Abstract
Purpose of Review
To synthesize the critical role of obesity-associated inflammation, dietary factors, and nutrition in determining breast cancer risk.
Recent Findings
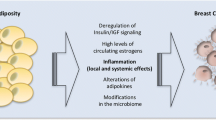
Obesity-associated inflammation is strongly linked to breast cancer risk and progression, largely via two processes: inflammatory pathways and dysregulated metabolism. Cytokine production in excess adipose tissues creates a chronic inflammatory microenvironment, which favors tumor development. Lifestyle factors, including diet, have long been recognized as important determinants of breast cancer risk and mortality.
Summary
Obesity increases the risk of developing breast cancer in both pre- and postmenopausal women and also negatively affects breast cancer recurrence and survival. Poor dietary habits characterized by the high intake of refined starches, sugar, and both saturated and trans-saturated fats, as well as the low intake of omega-3 fatty acids, natural antioxidants, and fiber, modulate inflammation and, thereby, appear to be linked to increased risk of breast cancer and mortality.

Similar content being viewed by others
References
American Cancer Society: Cancer facts & figures 2017. 2017.
Kuchenbaecker KB, Neuhausen SL, Robson M, Barrowdale D, McGuffog L, Mulligan AM, et al. Associations of common breast cancer susceptibility alleles with risk of breast cancer subtypes in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2014;16:3416.
Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9(10) https://doi.org/10.3390/nu9101063.
Rudolph A, Chang-Claude J, Schmidt MK. Gene–environment interaction and risk of breast cancer. Br J Cancer. 2016;114:125.
Theodoratou E, Timofeeva M, Li X, Meng X, Ioannidis JPA. Nature, nurture, and cancer risks: genetic and nutritional contributions to cancer. Annu Rev Nutr. 2017;37(1):293–320. https://doi.org/10.1146/annurev-nutr-071715-051004.
Center for Disease Control and Prevention (CDC). Adult obesity facts. Atlanta: CDC; 2017.
National Institutes of Health (NIH). Overweight and obesity. Bethesda: NIH; 2017.
Jarolimova J, Tagoni J, Stern TA. Obesity: its epidemiology, comorbidities, and management. Prim Care Companion CNS Disord. 2013;15(5):PCC.12f01475.
World Health Organization (WHO). Obesity, 2017.
Dobbins M, Decorby K, Choi BC. The association between obesity and cancer risk: a meta-analysis of observational studies from 1985 to 2011. ISRN Prev Med. 2013;2013:680536.
Ligibel JA, Alfano CM, Courneya KS, Wendy D-W, Burger Robert A, Chlebowski Rowan T, et al. American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol. 2014;32(31):3568–74. https://doi.org/10.1200/JCO.2014.58.4680.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–78. https://doi.org/10.1056/NEJMoa055643.
Patel AV, Hildebrand JS, Gapstur SM. Body mass index and all-cause mortality in a large prospective cohort of white and black U.S. adults. PLoS One. 2014;9(10):e109153.
McDonnell DP, Park S, Goulet MT, Jasper J, Wardell SE, Chang CY, et al. Obesity, cholesterol metabolism, and breast cancer pathogenesis. Cancer Res. 2014;74(18):4976–82. https://doi.org/10.1158/0008-5472.CAN-14-1756.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–78. https://doi.org/10.1016/S0140-6736(08)60269-X.
Matthews SB, Thompson HJ. The obesity-breast cancer conundrum: an analysis of the issues. Int J Mol Sci. 2016;17(6):989. https://doi.org/10.3390/ijms17060989.
Go Y, Chung M, Park Y. Dietary patterns for women with triple-negative breast cancer and dense breasts. Nutr Cancer. 2016;68(8):1281–8. https://doi.org/10.1080/01635581.2016.1225102.
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006;296(2):193–201. https://doi.org/10.1001/jama.296.2.193.
Biganzoli E, Desmedt C, Fornili M, de Azambuja E, Cornez N, Ries F, et al. Recurrence dynamics of breast cancer according to baseline body mass index. Eur J Cancer. 2017;87:10–20. https://doi.org/10.1016/j.ejca.2017.10.007.
Chan DS, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25(10):1901–14. https://doi.org/10.1093/annonc/mdu042.
Dowsett M, Folkerd E. Reduced progesterone levels explain the reduced risk of breast cancer in obese premenopausal women: a new hypothesis. Breast Cancer Res Treat. 2015;149(1):1–4. https://doi.org/10.1007/s10549-014-3211-4.
Nichols HB, Anderson C, White AJ, Milne GL, Sandler DP. Oxidative stress and breast cancer risk in premenopausal women. Epidemiology. 2017;28(5):667–74. https://doi.org/10.1097/EDE.0000000000000685.
Cleary MP, Grossmann ME. Obesity and breast cancer: the estrogen connection. Endocrinology. 2009;150(6):2537–42. https://doi.org/10.1210/en.2009-0070.
