyngée (OLP). Cet essai randomisé contrôlé a étudié l’OLP de l’Auragain comparativement à celle du Supreme chez des patients subissant une chirurgie ambulatoire.
Méthodes
Des patients adultes ayant un indice de masse corporelle ≤ 40 kg· m−2 venant pour chirurgie ambulatoire et nécessitant une SGA ont été randomisés pour bénéficier de l’Auragain ou du Supreme. L’anesthésie a été induite avec de la lidocaïne (1 mg· kg−1), du fentanyl (1-2 μg·kg−1) et du propofol (2-3 mg· kg−1). La SGA a été insérée selon une technique standard et le ballonnet a été gonflé à 60 cmH2O. Le principal critère d’évaluation comparé entre les deux groupes était l’OLP.
Résultats
Cent soixante-cinq patients (n = 81, Auragain; n = 84, Supreme) ont terminé l’étude. Les données démographiques étaient similaires entre les groupes. L’OLP moyenne (écart-type [ÉT]) était significativement plus élevée dans le groupe Auragain que dans le groupe Supreme (respectivement, 26,4 [2,8] cmH2O contre 21,6 [3,4] cmH2O; différence des moyennes, 4,8 cmH2O; intervalle de confiance [IC] à 95 % : 3,9 à 5,8; P < 0,001). Le temps moyen (ÉT) d’insertion a été plus long dans le groupe Auragain que dans le groupe Supreme (respectivement, 13 [4] s contre 11 [3] s; différence des moyennes, 2 s; IC à 95 %, 1 à 3 s; P < 0,001).
Conclusion
Chez les patients subissant une anesthésie ambulatoire, l’OLP a été plus élevée avec l’Auragain qu’avec le Supreme, mais son insertion a pris plus de temps. Une OLP plus élevée pourrait permettre d’utiliser les SGA dans un plus vaste éventail de procédures et de patients.
Enregistrement de l’essai clinique
www.ClinicalTrials.gov (NCT02816463). Enregistré le 28 juin 2016.
Similar content being viewed by others
Since their introduction, supraglottic airways (SGAs) have been widely used for airway management during general anesthesia. These devices are designed to provide a seal around the laryngeal inlet and have been utilized as ventilation devices as well as conduits for tracheal intubation.1,2,3,4,5
Oropharyngeal leak pressure (OLP)—i.e., the airway pressure at which gas leaks back around the SGA cuff—is a key marker of the efficacy and safety of SGAs. A higher OLP suggests a better seal between the SGA and the supraglottic mucosa and is thought to allow for greater levels of positive pressure ventilation and improved gastric aspiration protection.2 Improvements in newer SGAs have aimed to achieve higher OLPs, enhance gastric venting, and facilitate SGA-guided intubation.2 Certain clinical situations require SGA devices to maintain high OLP such as patients with obesity, increased intra-abdominal pressure in laparoscopic surgery, and patients with restrictive lung disease.6
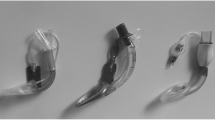
The LMA® Supreme™ (Supreme) (Teleflex, Morrisville, NC, USA) is a single-use, anatomically curved SGA with a gastric access conduit.7 The Supreme features a preformed curved shaft with a double lumen, a built-in bite block, and moulded fins at the laryngeal outlet (Fig. 1).7,8,9 It is the one of the most commonly used SGAs with a well-established safety and efficacy profile.6
The Ambu® AuraGain™ (Auragain) (Ambu Inc., Columbia, MD, USA) is a newer SGA released in 2014. The Auragain similarly has a preformed curved shaft with a double lumen, but it also features a comparatively wider airway tube to facilitate the passage of a larger endotracheal tube and does not have fins at the laryngeal outlet (Fig. 1).9,10,11
Previous studies have reported conflicting results regarding differences in OLP between the Auragain and the Supreme. Lopez et al.10 compared the Auragain with the Supreme and showed a higher mean OLP of 34 cmH2O for the Auragain (vs 29 cmH2O in the Supreme). Nevertheless, other studies comparing the Auragain with the Supreme have reported no significant differences in OLP between the two devices.9,12 To date, limited data are available regarding the OLP of the Auragain vs the Supreme in patients undergoing ambulatory surgery.
