Abstract
Purpose
During the process of tracheal intubation, patients are apneic or hypoventilating and are at risk of becoming hypoxemic. This risk is especially high in patients with acute or chronic respiratory failure and accompanying compromised respiratory reserve. To address this concern, apneic oxygenation can be administered during tracheal intubation to aid in maintaining arterial oxygen saturation. The objective of this narrative review is to examine the utilization of apneic oxygenation within the operating room, intensive care unit (ICU), emergency department, and pre-hospital settings and to determine its efficacy compared with controls.
Source
For this narrative review, we obtained pertinent articles using MEDLINE® (1946 to April 2016), EMBASE™ (1974 to April 2016), Google Scholar, and manual searches. Apneic oxygenation was administered using various techniques, including the use of nasal prongs, nasopharyngeal or endotracheal catheters, or laryngoscopes.
Principal findings
First, all 12 operating room studies showed that apneic oxygenation significantly prolonged the duration to, and incidence of, desaturation. Second, two of the five ICU studies showed a significantly smaller decline in oxygen saturation with apneic oxygenation, with three studies showing no statistically significant difference vs controls. Lastly, two emergency department or pre-hospital studies showed that the use of apneic oxygenation resulted in a significantly lower incidence of desaturation and smaller declines in oxygen saturation.
Conclusion
Sixteen of the 19 studies showed that apneic oxygenation prolongs safe apneic time and reduces the incidence of arterial oxygen desaturation. Overall, studies in this review show that apneic oxygenation prolongs the time to oxygen desaturation during tracheal intubation. Nevertheless, the majority of the studies were small in size, and they neither measured nor were adequately powered to detect adverse respiratory events or other serious rare complications. Prolonged apneic oxygenation (with its consequent hypercarbia) can have risks and should be avoided in patients with conditions such as increased intracranial pressure, metabolic acidosis, hyperkalemia, and pulmonary hypertension.
Résumé
Objectif
Pendant le processus d’intubation trachéale, les patients sont en état d’apnée ou d’hypoventilation et courent le risque de devenir hypoxémiques. Ce risque est particulièrement élevé chez les patients atteints d’insuffisance respiratoire aiguë ou chronique souvent accompagnée d’une réserve respiratoire compromise. Afin de traiter ce problème, une oxygénation apnéique peut être mise en œuvre pendant l’intubation trachéale afin d’aider à maintenir la saturation artérielle en oxygène. L’objectif de ce compte rendu narratif était d’examiner l’utilisation de l’oxygénation apnéique en salle d’opération, à l’unité de soins intensifs (USI), à l’urgence, et dans des contextes pré-hospitaliers ainsi que de déterminer l’efficacité de cette approche par rapport à des témoins.
Source
Pour ce compte rendu narratif, nous avons obtenu les articles pertinents dans les bases de données MEDLINE® (1946 à avril 2016), EMBASE™ (1974 à avril 2016), Google Scholar et par des recherches manuelles. L’oxygénation apnéique était administrée à l’aide de diverses techniques, notamment l’utilisation de pinces nasales, de sondes nasopharyngées ou endotrachéales, ou de laryngoscopes.
Constatations principales
Premièrement, les 12 études traitant du contexte de la salle d’opération ont toutes démontré que l’oxygénation apnéique prolongeait significativement la durée jusqu’à et l’incidence de désaturation. Deuxièmement, deux des cinq études à l’USI ont montré un déclin significativement réduit de la saturation en oxygène avec l’application d’une oxygénation apnéique, et trois études n’ont montré aucune différence significative d’un point de vue statistique par rapport aux témoins. Enfin, deux études réalisées à l’urgence ou dans un contexte pré-hospitalier ont montré que l’utilisation de l’oxygénation apnéique entraînait une incidence significativement réduite de désaturation et des déclins moindres de la saturation en oxygène.