Simpson ER, Misso M, Hewitt KN, Hill RA, Boon WC, Jones ME, et al. Estrogen—the good, the bad, and the unexpected. Endocr Rev. 2005;26(3):322–30. https://doi.org/10.1210/er.2004-0020.
Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD. Cardiovascular disease mortality among breast cancer survivors. Epidemiology. 2016;27(1):6–13. https://doi.org/10.1097/EDE.0000000000000394.
Haque R, Prout M, Geiger AM, Kamineni A, Thwin SS, Avila C, et al. Comorbidities and cardiovascular disease risk in older breast cancer survivors. Am J Manag Care. 2014;20(1):86–92.
Pfeiler G. Systemic treatment in premenopausal patients with breast cancer. Breast Care. 2015;10(5):305–6.
Helyer LK, Varnic M, Le LW, Leong W, McCready D. Obesity is a risk factor for developing postoperative lymphedema in breast cancer patients. Breast J. 2010;16(1):48–54. https://doi.org/10.1111/j.1524-4741.2009.00855.x.
McCarthy CM, Mehrara BJ, Riedel E, Davidge K, Hinson A, Disa JJ, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008;121(6):1886–92. https://doi.org/10.1097/PRS.0b013e31817151c4.
Kruk J. Overweight, obesity, oxidative stress and the risk of breast cancer. Asian Pac J Cancer Prev. 2014;15(22):9579–86. https://doi.org/10.7314/APJCP.2014.15.22.9579.
Baek AE, Yu YA, He S, Wardell SE, Chang CY, Kwon S, et al. The cholesterol metabolite 27 hydroxycholesterol facilitates breast cancer metastasis through its actions on immune cells. Nat Commun. 2017;8(1):864. https://doi.org/10.1038/s41467-017-00910-z.
Gilbert CA, Slingerland JM. Cytokines, obesity, and cancer: new insights on mechanisms linking obesity to cancer risk and progression. Annu Rev Med. 2013;64(1):45–57. https://doi.org/10.1146/annurev-med-121211-091527.
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49(11):1603–16. https://doi.org/10.1016/j.freeradbiomed.2010.09.006.
Cole SW, Nagaraja AS, Lutgendorf SK, Green PA, Sood AK. Sympathetic nervous system regulation of the tumour microenvironment. Nat Rev Cancer. 2015;15(9):563–72. https://doi.org/10.1038/nrc3978.
Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014;2014:149185.
Asegaonkar SB, Asegaonkar BN, Takalkar UV, Advani S, Thorat AP. C-reactive protein and breast cancer: new insights from old molecule. Int J Breast Cancer. 2015;2015:145647.
Grimm C, Kantelhardt E, Heinze G, Polterauer S, Zeillinger R, Kolbl H, et al. The prognostic value of four interleukin-1 gene polymorphisms in Caucasian women with breast cancer: a multicenter study. BMC Cancer. 2009;9(1):78. https://doi.org/10.1186/1471-2407-9-78.
Esquivel-Velázquez M, Ostoa-Saloma P, Palacios-Arreola MI, Nava-Castro KE, Castro JI, Morales-Montor J. The role of cytokines in breast cancer development and progression. J Interf Cytokine Res. 2015;35(1):1–16.
Tobias DK, Akinkuolie AO, Chandler PD, Lawler PR, Manson JE, Buring JE, et al. Markers of inflammation and incident breast cancer risk in the women’s health study. Am J Epidemiol. 2017; https://doi.org/10.1093/aje/kwx250.
Wang J, Lee IM, Tworoger SS, Buring JE, Ridker PM, Rosner B, et al. Plasma C-reactive protein and risk of breast cancer in two prospective studies and a meta-analysis. Cancer Epidemiol Biomark Prev. 2015;24(8):1199–206. https://doi.org/10.1158/1055-9965.EPI-15-0187.
Castro AM, Macedo-de la Concha LE, Pantoja-Meléndez CA. Low-grade inflammation and its relation to obesity and chronic degenerative diseases. Rev Méd Hosp Gen Méx. 2017;80(2):101–5. https://doi.org/10.1016/j.hgmx.2016.06.011.
Dias JA, Fredrikson GN, Ericson U, Gullberg B, Hedblad B, Engstrom G, et al. Low-grade inflammation, oxidative stress and risk of invasive post-menopausal breast cancer—a nested case-control study from the Malmo diet and cancer cohort. PLoS One. 2016;11(7):e0158959. https://doi.org/10.1371/journal.pone.0158959.
Ye J. Emerging role of adipose tissue hypoxia in obesity and insulin resistance. Int J Obes. 2009;33(1):54–66. https://doi.org/10.1038/ijo.2008.229.
Johnson AR, Milner JJ, Makowski L. The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev. 2012;249(1):218–38. https://doi.org/10.1111/j.1600-065X.2012.01151.x.
Lumeng CN, DelProposto JB, Westcott DJ, Saltiel AR. Phenotypic switching of adipose tissue macrophages with obesity is generated by spatiotemporal differences in macrophage subtypes. Diabetes. 2008;57(12):3239–46. https://doi.org/10.2337/db08-0872.