The purpose of this study was to compare the OLP (primary endpoint) of the Auragain with that of the Supreme in patients undergoing ambulatory surgery with general anesthesia. We hypothesized that the Auragain would provide a higher OLP than the Supreme.
Methods
The study was approved (11 August 2015) by the institutional research ethics board (University Health Network, Toronto, ON, Canada) and registered with ClinicalTrials.gov (NCT02816463). It was conducted at Toronto Western Hospital, a tertiary hospital located in Toronto, ON. Written informed consent was obtained from all patients. Inclusion criteria were American Society of Anesthesiologists physical status I-III, > 18 yr of age, elective ambulatory surgery under general anesthesia with an anticipated duration < two hours, and suitability for SGA use. Exclusion criteria included reduced mouth opening (< 2.5 cm), recent history of upper respiratory tract infection, sore throat < two weeks, and contraindication to SGA use including morbid obesity (body mass index > 40 kg·m−2) or severe symptomatic esophageal reflux disease.
Patients were randomized to either the Auragain or the Supreme group. Randomization was done by the institutional biostatistician using a computer-generated block randomization procedure. Sealed randomization envelopes were kept by the research coordinator and opened by a single investigator 30 min before the scheduled case, after which the patients were assigned to their study groups.
Patients were positioned supine on the operating table and routine intraoperative monitors13 were applied. General anesthesia was initiated with lidocaine 1-1.5 mg·kg−1, fentanyl 1-2 μg·kg−1, and propofol 2-3 mg·kg−1. The assigned SGA was inserted when the depth of anesthesia was deemed appropriate by the anesthesiologist. Anesthesiologists (fellow trainees or consultant-level attendings) who had a minimum of one-year experience with SGAs having inserted more than 100 of them were involved in the study.
In both groups, the SGA was sized according to manufacturer recommendations. In patients weighing < 50 kg, a size 3 SGA was used; 50-70 kg, size 4 SGA; and > 70 kg, size 5 SGA. Minor variations of the sizing of the SGA were permitted at the discretion of the anesthesiologist. The SGA was lubricated on its dorsal surface with a water-soluble, non-conductive lubricant (MUKO lubricating jelly, Cardinal Health Canada Inc. Mississauga, ON, Canada) and was inserted as per the manufacturer’s instructions. The SGA was inflated to an intracuff pressure of 60 cmH2O, as measured by a Portex cuff manometer (Smiths Medical, Dublin, OH, USA). Initial assessment of ventilation was achieved by observation of capnography and thoraco-abdominal movement. The SGA was repositioned, if necessary, to optimize ventilation or capnography. A maximum of three attempts at SGA insertion were permitted, after which patients were excluded from the study.
The OLP was measured using the technique described by Zhang et al.2 with the patient’s head in a neutral position and the adjustable pressure limiting (APL) valve of the circle system set at 70 cmH2O with a fresh gas flow of 3 L·min−1. The anesthesia circuit airway pressure was measured with a T-piece interposed between the SGA and the breathing circuit, using a pressure manometer Portex cuff manometer (Smiths Medical, Dublin, OH, USA). The OLP was defined as the measured circuit airway pressure when an audible leak was first detected using a stethoscope placed over the neck. Once the OLP had been measured, the APL valve was opened and either spontaneous or controlled ventilation was resumed.
Patients were maintained on desflurane in air/oxygen with a F i O2 of 0.3-0.5. No nitrous oxide was used. After insertion, all patients were ventilated manually for the first few breaths. Later they were ventilated spontaneously or controlled as clinically indicated. Muscle relaxation was not used. Fentanyl was used for intraoperative analgesia, titrated according to patient requirements. The anesthesiologist removed the SGA at the end of the procedure once patients were awake and obeyed commands. Patients were moved to the postanesthesia care unit (PACU) for routine PACU care and discharged home according to standardized discharge criteria.14 A single investigator (K.S.) who was blinded to the patient group allocation interviewed the patients, collected perioperative data, and contacted patients after discharge home via a telephone interview to collect data at 24 hr.