Conclusion
Seize des 19 études ont montré que l’oxygénation apnéique prolonge le temps d’apnée sécuritaire et réduit l’incidence de désaturation artérielle en oxygène. Globalement, les études examinées dans ce compte rendu montrent que l’oxygénation apnéique prolonge le temps jusqu’à la désaturation en oxygène pendant l’intubation trachéale. Toutefois, la majorité de ces études étaient de petite taille et ne mesuraient pas ou ne possédaient pas la puissance nécessaire pour déceler les complications respiratoires et autres complications graves rares. Une oxygénation apnéique prolongée (avec son hypercarbie conséquente) peut comporter des risques et devrait être évitée chez les patients présentant certaines conditions, notamment une pression intracrânienne élevée, une acidose métabolique, une hyperkaliémie ou une hypertension pulmonaire.
Similar content being viewed by others
Patients with acute respiratory failure or chronic conditions affecting respiratory reserve are at risk of developing hypoxemia, especially during attempts at tracheal intubation. Acute respiratory failure involves conditions such as congestive cardiac failure, exacerbation of chronic obstructive pulmonary disease, and respiratory infection. Chronic conditions compromising respiratory reserve include illnesses such as morbid obesity, chronic obstructive pulmonary disease, and pulmonary fibrosis. During the process of tracheal intubation with an apneic patient, there is a high probability that at-risk patients may become hypoxemic. Apneic oxygenation has been shown to improve arterial oxygen saturation and prolong the duration of safe apneic periods.
The purpose of this review is to examine the literature on the effectiveness of apneic oxygenation in patients undergoing tracheal intubation or airway manipulation in various settings, including the operating room, intensive care unit (ICU), emergency department, and pre-hospital settings.
Physiological mechanism of apneic oxygenation
During regular breathing in an adult, approximately 250 mL·min−1 of oxygen flows from the alveoli into the bloodstream, and 250 mL·min−1 of carbon dioxide returns from the bloodstream to the alveoli. When a patient is apneic, approximately 250 mL·min−1 of oxygen flows from the alveoli into the bloodstream, while only 8-20 mL·min−1 of carbon dioxide returns from the bloodstream to the alveoli. The remaining carbon dioxide produced is buffered in the bloodstream and tissues1,2 (Fig. 1). The difference between the volume of oxygen leaving and carbon dioxide entering creates a negative pressure in the alveoli.1,2 Supplemental oxygen provides an oxygen-rich mixture in the pharynx compared to when no supplemental oxygen is used. As a result of the negative pressure generated, there is a mass movement of gases from the pharynx into the alveoli, provided that the upper airway is patent.1 This process of apneic oxygenation may improve arterial oxygen saturation, prolong the safe apneic period for tracheal intubation, and reduce multiple attempts at laryngoscopy, thereby averting consequent risks of airway or dental trauma.3
Gas exchange during regular breathing and apnea. (a) During regular breathing, O2 moves at a rate of 250 mL·min−1 from the alveoli into the capillaries and into the tissues. Approximately an equal amount of CO2 leaves the tissues and moves into the capillaries and into the alveoli. The volume of gases entering alveoli during inspiration and the volume of gases leaving alveoli during expiration are roughly equal (double arrows in bronchus). (b) During apnea, O2 moves at a rate of 250 mL·min−1 from the alveoli into the capillaries and into the tissues. However, a small amount of CO2 is buffered in the tissues, while a larger amount is buffered in the bloodstream, leaving only 8-20 mL·min−1 to move into the alveoli. The difference in the volume of oxygen leaving and carbon dioxide entering creates a small negative pressure in the alveoli, thereby resulting in a movement of gases from the pharynx into the alveoli (arrow in bronchus towards alveolus)
Various techniques for applying apneic oxygenation
Numerous techniques in the administration of apneic oxygenation have been described (Fig. 2). One such technique is the use of nasal prongs (nasal cannula). A flexible tube with two short protruding prongs is connected to an oxygen source at one end and placed directly under the patient’s nose at the other end. The standard prongs, measuring approximately half the diameter of the nares, are inserted at the entry of the nostrils. A second technique is the use of a nasopharyngeal catheter, which is inserted into the nostril and advanced into the nasopharynx with its distal end lying above the vocal cords. The distance from the nares to the tragus of the ear is often measured and used as an estimate for the depth of catheter insertion.4 A third technique is nasal or oral insertion of a catheter supplying oxygen and passage of the catheter past the vocal cords and into the trachea. A fourth technique is placing bilateral endobronchial catheters in the right and left main stem bronchi to provide apneic oxygenation. Lastly, a laryngoscope can be used whereby oxygen can be delivered through a channel on one side of the laryngoscope blade.
