Abstract
Purpose of Review
Based on retrospective, historic data, surgeons have long recommended mastectomy as the surgical approach for women with multiple ipsilateral synchronous (multifocal or multi-centric) breast cancer (MIBC). In the modern era, however, local recurrence rates have significantly decreased due to improved imaging techniques and earlier detection through breast cancer screening, more accurate delivery of radiation, and the advent of targeted systemic therapies. Given the significant non-surgical advancements in the field of breast cancer care, the role of maximally invasive surgery in improving breast cancer outcomes has diminished. This raises the question as to whether the routine recommendation for mastectomy in MIBC is rooted in current evidence or archaic data. This review summarizes data regarding surgical options for women with MIBC.
Recent Findings
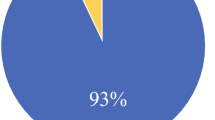
The incidence of MIBC is increasing as a result of improved imaging modalities and the use of breast MRI for breast cancer screening and staging. MIBC tends toward more aggressive biology and higher rates of nodal positivity but recent data contradict the notion that more aggressive surgery improves outcomes. Retrospective studies and meta-analyses performed in the current era of targeted therapy and more sensitive breast cancer detection have demonstrated equivalent rates of local regional recurrence (LRR) in women with MIBC undergoing breast-conserving therapy (BCT) when compared stage to stage with women with unifocal disease. Alliance Z11102, the first national, prospective trial of breast conservation in the MIBC population in the USA, demonstrated the feasibility of BCT in this patient population with acceptable rates of conversion to mastectomy in the MIBC cohort. Prospective data regarding LRR and cosmetic outcomes for women undergoing BCT from completed clinical trials continue to mature, and new randomized clinical trials investigating the biology and treatment of MIBC are under design.
Summary
The incidence of MIBC is increasing due to screening mammography, improved quality of imaging, and the utilization of breast MRI for breast cancer screening and staging. Local regional recurrence rates in women with unifocal disease have decreased due to earlier detection and improved regional and systemic therapy. As adjuvant therapy improves, the extent of surgery is less impactful on LRR and long-term survival. Current data demonstrate acceptable LRR in women undergoing BCT for MIBC for whom negative surgical margins are achieved and appropriate adjuvant therapy is administered. While additional prospective data regarding biology, LRR, cosmesis, and long-term survival in women with MIBC continue to be collected, current evidence supports the role of patient choice in deciding between breast conservation and mastectomy in this population.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wilson LD, Beinfield M, McKhann CF, Haffty BG. Conservative surgery and radiation in the treatment of synchronous ipsilateral breast cancers. Cancer. 1993;72:137–42.
Leopold KA, Recht A, Schnitt SJ, Connolly JL, Rose MA, Silver B, et al. Results of conservative surgery and radiation therapy for multiple synchronous cancers of one breast. Int J Radiat Oncol Biol Phys. 1989;16:11–6.
Kurtz JM, Jacquemier J, Amalric R, et al. Breast-conserving therapy for macroscopically multiple cancers. Ann Surg. 1990;212:38–44.
Hartsell WF, Recine DC, Griem KL, Cobleigh MA, Witt TR, Murthy AK. Should multicentric disease be an absolute contraindication to the use of breast-conserving therapy? Int J Radiat Oncol Biol Phys. 1994;30:49–53 22.
Fowble B, Yeh IT, Schultz DJ, Solin LJ, Rosato EF, Jardines L, et al. The role of mastectomy in patients with stage I-II breast cancer presenting with gross multifocal or multicentric disease or diffuse microcalcifications. Int J Radiat Oncol Biol Phys. 1993;27:567–73.
Wood WC. Should the use of contralateral prophylactic mastectomy be increasing as it is? Breast. 2009;18(Suppl 3):S93–5.
Jones NB, Wilson J, Kotur L, Stephens J, Farrar WB, Agnese DM. Contralateral prophylactic mastectomy for unilateral breast cancer: an increasing trend at a single institution. Ann Surg Oncol. 2009;16:2691–6.
Sorbero ME, Dick AW, Beckjord EB, Ahrendt G. Diagnostic breast magnetic resonance imaging and contralateral prophylactic mastectomy. Ann Surg Oncol. 2009;16:1597–605.