Vaysse C, Lomo J, Garred O, Fjeldheim F, Lofteroed T, Schlichting E, et al. Inflammation of mammary adipose tissue occurs in overweight and obese patients exhibiting early-stage breast cancer. NPJ Breast Cancer. 2017;3(1):19. https://doi.org/10.1038/s41523-017-0015-9.
Vona-Davis L, Rose DP. Angiogenesis, adipokines and breast cancer. Cytokine Growth Factor Rev. 2009;20(3):193–201. https://doi.org/10.1016/j.cytogfr.2009.05.007.
Lago F, Dieguez C, Gomez-Reino J, Gualillo O. Adipokines as emerging mediators of immune response and inflammation. Nat Clin Pract Rheumatol. 2007;3(12):716–24. https://doi.org/10.1038/ncprheum0674.
Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111–7. https://doi.org/10.1172/JCI57132.
Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29(7):1585–90. https://doi.org/10.2337/dc06-0057.
Tabassum I, Mahmood H, Faheem M. Type 2 diabetes mellitus as a risk factor for female breast cancer in the population of Northern Pakistan. Asian Pac J Cancer Prev. 2016;17(7):3255–8.
Nieto-Vazquez I, Fernandez-Veledo S, Kramer DK, Vila-Bedmar R, Garcia-Guerra L, Lorenzo M. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114(3):183–94. https://doi.org/10.1080/13813450802181047.
Greenberg AS, Nordan RP, McIntosh J, Calvo JC, Scow RO, Jablons D. Interleukin 6 reduces lipoprotein lipase activity in adipose tissue of mice in vivo and in 3T3-L1 adipocytes: a possible role for interleukin 6 in cancer cachexia. Cancer Res. 1992;52(15):4113–6.
Ferroni P, Riondino S, Buonomo O, Palmirotta R, Guadagni F, Roselli M. Type 2 diabetes and breast cancer: the interplay between impaired glucose metabolism and oxidant stress. Oxidative Med Cell Longev. 2015;2015:183928.
Padgett DA, Glaser R. How stress influences the immune response. Trends Immunol. 2003;24(8):444–8. https://doi.org/10.1016/S1471-4906(03)00173-X.
Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21(3):159–65. https://doi.org/10.1016/j.tem.2009.10.004.
Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5(3):243–51. https://doi.org/10.1038/nri1571.
Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res. 2014;58(2–3):193–210. https://doi.org/10.1007/s12026-014-8517-0.
Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–92. https://doi.org/10.1093/aje/kwp104.
Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry. 2013;73(9):827–35. https://doi.org/10.1016/j.biopsych.2013.01.032.
Bergmann N, Gyntelberg F, Faber J. The appraisal of chronic stress and the development of the metabolic syndrome: a systematic review of prospective cohort studies. Endocr Connect. 2014;3(2):R55–80. https://doi.org/10.1530/EC-14-0031.
Troxel WM, Matthews KA, Gallo LC, Kuller LH. Marital quality and occurrence of the metabolic syndrome in women. Arch Intern Med. 2005;165(9):1022–7. https://doi.org/10.1001/archinte.165.9.1022.
Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5–6):231–7. https://doi.org/10.1242/dmm.001180.
Oliver G, Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62(6):853–65. https://doi.org/10.1097/00006842-200011000-00016.
Kiecolt-Glaser JK, Habash DL, Fagundes CP, Andridge R, Peng J, Malarkey WB, et al. Daily stressors, past depression, and metabolic responses to high-fat meals: a novel path to obesity. Biol Psychiatry. 2015;77(7):653–60. https://doi.org/10.1016/j.biopsych.2014.05.018.
Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140(3):774–815. https://doi.org/10.1037/a0035302.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9. https://doi.org/10.1001/archgenpsychiatry.2010.2.
Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med. 2010;72(4):365–9. https://doi.org/10.1097/PSY.0b013e3181dbf489.
Macon M, Sumis A, Yu W, Hilakivi-Clarke L. Abstract LB-316: social isolation alters abdominal and mammary adipocytes to potentially increase mammary tumorigenesis in mice. Cancer Res. 2016;76(14 Supplement):LB-316.
World Cancer Research Fund International/American Institute for Cancer Research. Cancer preventability estimates. Washington DC: AICR; 2017.
Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S, et al. Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev. 2017;75(6):405–19. https://doi.org/10.1093/nutrit/nux012.
Belardi V, Gallagher EJ, Novosyadlyy R, LeRoith D. Insulin and IGFs in obesity-related breast cancer. J Mammary Gland Biol Neoplasia. 2013;18(3–4):277–89. https://doi.org/10.1007/s10911-013-9303-7.
Jenkins DJ, Kendall CW, Augustin LS, Franceschi S, Hamidi M, Marchie A, et al. Glycemic index: overview of implications in health and disease. Am J Clin Nutr. 2002;76(1):266s–73s.