Transnasal humidified high-flow oxygen
Optiflow™ (Fisher & Paykel Healthcare Limited, Laval, QC, Canada) is a recently developed oxygen therapy device that is capable of delivering oxygen via a nasal cannula at higher humidity over a broad range of concentrations and flows (Fig. 3). As a high-flow nasal cannula (HFNC) device, it consists of several main components: a breathing circuit, an oxygen humidification system, contoured nasal prongs, and a head strap (Fig. 4). Optiflow delivers oxygen at a temperature and humidity that matches the environment of healthy adult lungs, which results in improved tolerance by awake patients.5,6 Optiflow can deliver the prescribed oxygen concentration at various flow rates (0-70 L·min−1) and elevate the mean airway pressure proportional to the oxygen flow rate.5,7-11
High-flow nasal cannula system: Optiflow™. (A) Oxygen is supplied through a high-pressure tube connected to a wall oxygen source. (B) Oxygen and entrained room air enter the blender, mixing the two to achieve the desired FiO2 and flow rate. (C) The oxygen mixture flows from the blender to the humidifier. (D) The oxygen mixture is humidified to the desired temperature and humidity level. (E) The humidified oxygen mixture flows from the humidifier to the nasal prongs
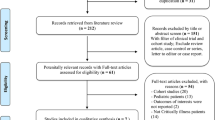
Search strategy for articles cited in this review
MEDLINE® (1946 to April 2016), EMBASE™ (1974 to April 2016), Google Scholar, and manual searches were used to find relevant articles. The following keywords were used in the search: “apneic (or apnoeic) oxygenation”, “ICU”, “emergency”, “artificial respiration”, and “intermittent positive-pressure ventilation”. We included abstracts published in the last three years and full articles with relevance to apneic oxygenation in patients at risk of hypoxemia.
Apneic oxygenation for tracheal intubation in various clinical settings
The use of apneic oxygenation in the operating room (Table 1)
Twelve prospective studies, eight of which are randomized-controlled trials, examined the use of apneic oxygenation in the operating room. Baraka et al.12 studied morbidly obese patients undergoing endotracheal intubation under anesthesia and muscle paralysis in the operating room. Thirty-four patients were randomized to receive either supplemental nasopharyngeal oxygenation (apneic oxygenation group) at a rate of 5 L·min−1 or no supplemental oxygenation (control group). Time to SpO2 < 95% was significantly prolonged in the apneic oxygenation group vs the control group [SpO2 = 100% at 4 min in 16/17 patients vs SpO2 < 95% in a mean (SD) time of 145 (27) sec, respectively; P < 0.05]. Similarly, Ramachandran et al.13 studied 30 obese patients randomized to an apneic oxygenation group receiving oxygen at a rate of 5 L·min−1 via nasal prongs or a control group without apneic oxygenation. The apneic oxygenation group had a significantly longer mean (SD) time to desaturation (SpO2 < 95%) than the control group [5.29 (1.02) min vs 3.49 (1.33) min, respectively; P < 0.05]. In addition, the lowest mean SpO2 recorded was significantly higher in the apneic oxygenation group compared with the control group [94.3 (4.4) % vs 87.7 (9.3) %, respectively; P < 0.05].