Arrington AK, Jarosek SL, Virnig BA, Habermann EB, Tuttle TM. Patient and surgeon characteristics associated with increased use of contralateral prophylactic mastectomy in patients with breast cancer. Ann Surg Oncol. 2009;16:2697–704.
Wilkinson LS, Given-Wilson R, Hall T, Potts H, Sharma AK, Smith E. Increasing the diagnosis of multifocal primary breast cancer by the use of bilateral whole-breast ultrasound. Clin Radiol. 2005;60:573–8.
Berg WA, Madsen KS, Schilling K, et al. Breast cancer: comparative effectiveness of positron emission mammography and MR imaging in presurgical planning for the ipsilateral breast. Radiology. 2011;258(1):59–72.
• Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RM, Dixon JM, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26:3248–58. This meta-analysis confirms the role of staging breast MRI in the increased detection of MIBC resulting in the need for more extensive surgery.
Moon WK, Noh DY, Im JG. Multifocal, multicentric, and contralateral breast cancers: bilateral whole-breast US in the preoperative evaluation of patients. Radiology. 2002;224:569–76.
Berg WA, Gilbreath PL. Multicentric and multifocal cancer: whole-breast US in preoperative evaluation. Radiology. 2000;214:59–66.
Morrow M, Harris JR. More mastectomies: is this what patients really want? J Clin Oncol. 2009;27:4038–40.
Bleicher RJ, Ciocca RM, Egleston BL, Sesa L, Evers K, Sigurdson ER, et al. Association of routine pretreatment magnetic resonance imaging with time to surgery, mastectomy rate, and margin status. J Am Coll Surg. 2009;209:180–7 quiz 294-5.
Fischer U, Kopka L, Grabbe E. Breast carcinoma: effect of preoperative contrast-enhanced MR imaging on the therapeutic approach. Radiology. 1999;213:881–8.
Bedrosian I, Mick R, Orel SG, Schnall M, Reynolds C, Spitz FR, et al. Changes in the surgical management of patients with breast carcinoma based on preoperative magnetic resonance imaging. Cancer. 2003;98:468–73.
Lee JM, Orel SG, Czerniecki BJ, Solin LJ, Schnall MD. MRI before reexcision surgery in patients with breast cancer. Ajr. 2004;182:473–80.
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9.
Bendifallah S, Werkoff G, Borie-Moutafoff C, Antoine M, Chopier J, Gligorov J, et al. Multiple synchronous (multifocal and multicentric) breast cancer: clinical implications. Surg Oncol. 2010;19(4):e115–23.
Katipamula R, Degnim AC, Hoskin T, Boughey JC, Loprinzi C, Grant CS, et al. Trends in mastectomy rates at the Mayo Clinic Rochester: effect of surgical year and preoperative magnetic resonance imaging. J Clin Oncol. 2009;27:4082–8.
McGuire KP, Santillan AA, Kaur P, et al. Are mastectomies on the rise? A 13-year trend analysis of the selection of mastectomy versus breast conservation therapy in 5865 patients. Ann Surg Oncol. 2009;16:2682–90.
Cho LC, Senzer N, Peters GN. Conservative surgery and radiation therapy for macroscopically multiple ipsilateral invasive breast cancers. Am J Surg. 2002;183:650–4.
Gentilini O, Botteri E, Rotmensz N, da Lima L, Caliskan M, Garcia-Etienne CA, et al. Conservative surgery in patients with multifocal/multicentric breast cancer. Breast Cancer Res Treat. 2009;113:577–83.
Bauman L, Barth RJ, Rosenkranz KM. Breast conservation in women with multifocal-multicentric breast cancer: is it feasible? Ann Surg Oncol. 2010;17(Suppl 3):325–9.
• Ataseven B, Lederer B, Blohmer JU, et al. Impact of multifocal or multicentric disease on surgery and locoregional, distant and overall survival in 6134 breast cancer patients treated with neoadjuvant chemotherapy. Ann Surg Onc. 2015;22(4):1118–27. This trial utilized the patients from large multicenter trials to address the questions of LRFS, DFS, and OS in women with MIBC. It is one of the largest series with 1401 patients with MIBC in comparison with 4733 with unifocal disease. This study also provides insight into the role of neoadjuvant chemotherapy and the impact on outcomes in the MIBC population.