Rose DP, Vona-Davis L. The cellular and molecular mechanisms by which insulin influences breast cancer risk and progression. Endocr Relat Cancer. 2012;19(6):R225–41. https://doi.org/10.1530/ERC-12-0203.
Mullie P, Koechlin A, Boniol M, Autier P, Boyle P. Relation between breast cancer and high glycemic index or glycemic load: a meta-analysis of prospective cohort studies. Crit Rev Food Sci Nutr. 2016;56(1):152–9. https://doi.org/10.1080/10408398.2012.718723.
Dong JY, Qin LQ. Dietary glycemic index, glycemic load, and risk of breast cancer: meta-analysis of prospective cohort studies. Breast Cancer Res Treat. 2011;126(2):287–94. https://doi.org/10.1007/s10549-011-1343-3.
Sieri S, Agnoli C, Pala V, Grioni S, Brighenti F, Pellegrini N, et al. Dietary glycemic index, glycemic load, and cancer risk: results from the EPIC-Italy study. Sci Rep. 2017;7(1):9757. https://doi.org/10.1038/s41598-017-09498-2.
Champ CE, Volek JS, Siglin J, Jin L, Simone NL. Weight gain, metabolic syndrome, and breast cancer recurrence: are dietary recommendations supported by the data? Int J Breast Cancer. 2012;2012:506868.
Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JAE, Stampfer MJ, et al. Red meat consumption and mortality: results from two prospective cohort studies. Arch Intern Med. 2012;172(7):555–63.
Taylor EF, Burley VJ, Greenwood DC, Cade JE. Meat consumption and risk of breast cancer in the UK women’s cohort study. Br J Cancer. 2007;96(7):1139–46. https://doi.org/10.1038/sj.bjc.6603689.
Fu Z, Deming SL, Fair AM, Shrubsole MJ, Wujcik DM, Shu X-O, et al. Well-done meat intake and meat-derived mutagen exposures in relation to breast cancer risk: the Nashville Breast Health Study. Breast Cancer Res Treat. 2011;129(3):919–28.
Inoue-Choi M, Sinha R, Gierach GL, Ward MH. Red and processed meat, nitrite, and heme iron intakes and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Int J Cancer. 2016;138(7):1609–18. https://doi.org/10.1002/ijc.29901.
Lee H-J, Wu K, Cox DG, Hunter D, Hankinson SE, Willett WC, Sinha R, Cho E. Polymorphisms in xenobiotic metabolizing genes, intakes of heterocyclic amines and red meat, and postmenopausal breast cancer. Nutr Cancer. 2013;65(8). https://doi.org/10.1080/01635581.2013.824991.
Sieri S, Chiodini P, Agnoli C, Pala V, Berrino F, Trichopoulou A, et al. Dietary fat intake and development of specific breast cancer subtypes. J Natl Cancer Inst. 2014;106(5) https://doi.org/10.1093/jnci/dju068.
Xia H, Ma S, Wang S, Sun G. Meta-analysis of saturated fatty acid intake and breast cancer risk. Medicine. 2015;94(52):e2391.
Playdon MC, Ziegler RG, Sampson JN, Stolzenberg-Solomon R, Thompson HJ, Irwin ML, et al. Nutritional metabolomics and breast cancer risk in a prospective study. Am J Clin Nutr. 2017;106(2):637–49. https://doi.org/10.3945/ajcn.116.150912.
Micha R, Mozaffarian D. Trans fatty acids: effects on metabolic syndrome, heart disease and diabetes. Nat Rev Endocrinol. 2009;5(6):335–44. https://doi.org/10.1038/nrendo.2009.79.
Chajes V, Thiebaut AC, Rotival M, Gauthier E, Maillard V, Boutron-Ruault MC, et al. Association between serum trans-monounsaturated fatty acids and breast cancer risk in the E3N-EPIC study. Am J Epidemiol. 2008;167(11):1312–20. https://doi.org/10.1093/aje/kwn069.
Wang J, John EM, Horn-Ross PL, Ingles SA. Dietary fat, cooking fat, and breast cancer risk in a multiethnic population. Nutr Cancer. 2008;60(4):492–504. https://doi.org/10.1080/01635580801956485.
Lachenmeier DW, Przybylski MC, Rehm J. Comparative risk assessment of carcinogens in alcoholic beverages using the margin of exposure approach. Int J Cancer. 2012;131(6):E995–1003. https://doi.org/10.1002/ijc.27553.
Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112(3):580–93. https://doi.org/10.1038/bjc.2014.579.
Romieu I, Scoccianti C, Chajes V, de Batlle J, Biessy C, Dossus L, et al. Alcohol intake and breast cancer in the European prospective investigation into cancer and nutrition. Int J Cancer. 2015;137(8):1921–30.
Lowry SJ, Kapphahn K, Chlebowski R, Li CI. Alcohol use and breast cancer survival among participants in the Women’s Health Initiative. Cancer Epidemiol Biomark Prev. 2016;25(8):1268–73. https://doi.org/10.1158/1055-9965.EPI-16-0151.