In Taha et al.’s14 study, 30 patients were randomized into an apneic oxygenation group receiving oxygen at a rate of 5 L·min−1 via nasopharyngeal catheter or a non-apneic oxygenation control group. The apneic oxygenation group maintained maximum oxygen saturation longer than the control group [SpO2 = 100% at 6 min vs SpO2 < 95% in 3.65 (1.15) min, respectively; P value not stated]. In a crossover study, Teller et al.15 examined 12 patients randomized to an apneic oxygenation group receiving oxygen at a rate of 3 L·min−1 via nasal catheter or a control placebo group, with the two groups switching interventions in the second part of the study. Time to desaturation (SaO2 < 92%) was significantly longer in the apneic oxygenation group compared with the control group [SaO2 > 97% all 10 min vs SaO2 < 92% in 6.8 (0.6) min, respectively; P < 0.01]. The lowest mean SaO2 recorded was significantly higher in the apneic oxygenation group vs the control group [SaO2 = 95% vs SaO2 = 91 (1)%, respectively; P < 0.001].
Christodoulou et al.16 examined the difference amongst patients randomized during tracheal intubation into three groups: apneic oxygenation via nasal prongs at a rate of 5 L·min−1 (n = 13), 10 L·min−1 (n = 14), or no apneic oxygenation control group (n = 14). Apneic oxygenation provided a significant difference in time to desaturation (P = 0.028) compared with the control group. The arterial oxygenation (i.e., PaO2) in the 10 L·min−1 group was significantly higher than both the 5 L·min−1 group and the control group at four minutes (P = 0.004). Lee17 studied 46 patients randomized to an apneic oxygenation group with oxygen rate at 5 L·min−1 via nasal prongs or to a control group without apneic oxygenation. At three minutes, the mean PaO2 decline in the apneic oxygenation group was significantly less than in the control group [PaO2, 479 (48) mmHg to 345 (78) mmHg vs PaO2, 479 (58) mmHg to 256 (81) mmHg, respectively; P < 0.05].
Millar et al.18 compared 17 patients randomized to an apneic oxygenation group receiving 8 L·min−1 of oxygen via an Eschmann® tracheal tube introducer in the trachea extending 2-3 cm beyond the vocal cords or a control group receiving no apneic oxygenation. The apneic oxygenation group had a significantly longer time to desaturation (time taken for SpO2 to fall to 90%) compared with the control group (average of 14 min 14 sec vs 5 min 6 sec, respectively; P < 0.001). Achar et al.4 compared the effectiveness of nasal prongs with that of a nasopharyngeal catheter in providing apneic oxygenation to 56 randomized patients, with both methods insufflating oxygen at a rate of 5 L·min−1. The nasopharyngeal catheter was significantly more effective, as no patient desaturated in the nasopharyngeal group (SpO2 < 95%), while nine patients (32%) desaturated (P = 0.001) in the nasal prongs group.
There were four prospective studies that examined the effectiveness of apneic oxygenation without a control group. In an early study (1959), Frumin et al.19 found that, in eight healthy patients, apneic oxygenation during intubation with an endotracheal catheter maintained adequate SpO2 for 18-55 min, with the lowest SpO2 recorded at 98-100%. Babinski et al.20 performed a study on five females scheduled for elective gynecology procedures and analyzed the effectiveness of 0.6-0.7 L·min−1 of oxygen insufflation via two endobronchial catheters inserted into the right and left main stem bronchi. All patients underwent 30 min of apnea without significant oxygen desaturation [PaO2 = 321 (46) mmHg at the start and 299 (37) mmHg at 30 min). Patel and Nouraei3 studied 25 patients with known difficult airways at high risk of oxygen desaturation during endotracheal intubation. Patients received oxygen via the Optiflow device at 70 L·min−1 using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) until the trachea was successfully intubated. Median [interquartile range (IQR)] apnea time was 14 [9-19] min, and no patient desaturated to SpO2 < 90%.
Rudlof and Hohenhorst2 performed a retrospective study analyzing 47 patients who underwent a panendoscopy under apneic oxygenation at 0.5 L·min−1 using a catheter inserted into the trachea. The median SpO2 at the end of the apneic period was 100%. Additionally, the mean (SD) apnea time was measured to be 24.7 (8.7) min with no adverse effects.