The primary outcome of the study was the OLP.2 Secondary outcomes included pharyngolaryngeal complications, anesthesiologist’s satisfaction with the SGA, and patient satisfaction with the anesthesia. Additional variables assessed included: SGA insertion time, number of insertion attempts, ease of SGA insertion, laryngospasm and blood staining on the SGA after removal, and length of PACU stay.
Assessment for pharyngolaryngeal complications was done at one and two hours in the postoperative recovery period and at 24 hr postoperatively during a phone call to the patient. Sore throat was defined as “constant pain or discomfort in the throat independent of swallowing”; dysphonia was defined as “difficulty speaking or pain on speaking” and dysphagia as “difficulty or pain provoked by swallowing”.15 The composite pharyngolaryngeal complication was rated as present if sore throat, dysphagia, or dysphonia was present at one, two, or 24 hr postoperatively. Anesthesiologist satisfaction with use of the SGA was subjectively assessed as high, moderate, or low.16 Patient satisfaction in relation to experience with the airway was measured at two hours after the surgery in the postoperative period. It was graded using a five-point Likert scale (0 = very dissatisfied to 5 = extremely satisfied). Insertion time was measured from the removal of the face mask until ventilation was confirmed by a satisfactory end-tidal capnography tracing. Ease of insertion with the SGA was assessed by the anesthesiologist as easy, fair, or difficult.
Statistical analysis
Based on a literature review,2,7,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32 the mean (SD) OLP of the Supreme was determined to be 25 (10) cmH2O. We aimed to show that the difference in mean OLP of the Auragain would be greater than 5 cmH2O, which would be considered clinically significant. With a power of 80% and an alpha of 0.05, and accounting for a dropout rate of 10%, a sample size of 85 patients in each group was required.
Continuous variables were presented as mean (SD) and categoric variables as number (%). The primary outcome of OLP was compared between the two groups using an independent samples t test. Continuous and categorical variables were analyzed using the t test and Chi square test, respectively. Bonferroni adjustments for multiplicity were done for the secondary endpoints. P < 0.05 after correction for multiplicity was considered significant. The data were analyzed according to per-protocol analysis. Statistical analyses were performed using IBM SPSS Statistics 20 (IBM Corporation, Armonk, NY, USA).
Results
Between 28 June 2016 and 9 May 2017, 344 patients scheduled for ambulatory surgery were assessed for eligibility and 170 patients were enrolled in the study (Fig. 2). Four patients in the Auragain group were subsequently excluded; two exceeded the maximum of three insertion attempts, and ventilation was deemed inadequate in another two patients after SGA insertion. One patient in the Supreme group was excluded because of excess leak and poor ventilation with the largest available size 5 device. Seven anesthesiologists were involved in the study: five fellows and two attendings. After the exclusions, 165 patients (81 in the Auragain and 84 in the Supreme group) were analyzed.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram (www.consort-statement.org) for patient participation
Patient demographic data and baseline characteristics, including age and body mass index, were similar between the two groups (Table 1). Surgeries included ambulatory orthopedic, ophthalmologic, and urologic procedures.
The mean (SD) OLP was significantly higher in the Auragain than in the Supreme group [26.4 (2.8) cmH2O vs 21.6 (3.4) cmH2O, respectively; difference in means (MD), 4.8 cmH2O; 95% CI, 3.9 to 5.8 cmH2O; P < 0.001] (Table 2). The mean (SD) insertion time was also significantly longer in the Auragain than in the Supreme group [13 (4) sec vs 11 (3) sec, respectively; MD, 2 sec; 95% CI, 1 to 3 sec; P < 0.001], and the first pass success was also significantly lower (77% vs 94%, respectively; P = 0.003). Anesthesiologist satisfaction was significantly lower with the Auragain, with only 53% rating it with high satisfaction compared with 72% with the Supreme (P < 0.001). The Auragain was also subjectively rated as more difficult to insert than the Supreme, with 48% of insertions of the Auragain scored as easy compared with 92% for the Supreme (P < 0.001).