Lachenmeier DW, Rehm J. Moderate red wine drinking does not help cut women’s breast cancer risk. J Women's Health. 2012;21(4):469–70.
Patterson E, Wall R, Fitzgerald GF, Ross RP, Stanton C. Health implications of high dietary omega-6 polyunsaturated fatty acids. J Nutr Metab. 2012;2012:539426.
Azrad M, Turgeon C, Demark-Wahnefried W. Current evidence linking polyunsaturated fatty acids with cancer risk and progression. Front Oncol. 2013;3:224.
Bagga D, Capone S, Wang HJ, Heber D, Lill M, Chap L, et al. Dietary modulation of omega-3/omega-6 polyunsaturated fatty acid ratios in patients with breast cancer. J Natl Cancer Inst. 1997;89(15):1123–31. https://doi.org/10.1093/jnci/89.15.1123.
Fay MP, Freedman LS, Clifford CK, Midthune DN. Effect of different types and amounts of fat on the development of mammary tumors in rodents: a review. Cancer Res. 1997;57(18):3979–88.
Kiyabu GY, Inoue M, Saito E, Abe SK, Sawada N, Ishihara J, et al. Fish, n-3 polyunsaturated fatty acids and n-6 polyunsaturated fatty acids intake and breast cancer risk: the Japan Public Health Center-based prospective study. Int J Cancer. 2015;137(12):2915–26. https://doi.org/10.1002/ijc.29672.
Abdelmagid SA, MacKinnon JL, Janssen SM, Ma DW. Role of n-3 polyunsaturated fatty acids and exercise in breast cancer prevention: identifying common targets. Nutr Metab Insights. 2016;9:71–84. https://doi.org/10.4137/NMI.S39043.
Lin PY, Huang SY, Su KP. A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression. Biol Psychiatry. 2010;68(2):140–7. https://doi.org/10.1016/j.biopsych.2010.03.018.
Michaeli B, Berger MM, Revelly JP, Tappy L, Chiolero R. Effects of fish oil on the neuro-endocrine responses to an endotoxin challenge in healthy volunteers. Clin Nutr. 2007;26(1):70–7. https://doi.org/10.1016/j.clnu.2006.06.001.
Ju-Sheng Zheng, Xiao-Jie Hu, Yi-Min Zhao, Jing Yang, Duo Li. Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. BMJ. 2013;346.
Zhihui W, Weihua Y, Zupei W, Jinlin H. Fish consumption and risk of breast cancer: meta-analysis of 27 observational studies. Nutr Hosp. 2016;33(3):282. https://doi.org/10.20960/nh.282.
Chen G-C, Yang J, Eggersdorfer M, Zhang W, Qin L-Q. N-3 long-chain polyunsaturated fatty acids and risk of all-cause mortality among general populations: a meta-analysis. Sci Rep. 2016;6:28165.
Kiecolt-Glaser JK, Epel ES, Belury MA, Andridge R, Lin J, Glaser R, et al. Omega-3 fatty acids, oxidative stress, and leukocyte telomere length: a randomized controlled trial. Brain Behav Immun. 2013;28:16–24. https://doi.org/10.1016/j.bbi.2012.09.004.
Hirko KA, Chai B, Spiegelman D, Campos H, Farvid MS, Hankinson SE, et al. Erythrocyte membrane fatty acids and breast cancer risk: a prospective analysis in the Nurses’ Health Study II. Int J Cancer. 2017; https://doi.org/10.1002/ijc.31133.
Khankari NK, Bradshaw PT, Steck SE, He K, Olshan AF, Shen J, et al. Polyunsaturated fatty acid interactions and breast cancer incidence: a population-based case-control study on Long Island, New York. Ann Epidemiol. 2015;25(12):929–35. https://doi.org/10.1016/j.annepidem.2015.09.003.
Schwingshackl L, Hoffmann G. Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis. 2014;24(9):929–39. https://doi.org/10.1016/j.numecd.2014.03.003.
He J, Gu Y, Zhang S. Consumption of vegetables and fruits and breast cancer survival: a systematic review and meta-analysis. Sci Rep. 2017;7(1):599. https://doi.org/10.1038/s41598-017-00635-5.
Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46(3):1029–56. https://doi.org/10.1093/ije/dyw319.
Narita S, Inoue M, Saito E, Abe SK, Sawada N, Ishihara J, et al. Dietary fiber intake and risk of breast cancer defined by estrogen and progesterone receptor status: the Japan Public Health Center-based prospective study. Cancer Causes Control. 2017;28(6):569–78. https://doi.org/10.1007/s10552-017-0881-3.
Anderson C, Harrigan M, George SM, Ferrucci LM, Sanft T, Irwin ML, et al. Changes in diet quality in a randomized weight loss trial in breast cancer survivors: the lifestyle, exercise, and nutrition (LEAN) study. NPJ Breast Cancer. 2016;2(1):16026. https://doi.org/10.1038/npjbcancer.2016.26.