In summary, eight comparative studies showed that apneic oxygenation in the operating room through various routes (nasal, nasopharyngeal, tracheal, or endobronchial administration) prolongs time to oxygen desaturation and reduces the incidence of oxygen desaturation without adverse effects. Four single-device studies also showed maintenance of adequate SpO2 with prolonged apnea.
The use of apneic oxygenation outside the operating room, including the ICU, emergency department, and pre-hospital encounters (Table 2)
Miguel-Montanes et al.21 studied 101 patients requiring tracheal intubation in the ICU. The intervention group (n = 51) received preoxygenation using Optiflow HFNC at 60 L·min−1, which was maintained throughout the intubation. This technique was compared with a control group (n = 50) preoxygenated with a non-rebreathing bag reservoir face mask at 15 L·min−1 for three minutes, followed by 6 L·min−1 via nasopharyngeal catheter during the intubation. High-flow nasal cannula exceeded the control, with a higher median lowest SpO2 (100% vs 94%, respectively; P < 0.0001), a smaller decrease in SpO2 throughout (P < 0.0001), and a lower hypoxemic (SpO2 < 80%) rate (2% vs 14%, respectively; P < 0.03).
In a conference abstract, Vourc’h et al.22 randomized 119 patients into one of two groups. The apneic oxygenation group used Optiflow HFNC at 60 L·min−1 from induction until completion of intubation. The control group received face mask preoxygenation at 15 L·min−1 but no supplemental oxygen during the intubation attempt. The median [IQR] lowest saturation was not significantly different between the apneic oxygenation and control groups (91.5 [80-96]% vs 89.5 [81-95]%, respectively)
Semler et al. 23 randomized 150 patients undergoing tracheal intubation in a medical ICU to receive either 100% oxygen at 15 L·min−1 via HFNC or no supplemental oxygen during laryngoscopy. They found that the median lowest SpO2 was 92% with apneic oxygenation vs 90% with usual care (95% confidence interval [CI] for the difference was -1.6 to 7.4; P = 0.16). There were no statistical differences in the incidence of SpO2 < 90% or SpO2 < 80% between the groups.
In summary, only one dedicated ICU study showed benefits of sustained SpO2 using apneic oxygenation compared with standard preoxygenation in patients requiring tracheal intubation. The other two studies, however, showed no benefit of apneic oxygenation. This discrepancy could be the result of heterogeneity in the underlying ICU population and the severity of pulmonary conditions, the device used to deliver high-flow apneic oxygenation, and variations in the oxygenation techniques used in the control group. Furthermore, many ICU patients have major ventilation-perfusion mismatch and shunting, and supplemental oxygenation may have limited value in improving arterial oxygenation.
There were two studies involving a mixed cohort of patients given tracheal intubation outside the operation room. In a study by Wijewardena et al.,24 patients in the ICU and emergency department receiving apneic oxygenation using HFNC therapy, both during preoxygenation and during intubation (n = 26), were compared with patients receiving standard preoxygenation without apneic oxygenation (n = 10). The decrease in SpO2 in the apneic oxygenation group (HFNC, with one exception) was 0-6%, while the decrease in the standard preoxygenation group was markedly higher, ranging from 0-15% (P value not stated).
Dyett et al. 25 performed a prospective observational study of patients receiving emergency airway management outside the operating theatres. Seventy-six of the 139 patients in their study received apneic oxygenation. Overall, apneic oxygenation did not reduce the incidence of hypoxemia compared with those without apneic oxygenation (19.6% vs 12.8%, respectively; P = 0.316). In a subgroup of patients receiving tracheal intubation for reasons other than respiratory failure, there were 0/31 (0%) hypoxemic episodes in those receiving apneic oxygenation compared with 10/60 (17%) in those without apneic oxygenation (P = 0.016).