Postoperative symptoms were analyzed in 160 patients (n = 78 Auragain; n = 82 Supreme) as five patients could not be contacted by telephone at 24 hr postoperatively. There were no significant differences in the composite pharyngolaryngeal complications, laryngospasm, blood stains, PACU stay, and patient satisfaction regarding SGA use between the two groups (Table 2).
Discussion
In this study, we found that the OLP of the Auragain was 4.8 cmH2O higher than that of the Supreme. Additionally, the Auragain was associated with increased insertion time, decreased first pass success, decreased ease of insertion, and decreased anesthesiologist satisfaction compared with the Supreme in patients undergoing ambulatory surgery.
The OLP is used to quantify the efficacy of the seal between the supraglottic airway and the supraglottic mucosa2,20 and is associated with the feasibility of positive pressure ventilation, degree of protection from aspiration, and suitability of a supraglottic airway for laparoscopic surgery.3,33 A higher OLP for the Auragain suggests that the Auragain can achieve a better glottic seal (and thus higher ventilatory pressures) for ambulatory surgical patients.
Previously, three studies compared the OLP of the Auragain vs the Supreme and reported conflicting results.9,10,12 In a randomized-controlled trial by Lopez et al.,10 60 adult patients undergoing gynecologic laparoscopic surgery were studied. The OLP was higher in the Auragain vs the Supreme [34 (5) cmH2O vs 29 (5) cmH2O, P < 0.001]. Conversely, in an Asian population characterized by smaller build and smaller mouth opening, no significant difference in OLP was found between the Auragain and the Supreme12 (24.1 cmH2O vs 23.6 cmH2O; P = 0.72).
Jagannathan et al.9 studied 100 children and found no significant difference in OLP between the Auragain and the Supreme. Whereas Jagannathan et al.9 studied pediatric patients, the current study focused on adults using larger supraglottic airways. Singh et al.34 studied 60 patients undergoing laparoscopic cholecystectomy and reported no significant difference in OLP between the Auragain and the LMA ProSeal (28.8 cmH2O vs 27.2 cmH2O; P = 0.30) but obese patients (defined as body mass index ≥ 30 kg·m−2) were not included in the study. In our study, the OLP of 21.5 cmH–2O for the Supreme was lower than expected, but it was comparable to the OLPs provided by previous meta-analyses ranging from 21 to 32 cmH2O.35,36
Anesthesiologist satisfaction was significantly lower for the Auragain than for the Supreme. Previous studies have not examined anesthesiologist satisfaction with the Auragain, although one study found no significant difference in anesthesiologist satisfaction or insertion time between the Supreme and LMA® ProSeal (Teleflex Medical, Morrisville, NC, USA).16 Anesthesiologist satisfaction may have been related to first pass success or ease of insertion, both of which were lower with the Auragain in this study.
There was no significant difference in the incidence of composite pharyngolaryngeal complications between the Auragain and the Supreme (32% vs 38%; P = 0.51). The potential of the Auragain to provide an improved supraglottic seal without increasing adverse postoperative outcomes is reassuring. Shariffuddin et al.12 reported a lower sore throat incidence for the Auragain compared with the Supreme. Other studies reported no significant differences in the incidence of pharyngolaryngeal complications between the Auragain and the Supreme.9,10 Comparisons of the Auragain vs the Supreme found that the incidence of postoperative sore throat varied from 3.2-10% for the Auragain to 0-38% for the Supreme.10,12 Two meta-analyses comparing the Supreme with other supraglottic airways found that the incidence of postoperative sore throat for the Supreme varied from 2-56.7% to 6.7-11.7%.35,36
Similar to a previous study,12 the insertion time was longer for the Auragain than for the Supreme (12.6 sec vs 10.5 sec; P < 0.001). Although there is a statistically significant difference in insertion time between the devices, it is unclear whether a difference of two seconds is considered clinically significant. To accommodate for the bulky curvature of the Auragain, the device generally has to be inserted laterally via a paramedian or side-sweeping technique, potentially contributing to an increased insertion time.11 On the contrary, other studies found no significant difference in insertion time when the Auragain was compared with the Supreme or the air-Q.9,10,37 Nevertheless, Singh et al.34 observed that the Auragain took longer to insert than the LMA ProSeal (13.57 sec vs 11.60 sec; P = 0.001).