Zhang CX, Ho SC, Chen YM, Fu JH, Cheng SZ, Lin FY. Greater vegetable and fruit intake is associated with a lower risk of breast cancer among Chinese women. Int J Cancer. 2009;125(1):181–8. https://doi.org/10.1002/ijc.24358.
Griffiths K, Aggarwal BB, Singh RB, Buttar HS, Wilson D, De Meester F. Food antioxidants and their anti-inflammatory properties: a potential role in cardiovascular diseases and cancer prevention. Diseases. 2016;4(3) https://doi.org/10.3390/diseases4030028.
Bakker MF, Peeters PH, Klaasen VM, Bueno-de-Mesquita HB, Jansen EH, Ros MM, et al. Plasma carotenoids, vitamin C, tocopherols, and retinol and the risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition cohort. Am J Clin Nutr. 2016;103(2):454–64.
Eliassen AH, Hendrickson SJ, Brinton LA, Buring JE, Campos H, Dai Q, et al. Circulating carotenoids and risk of breast cancer: pooled analysis of eight prospective studies. J Natl Cancer Inst. 2012;104(24):1905–16. https://doi.org/10.1093/jnci/djs461.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81. https://doi.org/10.1056/NEJMra070553.
Egnell M, Fassier P, Lecuyer L, Zelek L, Vasson MP, Hercberg S, Latino-Martel P, Galan P, Deschasaux M, Touvier M. B-vitamin intake from diet and supplements and breast cancer risk in middle-aged women: results from the prospective NutriNet-Sante cohort. Nutrients. 2017;9(5). doi: https://doi.org/10.3390/nu9050488.
Shao T, Klein P, Grossbard ML. Vitamin D and breast cancer. Oncologist. 2012;17(1):36–45.
Hines SL, Jorn HK, Thompson KM, Larson JM. Breast cancer survivors and vitamin D: a review. Nutrition. 2010;26(3):255–62. https://doi.org/10.1016/j.nut.2009.08.020.
Hardman WE. Walnuts have potential for cancer prevention and treatment in mice. J Nutr. 2014;144(4):555S–60S. https://doi.org/10.3945/jn.113.188466.
Gonzalez CA, Salas-Salvado J. The potential of nuts in the prevention of cancer. Br J Nutr. 2006;96(Suppl 2):S87–94. https://doi.org/10.1017/BJN20061868.
Chlebowski RT, Aragaki AK, Anderson GL, Thomson CA, Manson JE, Simon MS, et al. Low-fat dietary pattern and breast cancer mortality in the Women’s Health Initiative randomized controlled trial. J Clin Oncol. 2017;35(25):2919–26. https://doi.org/10.1200/JCO.2016.72.0326.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002.
Zuniga KE, Mackenzie MJ, Roberts SA, Raine LB, Hillman CH, Kramer AF, et al. Relationship between fruit and vegetable intake and interference control in breast cancer survivors. Eur J Nutr. 2016;55(4):1555–62. https://doi.org/10.1007/s00394-015-0973-3.
Zang J, Shen M, Du S, Chen T, Zou S. The association between dairy intake and breast cancer in western and Asian populations: a systematic review and meta-analysis. J Breast Cancer. 2015;18(4):313–22. https://doi.org/10.4048/jbc.2015.18.4.313.
Hoffmann G, Schwingshackl L. Mediterranean diet supplemented with extra virgin olive oil reduces the incidence of invasive breast cancer in a randomised controlled trial. Evid Based Med. 2016;21(2):72. https://doi.org/10.1136/ebmed-2015-110366.
Mourouti N, Panagiotakos DB. The beneficial effect of a Mediterranean diet supplemented with extra virgin olive oil in the primary prevention of breast cancer among women at high cardiovascular risk in the PREDIMED trial. Evid Based Nurs. 2016;19(3):71. https://doi.org/10.1136/ebnurs-2016-102303.
Skouroliakou M, Grosomanidis D, Massara P, Kostara C, Papandreou P, Ntountaniotis D, et al. Serum antioxidant capacity, biochemical profile and body composition of breast cancer survivors in a randomized Mediterranean dietary intervention study. Eur J Nutr. 2017; https://doi.org/10.1007/s00394-017-1489-9.
Tabung FK, Steck SE, Liese AD, Zhang J, Ma Y, Johnson KC, et al. Patterns of change over time and history of the inflammatory potential of diet and risk of breast cancer among postmenopausal women. Breast Cancer Res Treat. 2016;159(1):139–49. https://doi.org/10.1007/s10549-016-3925-6.
Shivappa N, Sandin S, Lof M, Hebert JR, Adami HO, Weiderpass E. Prospective study of dietary inflammatory index and risk of breast cancer in Swedish women. Br J Cancer. 2015;113(7):1099–103. https://doi.org/10.1038/bjc.2015.304.
Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16(16):1599–600. https://doi.org/10.1016/S1470-2045(15)00444-1.
Kotepui M. Diet and risk of breast cancer. Contemp Oncol. 2016;20(1):13–9.