Holland R, Veling DH, et al. Histologic multifocality of Tis, T1-2 breast carcinomas. Implications or clinical trials of breast-conserving surgery. Cancer. 1985;56(5):979–90.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty year follow up of a randomized clinical trial comparing total mastectomy, lumpectomy , and lumpectomy plus radiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
Veronesi U, Cascinellli N, et al. Twenty-year follow up of a randomized study comparing breast conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32.
Schell AM, Rosernkranz K, Lewis P. Role of breast MRI in the preoperative evaluation of patients with newly diagnosed breast cancer. AJR. 2009;192:1438–44.
Lynch SP, Lei X, Hsu L et al. Breast cancer multifocality and multicentricity and locoregional recurrence. Oncologist 2013; 18(11):1167–73.
•• Rosenkranz KM, Ballman K, McCall L, Kubicky C, Cuttino L, le-Petross H, et al. The feasibility of breast-conserving surgery for multiple ipsilateral breast cancer: an initial report from ACOSOG Z11102 (Alliance). Ann Surg Oncol. 2018;25(10):2858–66. This is the first prospective trial to address the issue of MIBC. The trial confirms the feasibility—defined as low conversion to mastectomy rate—of BCT for MIBC.
Kapoor NS, Chung, et al. Preliminary results: double lumpectomies for multicentric breast carcinoma. Am Surg. 2012;78(12):1345–8.
Nijrenhuis M, Rutgers E. Conservative surgery for multifocal/multicentric breast cancer. Breast. 2015;24:S96–9.
•• Yerushalmi R, Tyldesley S, Woods R, Kennecke HF, Speers C, Gelmon KA. Is breast-conserving therapy a safe option for patients with tumor multicentricity and multifocality? Ann Oncol. 2012;23:876–81. This one of the largest and most recent publications which addresses LRR for MIBC when comparing BCT to mastectomy. The results provide insight into risk factors for recurrence. These data may help with patient selection for BCT in the setting of MIBC.
Milulescu A, DiMarino I, et al. Management of multifocal-multicenric breast cancer: current perspective. Chirurgia. 2018;112(1):12–7.
Nos C, Bourgeois D, et al. Conservative treatment of multifocal breast cancer: a comparative study. Bull Cancer. 1999;86(2):184–8.
Kaplan J, Giron G, Tartter PI, Bleiweiss IJ, Estabrook A, Smith SR. Breast conservation in patients with multiple ipsilateral synchronous cancers. J Am Coll Surg. 2003;197(5):726–9.
Oh JL, Dryden MK, et al. Locoregional control of clinically diagnosed multifocal or multicentric breast cancer after neoadjuvant chemotherapy and locoregional therapy. J Clin Oncol. 2006;24(31):4971–5.
Lim W, Park E-H, Choi SL, Seo JY, Kim HJ, Chang MA, et al. Breast conserving surgery for multifocal breast cancer. Ann Surg. 2009;249(1):87–90.
•• Lynch SP, Lei C, et al. Breast cancer and multifocality and multicentricity and locoregional recurrence. Oncologist. 2013;18(11):1167–73. This is one of the largest trials confirming acceptable local recurrence rates in women with MIBC treated with breast conservation. Upon multivariate analysis, the authors concluded that “MIBC” is not an independent risk factor for local recurrence.
Kadioglu H, Yucel S, et al. Feasibility of breast conserving therapy in multifocal breast cancers. Am J Surg. 2014;208:457–64.
National Comprehensive Cancer Network. Clinical practice guidelines in oncology: breast guidelines version 4; 2018.
•• Curigliano G, Bursetin HJ, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the primary therapy of early breast cancer 2017. Ann Oncol. 2017;28(8):1700–12. The St Gallen consensus makes a strong argument for de-escalating surgical care in favor of well-delivered radiation and guideline adherent administration of systemic therapies. The panel supports BCT in MIBC.
Chao SLW, Woo C, et al. Reliable lymphatic drainage to axillary sentinel lymph nodes regardless of tumor location within the breast. Am J Surg. 2001;182:307–11.
Carpenter S, Fraser J, Flemming M, Gray R, Halyard M, Pockaj B. Optimal treatment of multiple ipsilateral primary breast cancers. Am J Surg. 2008;196:530–6.
Veronesi U, Paganelli G, Galimberti V, Viale G, Zurrida S, Bedoni M, et al. Sentinal-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes. Lancet. 1997;349:1864–7.