With respect to the first pass success, it was significantly lower for the Auragain than for the Supreme (77% vs 94%; P = 0.01). This could be due to the comparatively bulky shaft and the width of the bowl of the Auragain compared with the Supreme. Our findings were different from previous studies that found no significant difference in first pass success between the Auragain and the Supreme.9,10,12 Compared with the Supreme, the Auragain was found to require more maneuvers to secure device placement, but fewer adjustments were required to optimize ventilation.9,10 No significant difference in first pass success was found when the Auragain was compared with the air-Q® intubating laryngeal airway (Cookgas LLC, Mercury Medical, Clearwater, FL, USA) and/or the LMA ProSeal.34,37
As in a previous study,12 we found that the Auragain was rated as more difficult to insert than the Supreme (48% vs 92% of insertions scored as easy; P < 0.001). Previously, it was suggested that the prominent size of the Auragain cuff can impact the insertion time as well as the ease of insertion.10,12 A recent cadaveric study indicated that the firm tip of the Auragain conferred less pliability and did not bend easily towards the hypopharynx after contacting the posterior hypopharyngeal wall.11 In children, no significant difference in ease of device placement was found between the Auragain and the Supreme.9 In addition, no significant difference in ease of device placement was observed when the Auragain was compared with the air-Q or the LMA ProSeal.34,37
There were several limitations of this study. First, the anesthesiologists were not blinded to the SGA used, leading to potential personal bias. Second, most anesthesiologists generally had more experience with the Supreme than with the Auragain, which could have influenced insertion time and ease of insertion. Third, this study examined the clinical use of the Auragain in adult patients with normal airways. These results may not apply to children or patients with more difficult airways. Fourth, the use of this device in larger sample sizes would be needed to assess its safety in patients undergoing positive pressure ventilation and laparoscopic surgery. Finally, the OLP and the intracuff pressure were not measured at the end of the procedure, so it was not possible to comment on how long the difference in OLP between the Auragain and the Supreme persists.
Conclusions
The OLP was higher for the Auragain than for the Supreme in patients undergoing ambulatory surgery with general anesthesia. The insertion time was longer with the Auragain, while first pass success, ease of insertion, and anesthesiologist satisfaction were lower. The difference in insertion time between the devices is small and may not have any clinical significance. The higher OLP attained with the Auragain may make it more suitable for use with positive pressure ventilation potentially increasing the margin of safety in aspiration risk.
References
Campo SL, Denman WT. The laryngeal mask airway: its role in the difficult airway. Int Anesthesiol Clin 2000; 38: 29-45.
Zhang L, Seet E, Mehta V, et al. Oropharyngeal leak pressure with the laryngeal mask airway Supreme™ at different intracuff pressures: a randomized controlled trial. Can J Anesth 2011; 58: 624-9.
Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 1999; 82: 286-7.
Moser B, Audigé L, Keller C, Brimacombe J, Gasteiger L, Bruppacher HR. Flexible bronchoscopic intubation through the AuraGain™ laryngeal mask versus a slit Guedel tube: a non-inferiority randomized-controlled trial. Can J Anesth 2017; 64: 1119-28.
Kleine-Brueggeney M, Kotarlic M, Theiler L, Greif R. Limitations of pediatric supraglottic airway devices as conduits for intubation - an in vitro study. Can J Anesth 2018; 65: 14-22.
Shin HW, Yoo HN, Bae GE, et al. Comparison of oropharyngeal leak pressure and clinical performance of LMA ProSeal™ and i-gel® in adults: meta-analysis and systematic review. J Int Med Res 2016; 44: 405-18.
Eschertzhuber S, Brimacombe J, Hohlrieder M, Keller C. The laryngeal mask airway Supreme™ – a single use laryngeal mask airway with an oesophageal vent. A randomised, cross-over study with the laryngeal mask airway ProSeal™ in paralysed, anaesthetised patients. Anaesthesia 2009; 64: 79-83.
Wong DT, Yang JJ, Jagannathan N. Brief review: The LMA Supreme™ supraglottic airway. Can J Anesth 2012; 59: 483-93.
