Abstract
As a probiotic, Weizmannia coagulans (W. coagulans) is often used in food and medicine to regulate intestinal flora and exert anti-inflammatory effects. In this study, the anti-acne efficacy and mechanism of extracellular proteins (YTCY-EPs) from W. coagulans YTCY strain are analyzed. The main components of YTCY-EPs, extracted and separated from the fermentation broth, are peptides ranging from 1.51 to 11.44 kDa, accounting for about 80%. Among the peptides identified by LC/MS–MS, YTCY_A-F possess the properties of antimicrobial peptides, while YTCY_1-4 possess antioxidative properties. These peptides have a strong effect on Cutibacterium acnes (C. acnes) and significantly inhibit Staphylococcus aureus. The inhibition rate of biofilm adhesion of YT-EPs to C. acnes reached 50% under the MIC. It was found that YTCY-EPs possess strong antioxidant and anti-inflammatory properties. It can effectively reduce active oxygen nearly 3 times and can reduce the downstream TLR2/NF-κB and MAPKs/AP-1 pathways by regulating the nuclear translocation of NF-κB and AP-1 in vitro. The transcriptional expression of inflammatory cytokines, inflammatory chemokines, and matrix metalloproteinase genes is also regulated, thereby slowing the recruitment of inflammatory cells and the development of inflammation, and increasing keratinocyte mobility. In addition, the expression levels of inflammatory factors and matrix metalloproteinases in the rabbit ears with acne problems that were tested with YTCY-EPs were significantly reduced, and it was obviously observed that the rabbit ear inflammation, acne, and keratinization problems were repaired. The results of this study prove that YTCY-EPs can be used as a potential anti-acne raw material in cosmetics.












Similar content being viewed by others
Data Availability
The data presented in the study is available in the article.
References
Harris-Tryon TA, Grice EA (2022) Microbiota and maintenance of skin barrier function. Science 376(6596):940–945. https://doi.org/10.1126/science.abo0693
Mary Hannah Swaney LRK (2022) Living in your skin: microbes, molecules, and mechanisms. Infect Immun 89(4):20. https://doi.org/10.1128/IAI.00695-20
Dréno B, Pécastaings S, Corvec S, Veraldi S, Khammari A, Roques C (2018) Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol 32(S2):5–14. https://doi.org/10.1111/jdv.15043
Mayslich C, Grange PA, Dupin N (2021) Cutibacterium acnes as an opportunistic pathogen: an update of its virulence-associated factors. Microorganisms 9(2):303
Sanford JA, O’Neill AM, Zouboulis CC, Gallo RL (2019) Short-chain fatty acids from cutibacterium acnes activate both a canonical and epigenetic inflammatory response in human sebocytes. J Immunol 202(6):1767–1776. https://doi.org/10.4049/jimmunol.1800893
Lim H-J, Kang S-H, Song Y-J, Jeon Y-D, Jin J-S (2021) Inhibitory effect of quercetin on propionibacterium acnes-induced skin inflammation. Int Immunopharmacol 96:107557. https://doi.org/10.1016/j.intimp.2021.107557
Cong T-X, Hao D, Wen X, Li X-H, He G, Jiang X (2019) From pathogenesis of acne vulgaris to anti-acne agents. Arch Dermatol Res 311(5):337–349. https://doi.org/10.1007/s00403-019-01908-x
Jugeau S, Tenaud I, Knol AC, Jarrousse V, Quereux G, Khammari A et al (2005) Induction of toll-like receptors by Propionibacterium acnes. Br J Dermatol 153(6):1105–1113. https://doi.org/10.1111/j.1365-2133.2005.06933.x
Salminen S, Collado MC, Endo A, Hill C, Lebeer S, Quigley EMM et al (2021) The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol 18(9):649–667. https://doi.org/10.1038/s41575-021-00440-6