One prospective study and one retrospective study analyzed the use of apneic oxygenation in either the emergency department or in an emergency pre-hospital setting. Sakles et al.26 assessed 90 neurologically injured patients in the emergency department undergoing tracheal intubation and compared the difference between patients receiving apneic oxygenation at various levels [5 L·min−1 (n = 9), 10 L·min−1 (n = 4), and ≥ 25 L·min−1 (n = 26)] with patients without apneic oxygenation (n = 51). The apneic oxygenation group had a significantly lower rate of oxygen desaturation (SpO2 < 90%) than the non-apneic oxygenation group (7.7%; 95% CI, 1.6 to 20.9 vs 29.4%; 95% CI, 17.5 to 43.8; respectively; P = 0.03).
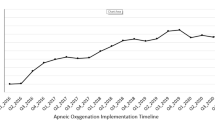
Wimalasena et al.27 retrospectively examined the difference in the incidences of oxygen desaturation (SpO2 < 93%) in a 22-month period in both out-of-hospital and interhospital retrievals. They compared patient outcomes before (n = 310) and after (n = 418) implementation of apneic oxygenation into the rapid sequence intubation protocol. Their study results showed that 22.6% of patients in the pre-apneic oxygenation phase had an episode of desaturation compared with 16.5% of patients in the post-apneic oxygenation phase, resulting in a difference of 6.1% (95% CI, 0.2 to 11.2).
In summary, in four of six studies involving patients undergoing tracheal intubation in ICU, emergency department, and pre-hospital settings, results showed that apneic oxygenation significantly reduces oxygen desaturation when compared with controls. In one observational study in ICU and emergency department patients, apneic oxygenation resulted in no overall reduction in hypoxemia but showed a reduction in hypoxemia in a patient subgroup.
Limitations of apneic oxygenation
Two main factors may limit the application of apneic oxygenation, i.e., elevation of carbon dioxide and rapid sequence intubation. First, apneic oxygenation can be applied for only a limited amount of time. During apneic oxygenation, CO2 levels continue to rise, which can lead to a decrease in pH and the development of severe respiratory acidosis.19,20 , 28 Measurements of mean CO2 levels have ranged from 24.5 mmHg29 to 160 mmHg,19 with CO2 rates increasing from 1.1-3.4 mmHg·min−1.3 The lower rate of CO2 increase during apneic oxygenation was obtained in a study using HFNC.3 Many of the studies do not provide data on patients’ PaCO2 or end-tidal CO2. The mean apneic time ranged from 5.29 min12 to 43 min amongst clinical studies.19 Many study patients tolerated very long periods of apnea. No significant side effects attributed to hypercapnia were reported. It is possible that hypercapnia might have caused physiologic disturbances that were not captured in the study results. Prolonged apneic oxygenation should be avoided in patients with contraindications to hypercapnia, such as those with increased intracranial pressure, hemodynamic instability, and cardiac dysrhythmia. Second, a patent airway is needed for effective apneic oxygenation. Emergency and ICU patients may require rapid sequence intubation with cricoid pressure, which may cause obstruction between the oropharynx and trachea, thereby preventing mass airflow between these spaces during apnea. Despite this concern, emergency and ICU studies have shown apneic oxygenation to be effective. Third, although the majority of studies utilize nasal prongs or nasopharyngeal catheters in the application of apneic oxygenation, several studies use tracheal or endobronchial catheters. It is clinically impractical to place catheters below the glottis for apneic oxygenation.
Limitations of this review
There are a few limitations to this review. First, a publication bias regarding apneic oxygenation may exist among the articles reviewed. It is possible that studies with positive results were published, while studies with negative results were neither submitted nor published. Second, a small sample size in a few of the prospective studies limits the generalizability of the results. Nevertheless, when all studies were analyzed together, 16 out of 19 studies showed beneficial effects of apneic oxygenation while three studies showed no clear benefit.