Jagannathan N, Hajduk J, Sohn L, et al. A randomised comparison of the Ambu® AuraGain™ and the LMA® supreme in infants and children. Anaesthesia 2016; 71: 205-12.
Lopez AM, Agusti M, Gambus P, Pons M, Anglada T, Valero R. A randomized comparison of the Ambu AuraGain versus the LMA supreme in patients undergoing gynaecologic laparoscopic surgery. J Clin Monit Comput 2017; 31: 1255-62.
Lopez AM, Sala-Blanch X, Valero R, Prats A. Cross-over assessment of the AmbuAuraGain, LMA Supreme New Cuff and Intersurgical I-Gel in fresh cadavers. Open J Anesthesiol 2014; 4: 332-9.
Shariffuddin II, Teoh WH, Tang EB, Hashim NH, Loh PS. Ambu® AuraGain™ versus LMA Supreme™ Second Seal™: a randomised controlled trial comparing oropharyngeal leak pressures and gastric drain functionality in spontaneously breathing patients. Anaesth Intensive Care 2017; 45: 244-50.
Dobson G, Chong M, Chow L, et al. Guidelines to the practice of anesthesia - revised edition 2017. Can J Anesth 2017; 64: 65-91.
Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg 1999; 88: 508-17.
Brimacombe J, Holyoake L, Keller C, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology 2000; 93: 26-31.
Seet E, Rajeev S, Firoz T, et al. Safety and efficacy of laryngeal mask airway Supreme versus laryngeal mask airway ProSeal: a randomized controlled trial. Eur J Anaesthesiol 2010; 27: 602-7.
Kang F, Li J, Chai X, Yu J, Zhang H. Tang Cl. Comparison of the I-gel laryngeal mask airway with the LMA-Supreme for airway management in patients undergoing elective lumbar vertebral surgery. J Neurosurg Anesthesiol 2014; 27: 37-41.
Joly N, Poulin LP, Tanoubi I, Drolet P, Donati F, St-Pierre P. Randomized prospective trial comparing two supraglottic airway devices: i-gel™ and LMA-Supreme™ in paralyzed patients. Can J Anesth 2014; 61: 794-800.
Tiefenthaler W, Eschertzhuber S, Brimacombe J, Fricke E, Keller C, Kaufmann M. A randomised, non-crossover study of the GuardianCPV™ Laryngeal Mask versus the LMA Supreme™ in paralysed, anaesthetised female patients. Anaesthesia 2013; 68: 600-4.
Beleña JM, Núñez M, Anta D, et al. Comparison of Laryngeal Mask Airway Supreme and Laryngeal Mask Airway Proseal with respect to oropharyngeal leak pressure during laparoscopic cholecystectomy: a randomised controlled trial. Eur J Anaesthesiol 2013; 30: 119-23.
Russo SG, Cremer S, Galli T, et al. Randomized comparison of the i-gel™, the LMA Supreme™, and the Laryngeal Tube Suction-D using clinical and fibreoptic assessments in elective patients. BMC Anesthesiol 2012; 12: 18.
Van Zundert TC, Brimacombe JR. Similar oropharyngeal leak pressures during anaesthesia with i-gel™, LMA-ProSeal™ and LMA-Supreme™ laryngeal masks. Acta Anaesthesiol Belg 2012; 63: 35-41.
Ragazzi R, Finessi L, Farinelli I, Alvisi R, Volta CA. LMA Supreme™ vs i-gel™–a comparison of insertion success in novices. Anaesthesia 2012; 67: 384-8.
López AM, Valero R, Hurtado P, Gambus P, Pons M, Anglada T. Comparison of the LMA Supreme™ with the LMA Proseal™ for airway management in patients anaesthetized in prone position. Br J Anaesth 2011; 107: 265-71.
Ali MZ, Ebied RS, El-Tawdy AF, Refaat AI, Kamal NM. Controlled mechanical ventilation with LMA Sureme™ versus i-gel™ in anesthetized adult patients. J Egypt Soc Parasitol 2011; 41: 365-78.
Beleña JM, Gracia JL, Ayala JL, et al. The Laryngeal Mask Airway Supreme for positive pressure ventilation during laparoscopic cholecystectomy. J Clin Anesth 2011; 23: 456-60.