Cuevas-González PF, Liceaga AM, Aguilar-Toalá JE (2020) Postbiotics and paraprobiotics: from concepts to applications. Food Res Int 136:109502. https://doi.org/10.1016/j.foodres.2020.109502
Cabello-Olmo M, Araña M, Urtasun R, Encio IJ, Barajas M (2021) Role of postbiotics in diabetes mellitus: current knowledge and future perspectives. Foods 10(7):1590
Salva S, Kolling Y, Ivir M, Gutiérrez F, Alvarez S (2021) The role of immunobiotics and postbiotics in the recovery of immune cell populations from respiratory mucosa of malnourished hosts: effect on the resistance against respiratory infections. Front Nutr 8. https://doi.org/10.3389/fnut.2021.704868
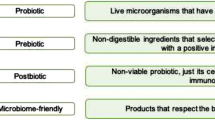
Tarrah A (2022) Probiotics, prebiotics, and their application in the production of functional foods. Fermentation 8(4):154
Pang J-H, Wong W-R, Hakozaki T, Yoshii T, Chen T-Y (2011) Up-regulation of tight junction-related proteins and increase of human epidermal keratinocytes barrier function by Saccharomycosis ferment filtrate. J Cosmet Dermatol Sci Appl 01(01):15–24. https://doi.org/10.4236/jcdsa.2011.11003
Takei K, Mitoma C, Hashimoto-Hachiya A, Takahara M, Tsuji G, Nakahara T et al (2015) Galactomyces fermentation filtrate prevents T helper 2-mediated reduction of filaggrin in an aryl hydrocarbon receptor-dependent manner. Clin Exp Dermatol 40(7):786–793. https://doi.org/10.1111/ced.12635
Hong Y-F, Lee Hy, Jung BJ, Jang S, Chung DK, Kim H (2015) Lipoteichoic acid isolated from Lactobacillus plantarum down-regulates UV-induced MMP-1 expression and up-regulates type I procollagen through the inhibition of reactive oxygen species generation. Mol Immunol 67(2):248–255. https://doi.org/10.1016/j.molimm.2015.05.019
Hye Rim K, Hangeun K, Bong Jun J, Ga Eun Y, Soojin J, Dae KC (2015) Lipoteichoic acid isolated from lactobacillus plantarum inhibits melanogenesis in B16F10 mouse melanoma cells. Mol Cells 38(2):163–170. https://doi.org/10.14348/molcells.2015.2263
Chen J, Cai J, Lin J, Cheng Z, Long M (2023) Inhibitory effects of bacillus coagulans TL3 on the ileal oxidative stress and inflammation induced by lipopolysaccharide in rats. Curr Microbiol 80(2):84. https://doi.org/10.1007/s00284-022-03171-2
Wang Y, Lin J, Cheng Z, Wang T, Chen J, Long M (2022) Bacillus coagulans TL3 inhibits lps-induced caecum damage in rat by regulating the TLR4/MyD88/NF-κB and Nrf2 signal pathways and modulating intestinal microflora. Oxid Med Cell Longev 2022:5463290. https://doi.org/10.1155/2022/5463290
Majeed M, Majeed S, Nagabhushanam K, Lawrence L, Arumugam S, Mundkur L (2020) Skin protective activity of lactosporin-the extracellular metabolite from bacillus coagulans MTCC 5856. Cosmetics 7(4):76
Majeed M, Majeed S, Nagabhushanam K, Mundkur L, Rajalakshmi HR, Shah K et al (2020) Novel topical application of a postbiotic, lactosporin®, in mild to moderate acne: a randomized, comparative clinical study to evaluate its efficacy, tolerability and safety. Cosmetics 7(3):70
Endres JR, Clewell A, Jade KA, Farber T, Hauswirth J, Schauss AG (2009) Safety assessment of a proprietary preparation of a novel probiotic, bacillus coagulans, as a food ingredient. Food Chem Toxicol 47(6):1231–1238. https://doi.org/10.1016/j.fct.2009.02.018
Zhang Y, Wang D, Fu H, Zhao D, Zhang J, Li M et al (2022) Protective effects of extracellular proteins of Saccharomycopsis fibuligera on UVA-damaged human skin fibroblasts. J Funct Foods 88:104897
Li X, Xiao Yu, Huang C, Cao R, Li J, Zhu G (2021) Study on the ability of ambroxol combined with levofloxacin to inhibit and clear Klebsiella pneumoniae biofilm. Chin Clin Pharmacol Ther 26(10):1103