Fernandez K, Swnason M, Verbanac M. Is sentinel lymphadenectomy accurate in multifocal and multicentric breast cancer? Ann Surg Oncol. 2002;9:S16–7.
• van la Parra RF, de Roos WK, Contant CM, et al. A prospective validation study of sentinel lymph node biopsy in multicentric breast cancer: SMMaC trial. Eur J Surg Oncol. 2014;40:1250–5. This prospective trial confirms the validity of sentinel node excision for MIBC.
Donker M, Straver ME, van Tienhoven G, van de Velde CJH, Mansel RE, Litière S, et al. Comparison of the sentinel node procedure between patients with multifocal and unifocal breast cancer in the EORTC 10981-22023 AMAROS trial: identification rate and nodal outcome. Eur J Cancer. 2013;49(9):2093–100.
Vera-Badillo FE, Napoleone M, Ocana A, Templeton AJ, Seruga B, al-Mubarak M, et al. Effect of multifocality and multicentricity on outcome in early stage breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014;146(2):235–44.
•• Wolters R, Wockel A, et al. Comparing the outcome between multicenric and multifocal breast cancer: what is the impact on survival, and is there a role for guideline-adherent therapy? A retrospective multicenter cohort study of 8,935 patients. Breast Cancer Res Treat. 2013;142(3):579–90. This large retrospective study is critical to understanding the importance of guideline adherent treatment in optimizing outcomes for all women with breast cancer including the MIBC population. These data emphasize the importance of adjuvant therapies in the care of breast cancer patients.
Neri A, Marrelli D, Megha T, Bettarini F, Tacchini D, de Franco L, et al. Clinical significance of multifocal and multicentric breast cancers and choice of surgical treatment: a retrospective study on a series of 1158 cases. BMC Surg. 2015;15(1).
Lynch SP, Lei X, Chavez-MacGregor M, Hsu L, Meric-Bernstam F, Buchholz TA, et al. Multifocality and multicentricity in breast cancer and survival outcomes. Ann Surg Oncol. 2012;23(12):3063–9.
Winters Z, Bernaudo L. Evaluating the current evidence to support therapeutic mammoplasty or breast conserving surgery as an alternative to mastectomy in the treatment of multifocal and multicentric breast cancers. Gland Surg. 2018;7(6):525–35.
Tan MP, Sitoh NY, Sitoh YY. Optimizing breast conservation treatment for multifocal and multicentric breast cancer: a worthwhile endeavor? World J Surg. 2016;40(2):315–22.
Patani N, Carpenter R. Oncologic and aesthetic considerations of conservational surgery for multifocal/multicentric breast cancer. Breast J. 2010;16(3):222–32.
Fung KW, Lau Y, Fielding R, Or A, Yip AW. The impact of mastectomy, breast-conserving treatment and immediate breast reconstruction on the quality of life of Chinese women. ANZ J Surg. 2001;71:202–6.
Zhao R, Qiao Q, Yue Y, Yi SB, Chen L, Chen J, et al. The psychological impact of mastectomy on women with breast cancer. Zhonghua Zheng Xing Wai Ke Za Zhi. 2003;19:294–6.
Kiebert GM, de Haes JC, van de Velde CJ. The impact of breast-conserving treatment and mastectomy on the quality of life of early-stage breast cancer patients: a review. J Clin Oncol. 1991;9:1059–70.
Barlow WE, Taplin SH, Yoshida CK, Buist DS, Seger D, Brown M. Cost comparison of mastectomy versus breast-conserving therapy for early-stage breast cancer. J Natl Cancer Inst. 2001;93:447–55.
Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000;36:1938–43.
Norum J, Olsen JA, Wist EA. Lumpectomy or mastectomy? Is breast conserving surgery too expensive? Breast Cancer Res Treat. 1997;45:7–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The findings/opinions included in this article are that of Jennifer Tonneson and not of the U.S. Air Force Medical Service.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Local-Regional Evaluation and Therapy
Rights and permissions
About this article
Cite this article
Linshaw, D., Tonneson, J. & Rosenkranz, K. Surgical Therapy for Women with Multiple Synchronous Ipsilateral Breast Cancer (MIBC): Current Evidence to Guide Clinical Practice. Curr Breast Cancer Rep 11, 67–73 (2019). https://doi.org/10.1007/s12609-019-0309-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-019-0309-z