Finally, oxygenation, specifically, time to oxygen desaturation and oxygen desaturation rate, are the outcome measures used in the majority of the clinical studies. Oxygen saturation is a surrogate outcome variable which, in itself, has little clinical relevance. In contrast, clinically important outcomes, such as adverse respiratory events or adverse cardiac events, were not assessed in the studies. Furthermore, most of the studies have small sample sizes and were not adequately powered to detect adverse respiratory events or other serious rare complications. Large-scale adequately powered well-designed trials are needed to elucidate whether apneic oxygenation will reduce adverse respiratory events and whether the procedure is safe to use in patients at risk of hypoxemia undergoing tracheal intubation.
Practical guide to the application of apneic oxygenation during tracheal intubation in patients at a higher risk of hypoxemia
First, intubation equipment, a skilled operator, and an assistant should be readily available. Second, nasal cannula should be placed securely on the patient and connected to a dedicated oxygen source flowing minimally at 2-5 L·min−1. Third, preoxygenation using a face mask with F i O2 close to 1.0 (anesthesia machine or Ambu® bag with non-rebreathing mask) should be applied. If end-tidal O2 is available, ensure it has reached 85-90%. Fourth, proceed with general anesthesia, muscle relaxation, and bag mask ventilation. Fifth, increase the nasal oxygen flow to 10-15 L·min−1 and remove the face mask. Nasal cannula will provide apneic oxygenation during tracheal intubation. Nasal oxygenation should be continued until tracheal intubation is achieved and confirmed. Finally, apneic oxygenation can have risks and should be used with caution or avoided in clinical situations where hypercarbia could have adverse effects.
Conclusion
This review examined studies pertaining to apneic oxygenation during tracheal intubation in various clinical settings, including the operating room, ICU, emergency department, and pre-hospital situations. All 14 studies in the operating room and emergency departments, and two of five ICU studies, show that apneic oxygenation prolongs time to oxygen desaturation or reduces oxygen desaturation. Nevertheless, the majority of the studies were small in size, did not measure and were not adequately powered to detect adverse respiratory events or other serious rare complications. Prolonged apneic oxygenation (and its consequent hypercarbia) may be risky and should be avoided in patients with conditions such as increased intracranial pressure, metabolic acidosis, hyperkalemia, and pulmonary hypertension.
References
Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med 2012; 59(165-75): e1.
Rudlof B, Hohenhorst W. Use of apneic oxygenation for the performance of pan-endoscopy. Otolaryngol Head Neck Surg 2013; 149: 235-9.
Patel A, Nouraei SA. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015; 70: 323-9.
Achar SK, Pai AJ, Shenoy UK. Apneic oxygenation during simulated prolonged difficult laryngoscopy: comparison of nasal prongs versus nasopharyngeal catheter: a prospective randomized controlled study. Anesth Essays Res 2014; 8: 63-7.
Ritchie JE, Williams AB, Gerard C, Hockey H. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care 2011; 39: 1103-10.
Hasani A, Chapman TH, McCool D, Smith RE, Dilworth JP, Agnew JE. Domiciliary humidification improves lung mucociliary clearance in patients with bronchiectasis. Chron Respir Dis 2008; 5: 81-6.
Roca O, Riera J, Torres F, Masclans JR. High-flow oxygen therapy in acute respiratory failure. Respir Care 2010; 55: 408-13.
Millar JL, Lutton S, O’Connor P. The use of high-flow nasal oxygen therapy in the management of hypercarbic respiratory failure. Ther Adv Respir Dis 2014; 8: 63-4.
Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care 2011; 56: 1151-5.
Lenglet H, Sztrymf B, Leroy C, Brun P, Dreyfuss D, Ricard TD. Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy. Respir Care 2012; 57: 1973-8.
Rello J, Perez M, Roca O, et al. High-flow nasal therapy in adults with severe acute respiratory infection: a cohort study in patients with 2009 influenza A/H1N1v. J Crit Care 2012; 27: 434-9.
Baraka AS, Taha SK, Siddik-Sayyid SM, et al. Supplementation of pre-oxygenation in morbidly obese patients using nasopharyngeal oxygen insufflation. Anaesthesia 2007; 62: 769-73.
Ramachandran SK, Cosnowski A, Shanks A, Turner CR. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth 2010; 22: 164-8.