Teoh WH, Lee KM, Suhitharan T, Yahaza Z, Teo MM, Sia AT. Comparison of the LMA Supreme vs the i-gel™ in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia 2010; 65: 1173-9.
Tham HM, Tan SM, Woon KL, Zhao YD. A comparison of the Supreme™ laryngeal mask airway with the Proseal™ laryngeal mask airway in anesthetized paralyzed adult patients: a randomized crossover study. Can J Anesth 2010; 57: 672-8.
Chew EE, Hashim NH, Wang CY. Randomised comparison of the LMA Supreme™ with the I-Gel™ in spontaneously breathing anaesthetised adult patients. Anaesth Intensive Care 2010; 38: 1018-22.
Lee AK, Tey JB, Lim Y, Sia AT. Comparison of the single-use LMA Supreme with the reusable ProSeal LMA for anaesthesia in gynaecological laparoscopic surgery. Anaesth Intensive Care 2009; 37: 815-9.
Hosten T, Gurkan Y, Ozdamar D, Tekin M, Toker K, Solak M. A new supraglottic airway device: LMA-Supreme™, comparison with LMA-Proseal™. Acta Anaesthesiol Scand 2009; 53: 852-7.
Timmermann A, Cremer S, Eich C, et al. Prospective clinical and fiberoptic evaluation of the Supreme laryngeal mask airway™. Anesthesiology 2009; 110: 262-5.
Natalini G, Lanza G, Rosano A, Dell’Agnolo P, Bernardini A. Standard Laryngeal Mask Airway™ and LMA-ProSeal™ during laparoscopic surgery. J Clin Anesth 2003; 15: 428-32.
Singh K, Gurha P. Comparative evaluation of Ambu AuraGain™ with ProSeal™ laryngeal mask airway in patients undergoing laparoscopic cholecystectomy. Indian J Anaesth 2017; 61: 469-74.
Maitra S, Khanna P, Baidya DK. Comparison of laryngeal mask airway Supreme and laryngeal mask airway Pro-Seal for controlled ventilation during general anaesthesia in adult patients: systematic review with meta-analysis. Eur J Anaesthesiol 2014; 31: 266-73.
Chen X, Jiao J, Cong X, Liu L, Wu X. A comparison of the performance of the I-gel™ vs. the LMA-S™ during anesthesia: a meta-analysis of randomized controlled trials. PLoS One 2013; 8: e71910.
Sethi S, Maitra S, Saini V, Samara T. Comparison of Ambu® AuraGain™ laryngeal mask and air-Q™ intubating laryngeal airway for blind tracheal intubation in adults: a randomized controlled trial. Egypt J Anaesth 2017; 33: 137-40.
Acknowledgements
The authors thank the anesthesiologists who participated in this study. The authors also thank Ambu Inc. (Ambu AuraGain™) and Teleflex Medical Canada Inc. (LMA Supreme™) for providing the SGAs free of charge for this study.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
David T. Wong and Kawal P. Singh contributed substantially to all aspects of this manuscript, including conception and design, acquisition, analysis, interpretation of data, and drafting the article. Alister Ooi and Frances Chung contributed substantially to the conception, design, and drafting of the manuscript. Jason Lau, Mandeep Singh, and Jean Wong contributed to analyses of data and drafting of the article. Amelie Dallaire and Vina Meliana contributed to the acquisition and analysis of data and drafting of the article.
Funding
This study was supported in part by the Department of Anesthesia, Toronto Western Hospital, University Health Network, University of Toronto, and by the Toronto General & Western Hospital Foundation.
Ambu Inc. (Ambu AuraGain™) and Teleflex Medical Canada Inc. (LMA Supreme™) provided the supraglottic airways free of charge for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, D.T., Ooi, A., Singh, K.P. et al. Comparison of oropharyngeal leak pressure between the Ambu® AuraGain™ and the LMA® Supreme™ supraglottic airways: a randomized-controlled trial. Can J Anesth/J Can Anesth 65, 797–805 (2018). https://doi.org/10.1007/s12630-018-1120-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-018-1120-4