Yang S, Jiang Y, Yu X, Zhu L, Wang L, Mao J et al (2021) Polyphyllin I inhibits propionibacterium acnes-induced IL-8 secretion in HaCaT cells by downregulating the CD36/NOX1/ROS/NLRP3/IL-1β pathway. Evidence-Based Compl Altern Med 2021:1–11
Ciulla MG, Gelain F (2023) Structure–activity relationships of antibacterial peptides. Microb Biotechnol 16(4):757–777
Zhang H, Tang W, Wang Li, Qian H, Qi X (2013) Research progress on structure-activity relationship of antioxidant peptides. J Food Biotechnol 32(7):673–679
Xiaoqian Xu, Pradhan S, Yuping Ran (2021) Research progress on the interaction mechanism of acne-related microbiota. Chin J Dermatol Venereol 35(02):222–227. https://doi.org/10.13735/j.cjdv.1001-7089.202002153
Coenye T, Spittaels K-J, Achermann Y (2022) The role of biofilm formation in the pathogenesis and antimicrobial susceptibility of Cutibacterium acnes. Biofilm 4:100063. https://doi.org/10.1016/j.bioflm.2021.100063
de Souza GS, de Jesus SL, Mundim ACS, de Miranda MJ, Sales-Campos H, Lorenzón EN (2022) Antimicrobial-wound healing peptides: Dual-function molecules for the treatment of skin injuries. Peptides 148:170707
Gera S, Kankuri E, Kogermann K (2022) Antimicrobial peptides–unleashing their therapeutic potential using nanotechnology. Pharmacol Ther 232:107990
Yang C, Luo L, Bai X, Shen K, Liu K, Wang J et al (2020) Highly-expressed micoRNA-21 in adipose derived stem cell exosomes can enhance the migration and proliferation of the HaCaT cells by increasing the MMP-9 expression through the PI3K/AKT pathway. Arch Biochem Biophys 681:108259
Lee H, Hwang D, Lee M, Lee J, Cho S, Kim T-J et al (2022) Micro-current stimulation suppresses inflammatory responses in peptidoglycan-treated raw 264.7 macrophages and Propionibacterium acnes-induced skin inflammation via TLR2/NF-κB signaling pathway. Int J Mol Sci 23(5):2508
Cao J, Xu M, Zhu L, Xiao S (2023) Viaminate ameliorates Propionibacterium acnes-induced acne via inhibition of the TLR2/NF-κB and MAPK pathways in rats. Naunyn-Schmiedeberg’s Archives Pharmacol 1–14
Author information
Authors and Affiliations
Contributions
Yongtao Zhang, Yanbing Jiang,Jingsha Zhao and Qiuting Mo participated in the experiments of this study. Yongtao Zhang participated in the processing, analysis and visualization of the experimental results. Yongtao Zhang completed the writing of the article. Meng Li and Dongdong Wang participated in the revision of the article. Changtao Wang and Meng Li provided research funding for the research. All authors reviewed and approved the submission of this article.
Corresponding author
Ethics declarations
Ethical Approval
All animal experiments were authorized by the Institutional Animal Care and Use Committee (IACUC) at ZHBY Biotech Co., Ltd. The approval number was SCXK (Jing) 2019–0010. This study fully considers the interests of animals, treat animals kindly, prevent or reduce the stress, pain, and injury of animals, respect the lives of animals, stop barbaric behaviors against animals, and adopt the least painful method to deal with animals; experimental animal projects guarantee the safety of practitioners; the methods and purposes of animal experiments are in line with human moral and ethical standards and international practices.
Consent for Publication
All authors have read and approved the final manuscript.
Competing Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Jiang, Y., Zhao, J. et al. Weizmannia coagulans Extracellular Proteins Reduce Skin Acne by Inhibiting Pathogenic Bacteria and Regulating TLR2/TRAF6-Mediated NF-κB and MAPKs Signaling Pathways. Probiotics & Antimicro. Prot. (2023). https://doi.org/10.1007/s12602-023-10175-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12602-023-10175-2