Taha SK, Siddik-Sayyid SM, El-Khatib MF, Dagher CM, Hakki MA, Baraka AS. Nasopharyngeal oxygen insufflation following pre-oxygenation using the four deep breath technique. Anaesthesia 2006; 61: 427-30.
Teller LE, Alexander CM, Frumin MJ, Gross JB. Pharyngeal insufflation of oxygen prevents arterial desaturation during apnea. Anesthesiology 1988; 69: 980-2.
Christodoulou C, Rohald P, Mullen T, et al. Apneic oxygenation via nasal prongs at 10 L/min prevents hypoxemia during tracheal intubation for elective surgery. European Respiratory Society Annual Congress 2013 (abstract 5356).
Lee SC. Improvement of gas exchange by apneic oxygenation with nasal prong during fiberoptic intubation in fully relaxed patients. J Korean Med Sci 1998; 13: 582-6.
Millar FA, Hutchison GL, Glavin R. Gum elastic bougie, capnography and apnoeic oxygenation. Eur J Anaesthesiol 2001; 18: 51-3.
Frumin MJ, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology 1959; 20: 789-98.
Babinski MF, Sierra OG, Smith RB, Leano E, Chavez A, Castellanos A. Clinical application of continuous flow apneic ventilation. Acta Anaesthesiol Scand 1985; 29: 750-2.
Miguel-Montanes R, Hajage D, Messika J, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med 2015; 43: 574-83.
Vourc’h M, Asfar P, Volteau C, et al. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med 2015; 41: 1538-48.
Semler MW, Janz DR, Lentz RJ, et al. Randomized trial of apneic oxygenation during endotracheal intubation of the critically ill. Am J Respir Crit Care Med 2016; 193: 273-80.
Wijewardena G, Mariyaselvam M, English N, Young P. An audit on the use of High Flow Nasal Oxygen (HFNO) therapy for pre-oxygenation, to reduce the risk of desaturation and making emergency management of airway safer in the anaesthetic and critical care environments. Anaesthesia 2014; 69: abstract 155.
Dyett JF, Moser MS, Tobin AE. Prospective observational study of emergency airway management in the critical care environment of a tertiary hospital in Melbourne. Anaesth Intensive Care 2015; 43: 577-86.
Sakles JC, Patanwala AE, Mosier JM, Dicken JM. Effect of apneic oxygenation on oxygen desaturation during the emergency department intubation of patients with neurologic injury. Society for Academic Emergency Medicine California 2015 (abstract).
Wimalasena Y, Burns B, Reid C, Ware S, Habig K. Apneic oxygenation was associated with decreased desaturation rates during rapid sequence intubation by an Australian helicopter emergency medicine service. Ann Emerg Med 2015; 65: 371-6.
Dragoumanis CP, Papaiannou V, Foutzitzi S, Prassopoulous P, Pneumatikos I. Apnoeic oxygenation for elimination of respiratory motion artefact in an intubated patient undergoing helical computed tomography pulmonary angiography. J Radiol Case Rep 2008; 2: 5-7.
Fraioli RL, Sheffer LA, Steffenson JL. Pulmonary and cardiovascular effects of apneic oxygenation in man. Anesthesiology 1973; 39: 588-96.
Conflict of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author contributions
David Wong and Frances Chung contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Amanda Yee contributed to the conception and design of the article. Amanda Yee and Siaw May Leong contributed to the acquisition, analysis, and interpretation of data and drafting the article.
Financial support and sponsorship
Department of Anesthesia, University Health Network, University of Toronto, Toronto, ON, Canada.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2017; 64: this issue.
An erratum to this article is available at http://dx.doi.org/10.1007/s12630-017-0835-y.
Rights and permissions
About this article
Cite this article
Wong, D.T., Yee, A.J., Leong, S.M. et al. The effectiveness of apneic oxygenation during tracheal intubation in various clinical settings: a narrative review. Can J Anesth/J Can Anesth 64, 416–427 (2017). https://doi.org/10.1007/s12630-016-0802-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-016-0802-z