Cowen S, McLaughlin SL, Hobbs G, Coad J, Martin KH, Olfert IM, et al. High-fat, high-calorie diet enhances mammary carcinogenesis and local inflammation in MMTV-PyMT mouse model of breast cancer. Cancers (Basel). 2015;7(3):1125–42. https://doi.org/10.3390/cancers7030828.
Lopez-Garcia E, Schulze MB, Fung TT, Meigs JB, Rifai N, Manson JE, et al. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2004;80(4):1029–35.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hebert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96. https://doi.org/10.1017/S1368980013002115.
Tabung FK, Steck SE, Liese AD, Zhang J, Ma Y, Caan B, et al. Association between dietary inflammatory potential and breast cancer incidence and death: results from the Women’s Health Initiative. Br J Cancer. 2016;114(11):1277–85. https://doi.org/10.1038/bjc.2016.98.
Milner JA. Molecular targets for bioactive food components. J Nutr. 2004;134(9):2492s–8s.
Calder PC, Albers R, Antoine JM, Blum S, Bourdet-Sicard R, Ferns GA, et al. Inflammatory disease processes and interactions with nutrition. Br J Nutr. 2009;101(Suppl 1):S1–45.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48. https://doi.org/10.1016/j.clnu.2016.07.015.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. https://doi.org/10.1016/j.clnu.2016.09.004.
Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187–96. https://doi.org/10.1016/j.clnu.2017.06.017.
Pekmezi DW, Demark-Wahnefried W. Updated evidence in support of diet and exercise interventions in cancer survivors. Acta Oncol. 2011;50(2):167–78. https://doi.org/10.3109/0284186X.2010.529822.
Aoyagi T, Terracina KP, Raza A, Matsubara H, Takabe K. Cancer cachexia, mechanism and treatment. World J Gastrointest Oncol. 2015;7(4):17–29.
Blackburn GL, Wang KA. Dietary fat reduction and breast cancer outcome: results from the Women’s Intervention Nutrition Study (WINS). Am J Clin Nutr. 2007;86(3):s878–81.
Parry BM, Milne JM, Yadegarfar G, Rainsbury RM. Dramatic dietary fat reduction is feasible for breast cancer patients: results of the randomised study, WINS (UK)—stage 1. Eur J Surg Oncol. 2011;37(10):848–55. https://doi.org/10.1016/j.ejso.2011.07.010.
Halfdanarson TR, Thordardottir E, West CP, Jatoi A. Does dietary counseling improve quality of life in cancer patients? A systematic review and meta-analysis. J Support Oncol. 2008;6(5):234–7.
Colomer R, Moreno-Nogueira JM, Garcia-Luna PP, Garcia-Peris P, Garcia-de-Lorenzo A, Zarazaga A, et al. N-3 fatty acids, cancer and cachexia: a systematic review of the literature. Br J Nutr. 2007;97(5):823–31. https://doi.org/10.1017/S000711450765795X.
Alfano CM, Imayama I, Neuhouser ML, Kiecolt-Glaser JK, Smith AW, Meeske K, et al. Fatigue, inflammation, and omega-3 and omega-6 fatty acid intake among breast cancer survivors. J Clin Oncol. 2012;30(12):1280–7. https://doi.org/10.1200/JCO.2011.36.4109.
Shapira N. The potential contribution of dietary factors to breast cancer prevention. Eur J Cancer Prev. 2017;26(5):385–95. https://doi.org/10.1097/CEJ.0000000000000406.
George SM, Ballard-Barbash R, Shikany JM, Caan BJ, Freudenheim JL, Kroenke CH, et al. Better postdiagnosis diet quality is associated with reduced risk of death among postmenopausal women with invasive breast cancer in the Women’s Health Initiative. Cancer Epidemiol Biomark Prev. 2014;23(4):575–83.
Vrieling A, Buck K, Seibold P, Heinz J, Obi N, Flesch-Janys D, et al. Dietary patterns and survival in German postmenopausal breast cancer survivors. Br J Cancer. 2013;108(1):188–92. https://doi.org/10.1038/bjc.2012.521.
Kwan ML, Weltzien E, Kushi LH, Castillo A, Slattery ML, Caan BJ. Dietary patterns and breast cancer recurrence and survival among women with early-stage breast cancer. J Clin Oncol. 2009;27(6):919–26. https://doi.org/10.1200/JCO.2008.19.4035.
Finocchiaro C, Ossola M, Monge T, Fadda M, Brossa L, Caudera V, et al. Effect of specific educational program on dietary change and weight loss in breast-cancer survivors. Clin Nutr. 2016;35(4):864–70. https://doi.org/10.1016/j.clnu.2015.05.018.
Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC. Adolescent meat intake and breast cancer risk. Int J Cancer. 2015;136(8):1909–20. https://doi.org/10.1002/ijc.29218.
Bertrand KA, Burian RA, Eliassen AH, Willett WC, Tamimi RM. Adolescent intake of animal fat and red meat in relation to premenopausal mammographic density. Breast Cancer Res Treat. 2016;155(2):385–93. https://doi.org/10.1007/s10549-016-3679-1.
Yaghjyan L, Ghita GL, Rosner B, Farvid M, Bertrand KA, Tamimi RM. Adolescent fiber intake and mammographic breast density in premenopausal women. Breast Cancer Res. 2016;18(1):85. https://doi.org/10.1186/s13058-016-0747-8.
Harris HR, Willett WC, Vaidya RL, Michels KB. An adolescent and early adulthood dietary pattern associated with inflammation and the incidence of breast cancer. Cancer Res. 2017;77(5):1179–87. https://doi.org/10.1158/0008-5472.CAN-16-2273.
Arikawa AY, Kaufman BC, Raatz SK, Kurzer MS. Effects of a parallel-arm randomized controlled weight loss pilot study on biological and psychosocial parameters of overweight and obese breast cancer survivors. Pilot Feasibility Stud. 2017;4:17.
Demark-Wahnefried W, Peterson B, McBride C, Lipkus I, Clipp E. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000;88(3):674–84. https://doi.org/10.1002/(SICI)1097-0142(20000201)88:3<674::AID-CNCR26>3.0.CO;2-R.
Zhang FF, Liu S, John EM, Must A, Demark-Wahnefried W. Diet quality of cancer survivors and noncancer individuals: results from a national survey. Cancer. 2015;121(23):4212–21. https://doi.org/10.1002/cncr.29488.
Klassen AC, Smith KC, Shuster M, Coa KI, Caulfield LE, Helzlsouer KJ, Peairs KS, Shockney LD, Stoney D, Hannum S. We’re just not prepared for eating over our whole life”: a mixed methods approach to understanding dietary behaviors among longer term cancer survivors. Integr Cancer Ther. 2017. p. 1534735417731515.
Braakhuis A, Campion P, Bishop K. The effects of dietary nutrition education on weight and health biomarkers in breast cancer survivors. Med Sci (Basel). 2017;5(2)
Christifano DN, Fazzino TL, Sullivan DK, Befort CA. Diet quality of breast cancer survivors after a six-month weight management intervention: improvements and association with weight loss. Nutr Cancer. 2016;68(8):1301–8. https://doi.org/10.1080/01635581.2016.1224368.
Delgado-Cruzata L, Zhang W, McDonald JA, Tsai WY, Valdovinos C, Falci L, et al. Dietary modifications, weight loss, and changes in metabolic markers affect global DNA methylation in Hispanic, African American, and Afro-Caribbean breast cancer survivors. J Nutr. 2015;145(4):783–90. https://doi.org/10.3945/jn.114.202853.
Harrigan M, Cartmel B, Loftfield E, Sanft T, Chagpar AB, Zhou Y, et al. Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: the lifestyle, exercise, and nutrition (LEAN) study. J Clin Oncol. 2016;34(7):669–76. https://doi.org/10.1200/JCO.2015.61.6375.
Hamer J, Warner E. Lifestyle modifications for patients with breast cancer to improve prognosis and optimize overall health. CMAJ. 2017;189(7):E268–e274. https://doi.org/10.1503/cmaj.160464.
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1):30–67. https://doi.org/10.3322/caac.20140.
Campbell KL, Foster-Schubert KE, Alfano CM, Wang CC, Wang CY, Duggan CR, et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. J Clin Oncol. 2012;30(19):2314–26. https://doi.org/10.1200/JCO.2011.37.9792.
Jackson SE, Heinrich M, Beeken RJ, Wardle J. Weight loss and mortality in overweight and obese cancer survivors: a systematic review. PLoS One. 2017;12(1):e0169173. https://doi.org/10.1371/journal.pone.0169173.
WCRF. World Cancer Research Fund International. Continuous update project (Cup). 2017.
Norat T, Scoccianti C, Boutron-Ruault MC, Anderson A, Berrino F, Cecchini M, et al. European code against cancer 4th edition: diet and cancer. Cancer Epidemiol. 2015;39(Suppl 1):S56–66. https://doi.org/10.1016/j.canep.2014.12.016.
Cottet V, Touvier M, Fournier A, Touillaud MS, Lafay L, Clavel-Chapelon F, et al. Postmenopausal breast cancer risk and dietary patterns in the E3N-EPIC prospective cohort study. Am J Epidemiol. 2009;170(10):1257–67. https://doi.org/10.1093/aje/kwp257.
National Comprehensive Cancer Network (NCCN), NCCN clinical practice guidelines in oncology. Breast Cancer 2017, NCCN.
Funding
Annina Seiler received funding from the Swiss National Science Foundation (SNSF) (P2FRP1-168479).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any conflict of interests to declare
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Psycho-Oncology and Supportive Care
Rights and permissions
About this article
Cite this article
Seiler, A., Chen, M.A., Brown, R.L. et al. Obesity, Dietary Factors, Nutrition, and Breast Cancer Risk. Curr Breast Cancer Rep 10, 14–27 (2018). https://doi.org/10.1007/s12609-018-0264-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-018-0264-0